Background and Objectives: The rapid increase in the older adult population necessitates an increase in physicians who are adept at caring for the various medical comorbidities that accompany aging. To fill the gap in geriatric medical education and overcome barriers to medical student interest in geriatrics, we developed a friendly caller program that links medical students to older adults through multiple weekly phone calls. This study examines the impact of this program on geriatric care competency, a foundational skill for primary care physicians, in first-year medical students.
Methods: We used a mixed-methods design to measure how medical students’ self-assessed geriatric knowledge was impacted by their longitudinal interactions with seniors. We compared pre- and postsurvey data using a Mann-Whitney test. We used deductive qualitative analysis to examine themes that emerged from narrative feedback.
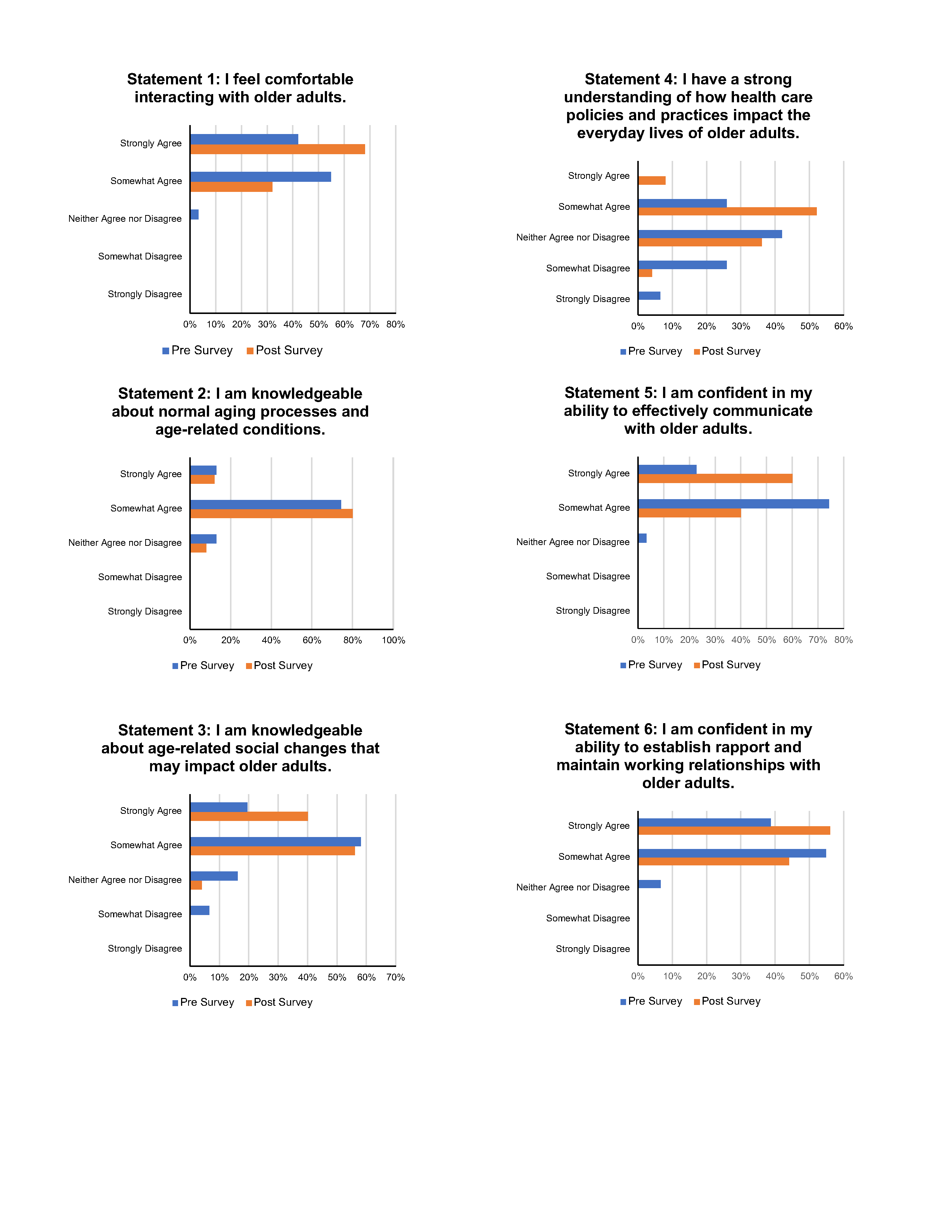
Results: Our results demonstrated that students (n=29) showed a statistically significant increase in components of their self-assessed geriatric care competency. Qualitative analysis of student responses revealed five common themes: transformation of preconceived notions regarding older adults, relationship building, greater understanding of older adults, communication skills, and self-compassion.
Conclusions: Given the shortage of physicians competent in geriatric care amid a rapidly growing older adult population, this study highlights a novel, older adult service-learning program that positively impacts geriatric knowledge in medical students.
Estimates from the US Census Bureau reveal that the nation’s 65-and-older population has risen by a third during the past decade. 1 This growth necessitates an increase in physicians who are trained to care for older adults. However, a significant shortage remains of primary care physicians who often provide care to older adults, as well as geriatricians, who represent only 1.9% of primary care providers. 2 This gap begins in medical training where students’ interest in family medicine is low, with only 8.1% of US allopathic medical students matching into family medicine in 2021. 3 This reality is coupled with an even lower geriatrics match rate, with 56% of the 2015 geriatric National Resident Matching Program fellowship positions unfilled. 4 Factors contributing to low interest in geriatrics include complexity of disease, low status, and lack of clinical exposure. 5
However, studies have found that these issues can be overcome with adequate education and experience. 5
Medical training has incorporated a variety of educational strategies to increase interest in geriatrics. For example, third-year medical students who participated in an in-home elective reported greater insight into geriatrics. 6 Other studies have demonstrated that interest in geriatrics increased following a home visit. 7 However, little data examine the role of longitudinal, preclinical exposure to older adults using phone calls. Thus, our medical school developed a geriatric service-learning project that paired medical students with older adults via weekly phone calls for 6 weeks. With the upsurge of online learning in medical education, assessing how remote learning models impact students’ interest in geriatrics and filling the gap in older adult medical education are important. We hypothesized that after participation in this program, first-year medical students would report higher levels of geriatric care competency.
We recruited first-year medical students using a form emailed to the class (see Table 1 for demographic makeup of student population). We recruited older adults through invitation by housing site coordinators in low-income housing, as well as through word of mouth by family and friends (see Table 2 for demographic makeup of older adult population).
|
Demographic
characteristics
|
N=29
(%)
|
|
Age
(in year)
|
|
20-24
|
18 (62.0)
|
|
25-29
|
10 (34.5)
|
|
30-34
|
1 (3.4)
|
|
Gender
|
|
Male
|
10 (34.5)
|
|
Female
|
19 (65.5)
|
|
Race/ethnicity
|
|
White
|
13 (44.8)
|
|
Black
|
0 (0)
|
|
Hispanic
|
1 (3.4)
|
|
Asian
|
15 (51.7)
|
|
Demographic
characteristics
|
N=29
(%)
|
|
Age
(in years)
|
|
65-69
|
1 (3.4)
|
|
70-74
|
11 (37.9)
|
|
75-79
|
4 (13.7)
|
|
80-84
|
2 (6.8)
|
|
85-89
|
2 (6.8)
|
|
90-104
|
4 (13.8)
|
|
Unknown
|
5 (17.2)
|
|
Gender
|
|
Male
|
6 (20.6)
|
|
Female
|
23 (79.3)
|
|
Race/ethnicity
|
|
White
|
17 (58.6)
|
|
Black
|
1 (3.4)
|
|
Hispanic
|
1 (3.4)
|
|
Other
|
10 (34.4)
|
|
Housing
|
|
Live alone
|
24 (82.7)
|
|
Live with spouse
|
2 (6.8)
|
|
Live with child
|
1 (3.4)
|
|
Other
|
2 (6.8)
|
Students watched a 45-minute training video involving an overview of active listening skills, mindfulness practice, and reporting guidelines for elder abuse and suicidal ideation. Students completed a presurvey and were paired with an adult age 65 or older. Students were encouraged to call their older adult three times a week, speaking for at least 20 minutes per call, over 6 weeks across the months of April and May 2020. The objective of the calls was to engage in meaningful conversation and thereby combat social isolation.
For these open-ended conversations, students were provided with a framework that included questions such as, “What brings you joy? What is important to you? What would make tomorrow a good day?” Additionally, students participated in weekly, 1-hour, faculty-facilitated debriefing sessions about their encounters. At the conclusion of the program, students received a certificate of appreciation and completed a postsurvey. The survey questioned students’ understanding of and comfort working with older adults. The study was reviewed by the USC Institutional Review Board and approved as exempt: Keck IRB UP-21-00488, Grant Number U1QHP28740. Funding was provided through HRSA GWEP.
We used a mixed-methods design to measure how students were impacted by their interactions with older adults. Using a Likert-scale in the surveys, we were able to assess students’ knowledge of older adults and geriatric care competency. We analyzed the quantitative data using a Mann-Whitney nonparametric test. We used an internally developed scale to obtain a more generalizable measure regarding students’ comfort working with older adults. While the UCLA Geriatrics Attitude scale is a validated instrument we could have used, it was not developed to study medical students.
We gathered narrative participant feedback during debriefing sessions as well as from short-answer survey questions. For our thematic analysis, we had two independent reviewers perform coding, which involved reading transcripted notes and survey answers, followed by identifying common themes. To increase objectivity and validity of our analysis, a third coder collaborated to arrive at agreed-upon themes that embodied responses.
Among the 29 students enrolling in and completing the program, self-reported duration of calls ranged from 20 to 60 minutes, three to five times per week. Deductive analysis of student debriefing sessions and surveys revealed the five themes shown in Table 3. The most common themes were transforming preconceived notions of older adults, relationship building, greater understanding of older adults, and communication skills. The fifth theme, self-compassion, was the least cited.
|
Themes
|
Quotations
|
|
Transforming preconceived notions of older adults (n=18)
|
“Older adults can live extremely productive lives. My older adult was busier than most people I know, even at her age.” “Older adults are not so different from younger adults, and many of the common misconceptions about aging do not apply.”
|
|
Relationship building (n=15)
|
“This is a different friendship than I ever expected to have. It is such a deep connection. I can’t believe I have a friendship with someone 60 years older than me. She gives me such a different perspective on life.” “I started this thinking that it was for the older adult, and I’ve learned much more about me. It’s helped me understand how connections are made with people over years and how deep bonds are formed—a delight!”
|
|
Greater understanding of older adults and the challenges they face (n=10)
|
“I am learning more about how transitions in life impact older adults—mobility, social isolation, memory, and such. I learned a lot from listening to other students experiences with their older adults, including ones that were challenging and needy.” “I have seen how social connections of family and friends can greatly benefit an older patient’s overall health.”
|
|
Communication skills (n=7)
|
“I’ve learned how to connect with a random stranger for hours over the phone and how to communicate over the phone.” “I’ve had a glimpse into what telehealth may be like, and I’ve learned how you can have both a personal and professional relationship with someone. From this experience, I am more likely to work with older adults in the future.”
|
|
Self-compassion (n=2)
|
“I’ve learned about putting boundaries on people for my own wellness.” “I need to learn how to meditate, and I need to learn better self-care.”
|
Responses to pre- and postsurveys are displayed in Figure 1. Analysis with the Mann-Whitney test revealed statistically significant differences (P<.05) between survey results for three statements (Table 4).
|
Statement
|
U
|
z score
|
P value
|
|
I feel comfortable interacting with older adults.
|
282.5
|
-1.72
|
.085
|
|
I am knowledgeable about normal aging processes and age-related conditions.
|
374.0
|
-0.21
|
.833
|
|
I am knowledgeable about age-related social changes that may impact older adults (eg, retirement, loss of a romantic partner, relocation).*
|
266.5
|
-1.99
|
.046
|
|
I have a strong understanding of how health care policies and practices impact the everyday lives of older adults.*
|
207.5
|
-2.96
|
.003
|
|
I am confident in my ability to effectively communicate with older adults.*
|
237.5
|
-2.46
|
.013
|
|
I am confident in my ability to establish rapport and maintain working relationships with older adults.
|
309.5
|
-1.28
|
.201
|
This service-learning project represents an innovative way to incorporate learning about geriatrics into medical education. While traditional geriatric curricula provide exposure via classroom lectures or standardized patients, this educational innovation allowed students to delve into the nuances of aging through phone calls, similar to telemedicine. This opportunity to provide connection and whole-person care to older adults is both unique and invaluable in medical education.
Thematic analyses revealed that students learned clinical skills within and beyond the field of geriatrics. For example, relationship building, the second most-cited theme, was attributed to high job satisfaction in working in geriatrics. 8 Additionally, the themes of transformation of preconceived notions and greater understanding of older adults are powerful findings because lack of exposure and negative perceptions of older adults are barriers to students pursuing geriatrics. 5 Furthermore, communication skills and self-compassion are critical clinical skills for future primary care physicians. Students found tools and methods not only for overcoming generational gaps but also for practicing establishing professional boundaries and caring for oneself in the process of caring for others.
Our findings confirm our hypothesis and demonstrate that a friendly caller program with older adults increases self-assessed geriatric care competency and awareness of older adult health issues. While the Association of American Medical Colleges (AAMC) established geriatric competencies for medical students, those requirements do not require students to demonstrate understanding of normal aging or age-related social changes—skills critical in recognizing how pathologies like depression and dementia manifest in older adults. 9 Additionally, AAMC competencies include discussions of code status, but those are meaningful conversations only when physicians can effectively communicate with older adults. 9 Furthermore, numerous health policy issues relevant to older adults are not addressed in medical education but remain important to the training of health care leaders who will care for the older adult population. Thus, novel training programs with older adults are critical to preparing our future health care workforce.
Our study has several limitations. First, the older adults generally were healthy and participatory in conversations, which is not reflective of institutionalized patients that medical students encounter in practice. Further limitations include small sample size, lack of control group, and selection bias. That is, students in this program likely had greater interest in older adult care than the average medical student population. Despite these limitations, this study is an example of how a remote, service-learning caller program can be impactful in increasing geriatric care competency in medical students. Future iterations of this study should implement a follow-up survey to assess how these findings influence the likelihood of working with older adults or matching into geriatric fellowships. Given the deficiency in the number of geriatricians and primary care providers, pipeline efforts are essential. This study highlights how early exposure to older adults positively influences medical student attitudes toward this patient population and may be critical to reversing this gap in care.
References
- U.S. Census Bureau. 65 and older population grows rapidly as baby boomers aga. Accessed July 25, 2022. https://www.census.gov/newsroom/press-releases/2020/65-older-population-grows.html
-
van Zuilen MH, Granville LJ. Playing the long game: Addressing the shortage of geriatrics educators.
J Am Geriatr Soc. 2019;67(4):647-649.
doi: 10.1111/jgs.15901
-
David AK. Matching 25% of medical students in family medicine by 2030: realistic or beyond our reach?
Fam Med. 2021;53(4):252-255.
doi: 10.22454/FamMed.2021.982403
-
Advisory Board. Why America faces a geriatrician shortage (and what to do about it). January 21, 2020. Accessed July 25, 2022. https://www.advisory.com/daily-briefing/2020/01/21/geriatricians
-
Lester PE, Dharmarajan TS, Weinstein E. The looming geriatrician shortage: ramifications and Solutions.
J Aging Health. 2020;32(9):1052-1062.
doi: 10.1177/0898264319879325
-
Meiboom AA, de Vries H, Hertogh CM, Scheele F. Why medical students do not choose a career in geriatrics: a systematic review.
BMC Med Educ. 2015;15(1):101.
doi: 10.1186/s12909-015-0384-4
-
Nagle BJ, Berry A, Gorman L, Dangiolo M. A preliminary qualitative evaluation of an in-home geriatric care elective experience for third-year medical students.
Cureus. 2018;10(4):e2415.
doi: 10.7759/cureus.2415
-
Goldlist K, Beltran CP, Rhodes-Kropf J, Sullivan AM, Schwartz AW. Out of the classroom, into the home: medical and dental students’ lessons learned from a geriatrics home visit.
J Am Geriatr Soc. 2022;70(9):2659-2665.
doi: 10.1111/jgs.17968
-
Leigh JP, Tancredi DJ, Kravitz RL. Physician career satisfaction within specialties.
BMC Health Serv Res. 2009;9(1):166.
doi: 10.1186/1472-6963-9-166



There are no comments for this article.