Background and Objectives: Demographic trends show an increasing older adult population. Therefore, family medicine training programs may need to reevaluate how well their residents perform clinic procedures essential to older adults. Our objective was to compare the rates of the most frequently performed clinic procedures for Medicare patients in a large multiregional health care system (MRHCS) with those in a family medicine residency clinic.
Methods: In this retrospective cohort study, Current Procedural Terminology coding data were queried from the billing systems of an MRHCS (the control group) and a family medicine residency clinic (the study group) for a 3-year period. The primary outcome was the procedural rate ratios per 1,000 office visits for the 10 most common clinic procedures in the MRHCS billed to Medicare.
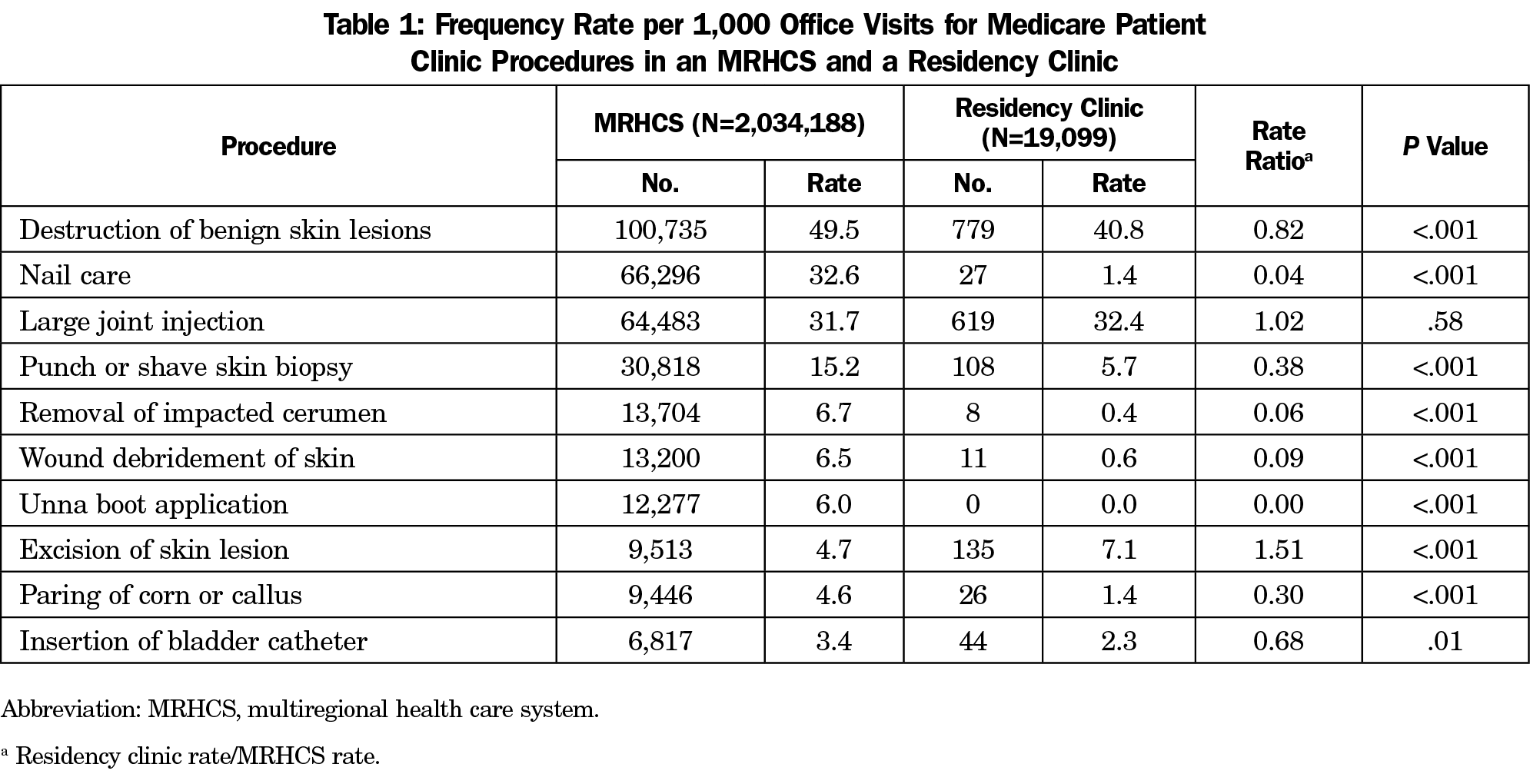
Results: The study group consisted of 19,099 office visits by Medicare patients to the residency clinic; the control group consisted of 2,034,188 visits to the MRHCS. Except for large joint injection, procedural rates were significantly different for the other nine procedures (destruction of benign skin lesions, nail care, punch or shave skin biopsy, removal of impacted cerumen, wound debridement of skin, Unna boot application, excision of skin lesion, paring of corn or callus, and insertion of bladder catheter). The rate of skin excision was higher in the residency clinic than in the MRHCS but lower for the other eight procedures.
Conclusions: These data suggest that teaching programs may need to adapt to meet the current and future practice needs of this increasing patient population.
According to the US Census Bureau’s 2017 national population projections,1 the percentage of Americans aged 65 years or older will increase from 15% in 2016 to 21% in 2030. The US medical education system is preparing a new generation of physicians who must address the needs of future patient populations, but a critical issue is that family medicine residency training may not meet the needs of those future patients and health care employers.2 As the number of Medicare patients grows, so will the need to ensure that residency programs across the country are adequately training new physicians to perform clinic procedures essential to older adults.
A spectrum of practice patterns exists in primary care. At one end of the spectrum, the family physician follows the traditional path of providing comprehensive care as an individual. At the other end, the physician serves as the coordinator of medical services on a team of health care providers that often includes medical, surgical, mental health, and rehabilitation specialists, all providing ongoing care. Comprehensive primary care can be defined as evaluation, management, and procedural services for a wide range of common health conditions resulting in less care by specialists. Bazemore et al3 examined a large sample of Medicare patients and showed a correlation between increasing comprehensiveness of primary care and decreasing Medicare costs. In an analysis of data from the 2016 National Family Medicine Graduate Survey4 of new family physicians, Peterson et al2 found that residents were highly interested in providing a broad spectrum of care, and their training generally matched that interest; however, surveys of actual practice patterns 1 year later highlighted a more limited scope with fewer procedures. Those studies examined broad categories of care (eg, obstetrics, emergency care, and “ambulatory procedures, skin”) rather than specific clinic procedures.
The 2018 Accreditation Council for Graduate Medical Education requirements for procedural training in family medicine residencies state, “Residents must be able to competently perform all medical, diagnostic, and surgical procedures considered essential for the area of practice,” but the family medicine program director and faculty must determine which procedures are essential on the basis of “current practices of program graduates, national data regarding procedural care in family medicine, and the needs of the community to be served.”5 To provide direction on which procedures should be considered essential, the Society of Teachers of Family Medicine (STFM) has compiled a list of more than 40 procedures that family medicine residents should be taught.6 A requisite number of performed procedures is not specified because the number performed to achieve competence depends on the complexity of the procedure and the capabilities of the learner.
A search of the medical literature identified few studies that investigated this issue. In addition to the STFM list, another survey of expert opinion from Australia provides a comprehensive list of procedures for family medicine residency training.7 However, achieving this recommended ideal is challenging in the current residency education environment, with competing pressures of inpatient, outpatient, and emergency department training; obstetrics training; work-life balance requirements; and documentation demands. To more precisely match the needs of future patient populations, a smaller, focused set of basic clinic procedural proficiencies may be identified from studies of actual practice.
The objective of the present study was to compare the rates of the most frequently performed clinic procedures for Medicare patients in a large multiregional health care system (MRHCS) with those in a family medicine residency clinic.
The study period of this retrospective cohort study began January 1, 2014, and ended January 1, 2017. The study group was composed of all Medicare patients who visited a residency clinic (Mayo Family Clinic Kasson in Kasson, Minnesota). The control group was composed of all Medicare patients who visited providers at a large MRHCS with sites in the Upper Midwest, Arizona, and Florida. The tertiary care facility in Rochester, Minnesota, was excluded because the care provided there often involves rare conditions and second or third opinions, rather than primary care of the geriatric population.
Billing records were queried for all Current Procedural Terminology (CPT) coding data for both groups during the study period. The list of 2,500 CPT codes in descending order by quantity billed to Medicare was reviewed to identify the 10 most common office procedures in the control group during the study period; those procedures served as the comparison procedures. Many codes were listed multiple times in this report because some billing systems within the MRHCS reported the data differently. Code quantities were combined as follows when they represented the same or similar procedures: 17000, 17003, 17004, 17110, and 17111 for destruction of benign skin lesions; 11719, 11721, and G0127 for nail care; 20610 for large joint injection; 11100, 11101, and 11300 through 11313 for punch or shave skin biopsy; 69210 for removal of impacted cerumen; 11042 and 97597 for wound debridement of skin; 29580 and 29581 for Unna boot application; 11400 through 11446, 11600 through 11646, and 12031 through 12052 for excision of malignant and benign skin lesions, including intermediate repairs; 11055 and 11056 for paring of corn or callus; and 51701 and 51702 for insertion of bladder catheter.
Procedural rates were calculated by dividing the number of procedures by the total number of evaluation, management, and preventive codes (office visits) in the respective groups to yield the rate of procedures per 1,000 office visits. Total Medicare office visits were defined from the following CPT codes: 99211 through 99215, 99391 through 99397, 99201 through 99205, and 99381 through 99387. The primary outcome was the procedural rate ratios for the 10 most common Medicare clinic procedures in the control group.
For statistical analysis, it was assumed that the rates for individual procedures were statistically independent and that the sampled period was adequate for generalization. Procedural rates were compared with the χ2 test with a 2-tailed 95% confidence interval. Two-tailed P values were calculated with the Microsoft Excel (version 2010) CHIDIST function. Because this study was a quality improvement project, the Mayo Clinic Institutional Review Board determined that it did not require institutional review board review.
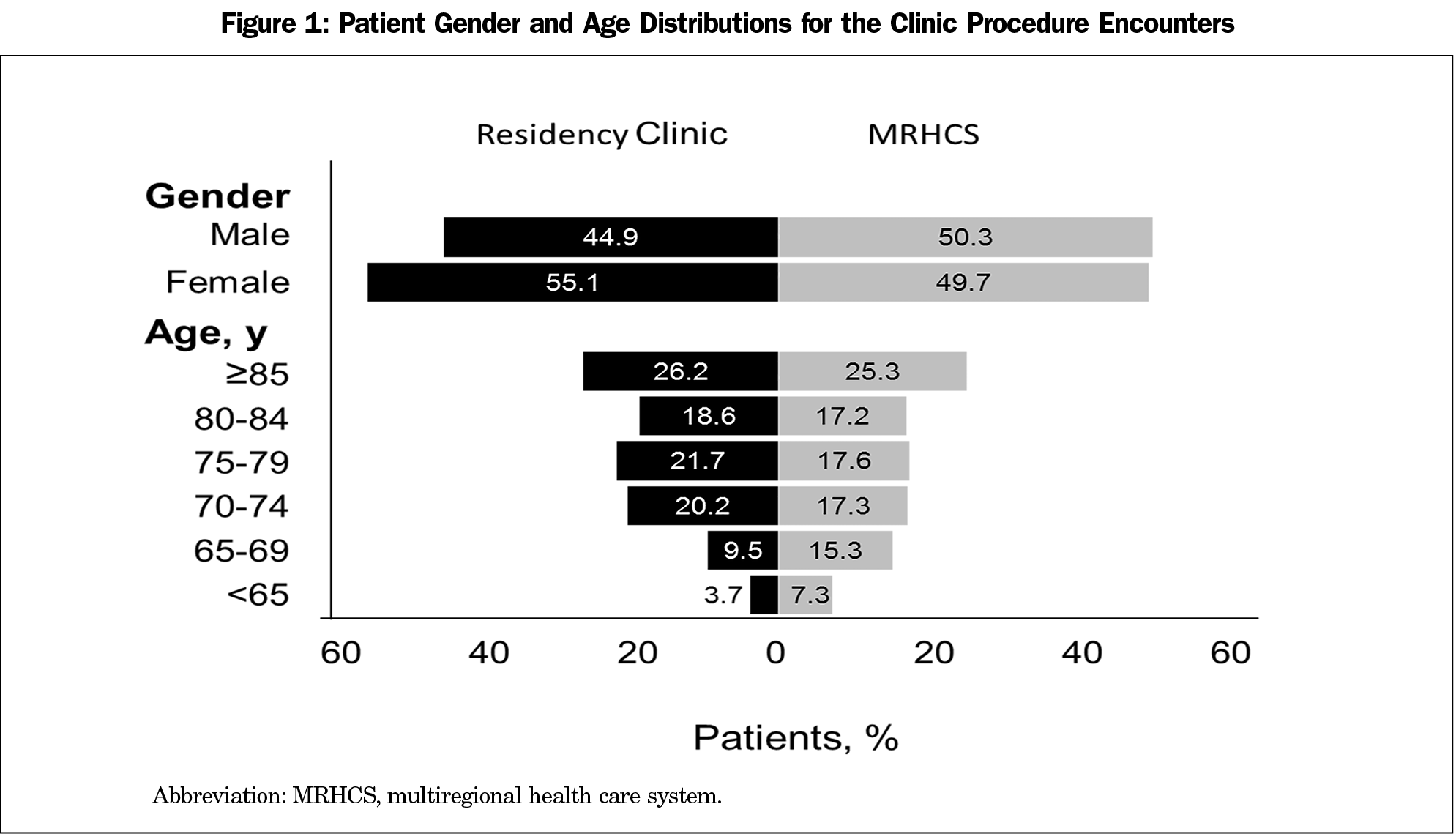
During the 3 years of the study, Medicare was billed for 2,034,188 office visits in the MRHCS and 19,099 in the residency clinic. As Figure 1 illustrates, there were no clinically meaningful differences in gender or age distributions for the encounters.
Except for the procedure of large joint injection, procedural rates were significantly different for the other nine procedures (Table 1). The rate of skin excision of malignant and benign lesions, including intermediate repairs, was significantly higher in the residency clinic than in the MRHCS (7.1 vs 4.7 per 1,000, P<.001). Rates for the other eight procedures were significantly lower in the residency clinic (Table 1).
In this study, quantitative billing data from a large MRHCS were used to identify actual procedural demand in a broadly representative Medicare population. When the procedural rates for the most common clinic procedures were compared with those at a family medicine residency clinic serving a similar population, 8 of the 10 most common office procedures in Medicare patients were performed at a lower rate in the residency clinic. This implies that the procedural training of family medicine residents may be inconsistent with their future practice patterns.
This study has several strengths. First, the analysis used billing records of procedures actually performed, which is more objective (and therefore presumably more accurate) than surveys of expert opinion or practice patterns. Second, we used a novel analytical method that can be easily adapted to other health care systems and residency clinics. Third, the use of billing data over a 3-year period yielded substantial sample sizes—the study group of more than 19,000 office visits was compared with a control group of more than 2 million visits. Fourth, this study included Medicare billing from all providers of the MRHCS (ie, primary care physicians, specialists, advanced practice providers, and nursing staff) to establish a comprehensive baseline need for clinic procedures in the Medicare population. This aligned with the purpose of the study, which was to investigate the comprehensiveness of family medicine residency education in the areas that matter most to Medicare patients.
This study has several potential weaknesses. First, the validity of these results depends on the accuracy of coding practices in the MRHCS and the residency clinic. However, coding accuracy is reviewed on a regular basis in this MRHCS, so that large-scale billing errors are unlikely. The residency clinic in this study was where residents in the residency program cared for their own panel of primary care patients; this clinic does not undergo coding review of outpatient billing, so that residents performing the procedures may not have accurately coded them. Second, residents rotate through sites other than their home clinic during the 36 months of residency. They currently spend 1 month in dermatology at an MRHCS site and 6 weeks at the Employee and Community Health Procedure Clinic, a part of the tertiary care facility that was excluded from this study; the residents can also use elective time to rotate with a podiatrist. Procedures performed during those rotations were not captured in the residency clinic billing data. Third, this MRHCS includes small rural branch clinics, suburban clinics in small to medium-sized cities, and small to medium-sized hospitals serving primary and secondary care functions, but it does not include a large urban population. Inclusion of Medicare billing data from poor, urban areas might change the ranked order of procedures performed, so these study results may not be applicable for that population.
Family medicine residents typically have approximately 1,650 to 2,200 outpatient clinic visits during their 36 months of training, and the residents may choose to focus on more complex or higher acuity needs rather than repeat simple office procedures in which they may already be competent. With the rapidly changing medical landscape, residents are being trained to work within care teams where members work at the maximal level of their licensure. Accordingly, cerumen removal and bladder catheter insertions were performed by nursing staff at this residency clinic. Furthermore, while residents may be encouraged to perform nail care, paring of corns or calluses, and wound debridement, a referral option exists within Mayo Clinic.
Medicare generally reimburses at a lower rate than most other insurers and payers. With the expected demographic increase in the geriatric population and the difficulties in transportation and mobility that come with advanced age, the likelihood increases that Medicare patients will lack adequate access to care in the coming decades. This growing need can be clearly seen and perhaps better anticipated by family medicine educators.
The eight procedures that were performed at a lower rate in the residency clinic in this study are relatively simple to learn. This is an encouraging finding, because those procedures can be incorporated into a routine residency clinic practice as needed by patients. The goal is for residents to achieve competence and confidence in these clinic procedures for Medicare patients. Later, physicians who want to delegate these responsibilities to allied health or nursing staff to improve efficiency will have the necessary experience to supervise more effectively.
An area that deserves further study is the effect of the setting in which residents learn procedures. When family physicians teach and learn procedures in a family medicine clinic, the unspoken message is that the standard of care includes family physicians performing these procedures. But it is unclear whether this same message is intended or received when the procedures are taught by a specialist in a specialty clinic. Therefore, it is possible that the setting in which a resident learns the procedure affects the resident’s comfort with performing that procedure in the future. If so, more emphasis should be placed on family medicine residents learning common outpatient procedures from family physicians in a family medicine clinic.
Comprehensiveness is a time-honored value in primary care, and recent evidence shows that it lowers Medicare costs. The older adult patient population is at risk in the coming decades because of demographic growth rates and lower reimbursement rates. This study has identified a potential gap in clinic procedural training between a family medicine residency clinic and outpatient clinical practice with Medicare patients. Creating a learning environment where comprehensive care is encouraged and modeled will likely result in graduates who are able and willing to deliver this type of care.
Acknowledgments
This study was presented as a poster at the North American Primary Care Research Group Annual Meeting, Chicago, Illinois, November 10, 2018. An oral presentation will be given at the Society of Teachers of Family Medicine Annual Meeting, Toronto, Ontario, April 27 - May 1, 2019.
References
- Vespa J, Armstrong DM, Medina L. Demographic Turning Points for the United States: Population Projections for 2020 to 2060. 2018:15. https://www.census.gov/content/dam/Census/library/publications/2018/demo/P25_1144.pdf. Accessed September 10, 2018.
- Peterson LE, Fang B, Puffer JC, Bazemore AW. Wide Gap between Preparation and Scope of Practice of Early Career Family Physicians. J Am Board Fam Med. 2018;31(2):181-182. https://doi.org/10.3122/jabfm.2018.02.170359
- Bazemore A, Petterson S, Peterson LE, Phillips RL Jr. More Comprehensive Care Among Family Physicians is Associated with Lower Costs and Fewer Hospitalizations. Ann Fam Med. 2015;13(3):206-213. https://doi.org/10.1370/afm.1787
- Weidner AKH, Chen FM, Peterson LE. Developing the National Family Medicine Graduate Survey. J Grad Med Educ. 2017;9(5):570-573. https://doi.org/10.4300/JGME-D-17-00007.1
- Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Family Medicine. 2018:38. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/120FamilyMedicine2018.pdf?ver=2018-06-15-112624-307. Accessed September 10, 2018.
- Nothnagle M, Sicilia JM, Forman S, et al; STFM Group on Hospital Medicine and Procedural Training. Required procedural training in family medicine residency: a consensus statement. Fam Med. 2008;40(4):248-252.
- Sylvester S, Magin P, Sweeney K, Morgan S, Henderson K. Procedural skills in general practice vocational training - what should be taught? Aust Fam Physician. 2011;40(1-2):50-54.



There are no comments for this article.