Background and Objectives: There is a persistent shortage of primary care physicians in the United States. Medical schools can help meet societal primary care health needs by graduating more students who select family medicine and other primary care careers. The objective of this narrative review was to evaluate the relationship between clerkships and primary care specialty choice.
Methods: We conducted a systematic literature search and narrative review of research articles examining the association between clerkships and primary care specialty choice. We evaluated the quality of included articles using a validated scale, assessed for methodology and outcomes, and synthesized using a narrative approach.
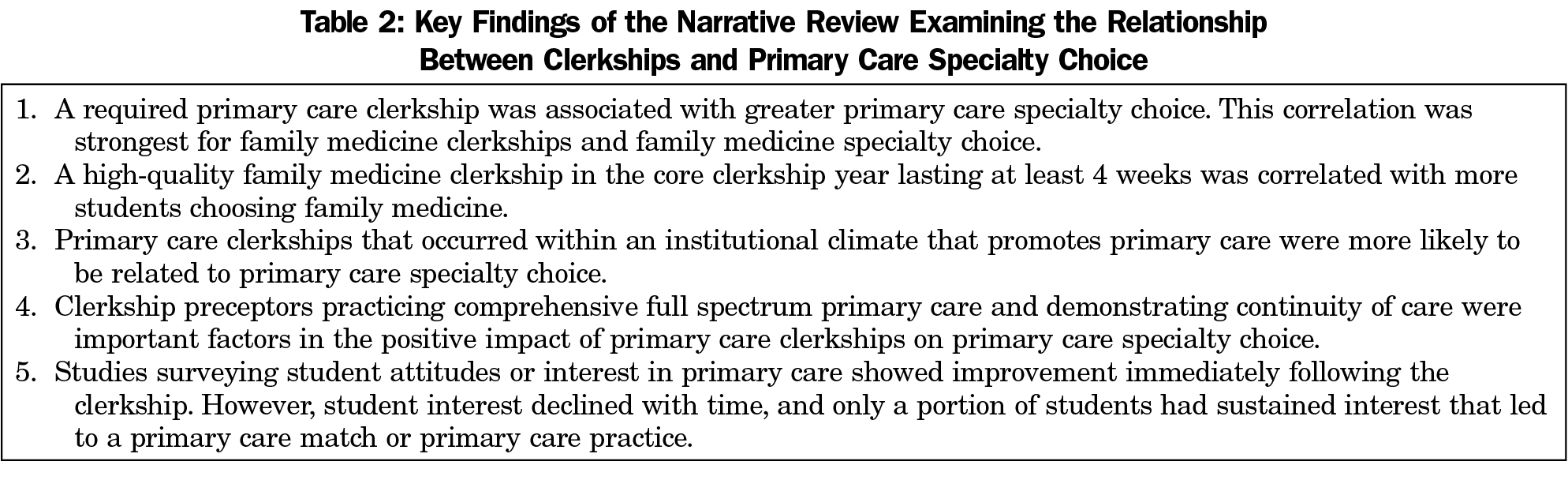
Results: We identified 59 articles meeting our research criteria. A required primary care clerkship in the core clerkship year was associated with increased primary care specialty choice. This finding was strongest for family medicine clerkships and family medicine specialty choice. Clerkships that were longer, were of higher quality, exposed students to a wider scope of primary care practice, and occurred within an institutional climate supportive of primary care were also correlated with more students choosing a primary care specialty. While student self-reported interest in primary care often increased following a primary care clerkship, this interest was not always sustained or consistently associated with a primary care residency match or primary care career.
Conclusions: Required family medicine and primary care clerkships were correlated with primary care specialty choice. More high-quality research is needed to better understand how to maximize the impact of clerkships on primary care specialty choice.
The scarcity of primary care physicians in the United States is worsening, with a projected shortage of up to 48,000 primary care physicians by the year 2034 contributing to a consequential negative impact on the health of the public.1 Although the recommended optimal percentage of primary care physicians for a health care system is 40% or greater,2,3 the percentage in the United States is currently only 30%, far lower than any other high-functioning wealthy democracy.4 As part of the solution to meet society’s needs, and to address health inequities, medical schools must graduate more students planning a primary care career in family medicine, general internal medicine, or pediatrics.5
Although many factors affect career choice, a required clerkship in family medicine or primary care has been established as a key educational intervention.6-8 Research demonstrating positive associations between family medicine clerkships and student choice of primary care led to widespread adoption of family medicine clerkships in US medical schools beginning in the 1970s and increasing over several decades. In the 2019-2020 academic year, 89% of medical schools in the United States and Canada had a required family medicine clerkship.9 Clinical experience in primary care and outpatient medicine are current requirements of the Liaison Committee on Medical Education (LCME), the accrediting body of medical schools in the United States and Canada.10
Previously published systematic reviews of primary care specialty choice have identified curriculum as an important factor.11-13 While some systematic reviews have commented on the positive impact of clerkships on primary care specialty choice,14,15 this study is the first comprehensive narrative review using a structured approach specifically focused on the relationship between clerkships and primary care specialty choice. In this review, we sought to synthesize evidence examining whether clerkships influence student choice of primary care, and what we can learn from the literature to help maximize the positive effects of clerkships.
We systematically searched and reviewed the existing literature using a narrative synthesis approach to explore whether clerkships were associated with primary care specialty choice.16 This methodology was chosen because the data set included heterogenous research methods and contexts. The Michigan State University Institutional Review Board determined this study to be non-human subjects research.
Data Retrieval
Articles in the topic area were obtained from those meeting inclusion criteria for the 2022 scoping review by Phillips et al examining the medical school structures, policies, and practices that promote primary care specialty choice.17 More keywords (“clerkship,” “preceptorship,” “ambulatory rotation,” “clinical rotation,” “primary care rotation”) were identified by mapping the language used in publications captured in the scoping review. Additional searches were conducted of Medline (PubMed), Education Resources Information Center (ERIC), Scopus, and CINAHL (EBSCO), using the search strategy developed by Phillips et al and augmented with the new keywords. We examined reference lists of all included articles to identify additional articles via citation chaining.
Article Selection
We developed inclusion and exclusion criteria prior to reviewing the search results. Inclusion criteria included peer reviewed, published research in English that described a required primary care clerkship in the clinical years, with outcomes including student attitudes toward primary care, interest in primary care, or specialty choice of primary care. We included articles from the United States, Canada, Australia, and New Zealand, because these countries have similar educational structures and workforce challenges. We did not limit the literature by year of publication. Studies were not excluded based on quality. Review articles were not included, but the citation lists of review articles were checked for additional articles.
In this narrative review we defined a clerkship as a required clinical experience or rotation conferring academic credit in the clinical years, typically the third and fourth year, lasting at least 10 full days. Some of the included articles used different terms to describe what we defined as a clerkship (eg, “rotation,” “preceptorship,” “attachment,” “ambulatory care experience”) and other excluded articles used the term “clerkship” but described elective courses or other experiences not meeting our definition. Articles describing longitudinal integrated clerkships and other required longitudinal rotations in the clinical years that met our inclusion criteria were included. The length of the preclinical and clinical phases of the curriculum (for example, 3-year vs 4-year programs) did not affect article inclusion, as long as the inclusion criteria were met.
We defined primary care as family medicine, general internal medicine, or pediatrics. Primary care specialty choice was defined as family medicine, general internal medicine, or pediatric practice; residency training or match to a residency in family medicine, general internal medicine, or pediatrics; student interest in primary care or family medicine; or student attitudes toward primary care or family medicine. Studies that solely evaluated interest or match in internal medicine or pediatrics without a general or primary care focus were not included.
Quality Evaluation
We evaluated the included articles using the quality assessment tool (QATSDD) developed by Sirriyeh et al18 utilizing the methodology described by Phillips et al.17 The 16-item tool has a maximum score of 48. Each included article was reviewed independently by two researchers (A.L.L. and D.R.E., both family physicians and medical educators) and quality ratings for each were averaged. When the researchers disagreed in their ratings by more than one standard deviation the article was reviewed for quality by both researchers together until consensus on the quality rating was reached. After completing the quality rating of the articles, we categorized articles into low, medium, and high quality, using QATSDD scores of 1-15, 16-24, and 25 or greater as criteria.
The primary scoping review search yielded 60 clerkship articles.17 Three articles were excluded because the full text was not obtainable, and two articles did not meet this study’s inclusion criteria, resulting in 55 included articles. A secondary search of the literature (July 2020) identified 265 additional articles. Of these, 218 were excluded based on title. Forty-seven abstracts were reviewed, and 33 were excluded. Fourteen full-text articles were reviewed and 12 were excluded. Two articles met inclusion criteria. A final search of the literature (June 2021) yielded one newly-published article meeting inclusion criteria. Citation chaining and review of bibliographies of published reviews yielded one additional article meeting inclusion criteria.
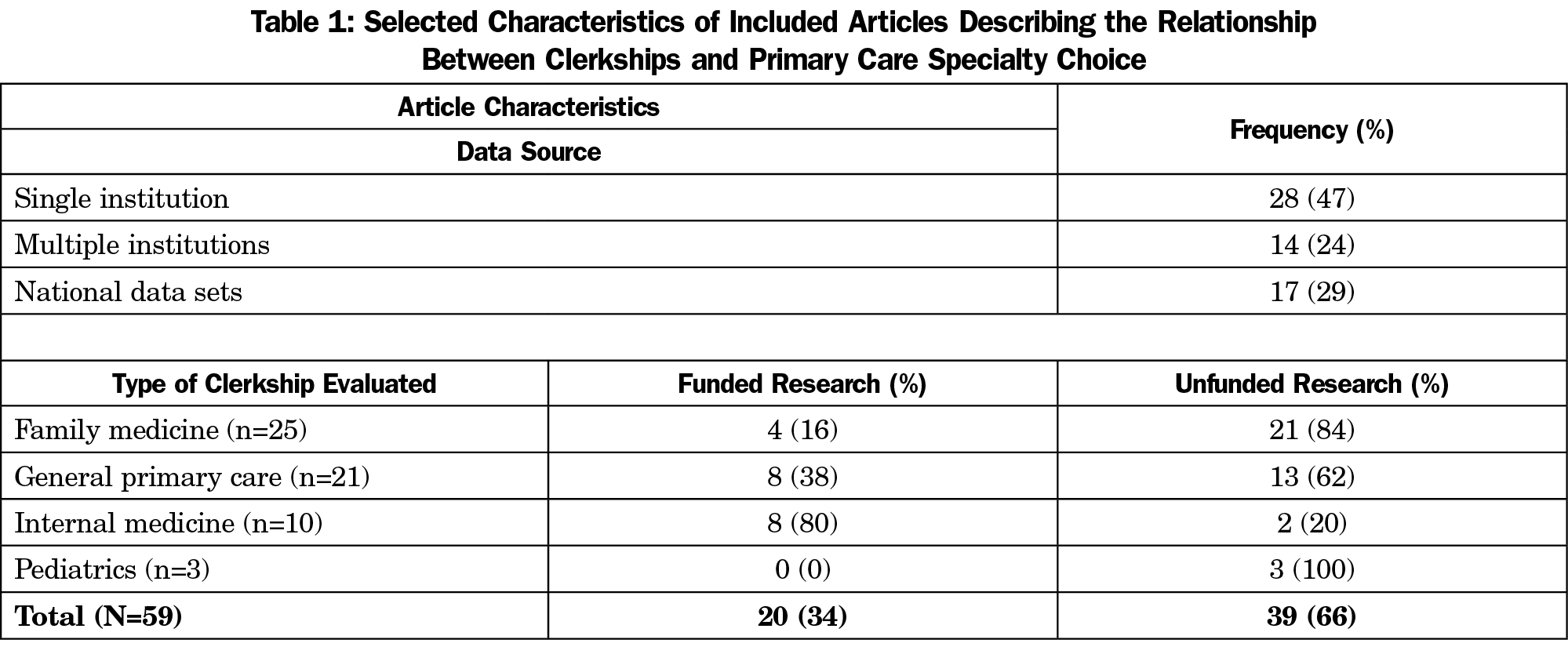
In total, 59 articles on clerkships met our inclusion criteria. The majority of included articles evaluated family medicine clerkships6,7,19-41 or general primary care clerkships,9,42-61 with 10 articles describing internal medicine clerkships62-71 and three articles about pediatrics clerkships72-74 meeting inclusion criteria. Article characteristics are further described in Table 1.
Article Quality, Methods, Outcomes, and Funding
The quality ratings varied dramatically among the papers, with the lowest-rated article receiving a score of 4 out of a maximum possible 48, and the highest rated article receiving a score of 37. Four papers were descriptive, without formal qualitative or quantitative analyses, and thus were not evaluated for quality. For 11 of the 59 articles, the independent quality ratings differed by more than 1 standard deviation, so a consensus quality rating was determined. Seventeen articles were of low quality, 16 were of medium quality, and 22 were of high quality. The most common journals were Academic Medicine and Family Medicine, each with 12 published articles.
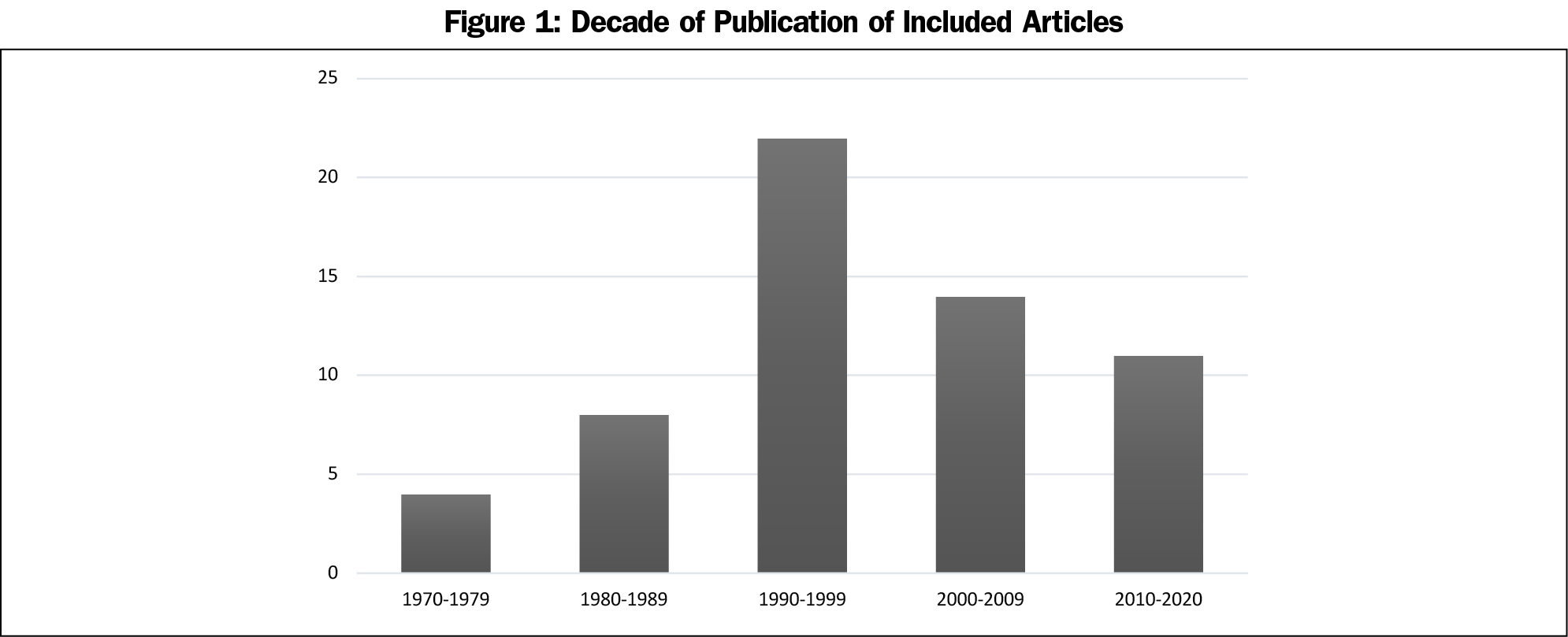
The literature on this subject slowly emerged in the 1970s and the number of papers peaked in the 1990s, concurrent with an increase in required primary care and family medicine clerkships. The number of studies then tapered off in the 2000s and beyond, as depicted in Figure 1. Over the last half century the quality of the research has evolved, with many earlier studies describing a single institution’s clerkship and using student self-reported attitudes about or interest in primary care as outcomes. Later studies were more likely to be multi-institutional or use national data sets and published match data. Table 2 presents a summary of key findings from the narrative review.
Forty-seven of the 59 included articles employed quantitative analysis, utilizing techniques ranging from descriptive comparisons of percentages, to simple t tests and χ2 tests, to complex multivariate analyses. Six articles utilized a qualitative approach and two used mixed methods. We observed several common types of methodologies in the included papers. Twelve papers used student self-report of interest in a primary care specialty as the outcome, using a survey to ask about primary care specialty interest before and after a clerkship, or asking students retrospectively to report on how a clerkship affected their specialty interest. Typically, these survey-based studies used unvalidated instruments, and the timing and anonymity of student responses was often unclear. Three articles surveyed medical school deans and faculty about the clerkships at their medical school and associated this information with published match data. Another seven articles used national data sets examining clerkships and published match results. Fourteen papers described asking primary care residents or practicing physicians to retrospectively evaluate the importance of a clerkship to their specialty choice.
Outcomes data regarding primary care specialty choice included a spectrum of reliability. This ranged from student self-report of attitudes toward, or interest in, a primary care specialty, to student self-reported specialty choice in the final medical school year, to published match data confirming primary care specialty choice, to studies of residents or physicians practicing in a primary care field.
Most papers did not report funding support for their research, as noted in Table 1. The 20 papers with funding described support from national agencies such as the Department of Health and Human Services, national and local foundations, and medical school departments. Eighty percent of the included internal medicine clerkship articles reported funding sources, primarily from the American Board of Internal Medicine Foundation. In contrast, only 16% of the included family medicine clerkship papers reported funding, and none of the included pediatric clerkship papers reported funding.
Clerkship Requirement
The large majority of included studies (86%) showed a positive association between required family medicine or primary care clerkships and primary care specialty choice. Two high-quality studies from the 1970s-1980s analyzed national data sets to evaluate the association between clerkships and specialty choice. Beck et al found that the 15 US medical schools in 1977 with a required family medicine clerkship had higher percentages of students choosing family medicine as a career.22 Similarly, Rabinowitz analyzed graduate questionnaires after students had chosen their specialties, finding that in 1988 the 20 schools with a required third-year family medicine clerkship had the highest percentage of students choosing family medicine as a career.6
In the 1990s, additional notable findings emerged. Campos-Outcalt and Senf determined that the US medical schools that implemented a required family medicine clerkship between 1984-1993 had increased family medicine match rates compared to control schools.27 In their retrospective survey of family medicine residents, Godkin and Quirk found that a required family medicine clerkship was rated as an important factor in the choice of family medicine as a specialty.33 A qualitative analysis by Musham and Chessman determined that students completing a required family medicine clerkship had an improved perception of family medicine, and negative stereotypes were dispelled.36 Overall, the literature consistently demonstrated that a required primary care clerkship was associated with increased student career choice of primary care.
Type of Clerkship
The research about the influence of primary care clerkships on primary care specialty choice most strongly supported an association between family medicine clerkships and family medicine specialty choice. The literature on internal medicine clerkships was mixed. Some studies found no association with primary care choice,49,71 while others found an increased interest in family medicine and pediatrics when an ambulatory component of the internal medicine clerkship was introduced.68,69 One entirely ambulatory internal medicine clerkship was associated with increased student interest in general internal medicine.70 The included pediatrics articles showed a positive association between the pediatric clerkship and pediatric specialty choice, but utilized outcomes of self-reported student interest in two of the three articles.72,73
Two studies of community-based longitudinal integrated clerkship (LIC) participants reported higher match rates in primary care compared to students in traditional block clerkships within the same institution.48,52 However, students selected the LIC option over the block option for clerkships in both of these institutions, and selection bias was noted by the authors as a limitation in interpreting these findings.
Clerkship Quality, Length, and Timing
Several studies found that higher perceived quality of a required primary care clerkship was correlated with greater primary care match rates.19,35,40,53,59,62,63 Clerkship length was also an important factor. A retrospective survey of family medicine residents compared to other residents found that the amount of medical school curriculum devoted to family medicine or primary care was an important factor in their specialty choice.28 Based on national US data from 2016, Wimsatt et al found that higher family medicine match rates were correlated with a family medicine clerkship of at least 4 weeks.41 Other studies reinforced the finding that a longer required family medicine clerkship was associated with higher family medicine match rates.24,25
Timing of the clerkship may also be important. In some national US studies that compared clerkship characteristics, the impact of a required primary care clerkship on specialty choice was found to be greater during the core clerkship year (commonly the third year) compared to the fourth year.6,47 Other studies found no difference between clerkships in the third or fourth year.24,56 One single-institution study of a required rural family medicine clerkship found that family medicine choice declined when the rotation was moved from the fourth year to the third year.32
Institutional Climate
Medical schools and health systems that prioritize and promote primary care had primary care clerkships that were more robustly related to student choice of a primary care specialty.8,22,41 Institutions that had more family medicine faculty teaching in the preclinical and clinical years, more senior family medicine faculty, and family medicine faculty in prominent administrative leadership positions were some specific aspects of institutional climate associated with a strong relationship between clerkships and choice of primary care.22,41 For an in-depth look at the impact of institutional climate, culture and structure on primary care specialty choice, see Seehusen et al.75
Clerkship Features
Within the clerkship, clinical exposure to comprehensive primary care and continuity of care was positively associated with family medicine specialty choice.8,28,40 Role modeling by high-quality primary care preceptors, particularly those who modeled a full scope of patient care, was also correlated with primary care choice.19,28,59,66
Clerkship Reinforcement
Notably, two studies found that student attitudes toward family medicine were enhanced immediately after the clerkship, but subsequently declined, possibly due to the influence of other rotations.32,39 Immediate postclerkship interest in primary care did not consistently result in a primary care match. The authors of each of these two studies suggested that having a required third-year family medicine clerkship followed by a required fourth-year reinforcing rotation may be important, although no conclusive studies have been conducted.
Primary care and family medicine clerkships were uncommon in the 1970s and 1980s, and were likely found only at medical schools with a serious commitment to primary care. By the 1990s, more medical schools had adopted primary care clerkships and the majority of research about the positive relationship between clerkships and primary care choice had been published. Yet even as primary care and family medicine clerkships became widespread over the last two decades, the number of US medical graduates choosing a primary care career has remained lower than physician workforce needs.9 It appears that primary care clerkships are necessary, but not sufficient on their own, to promote primary care choice.
Clerkships exist in the context of medical schools, health systems, and communities. It is likely that medical schools with higher quality and longer required primary care clerkships also provide a rich variety of additional curricular and extracurricular experiences in family medicine and primary care. These offerings reflect an institutional climate and culture that promotes primary care, from recruiting and admission of students likely to choose primary care; to early and repeated primary care experiences; to robust support, development, and promotion of primary care faculty.75 Clerkships also occur in communities and rely on community-based faculty with a commitment to education. All of these factors are interrelated and generate confounding, making the specific influence of clerkships difficult to isolate.
While several studies indicated that perceived higher-quality clerkships were associated with primary care career choice, little has been published about how to cultivate a high-quality clerkship experience. Specific curricular aspects of the clerkships, content and structure of didactic sessions, and types of preceptor practices have not been well studied with regard to primary care career choice. Some studies suggest that preceptors who model comprehensive primary care with a full scope of practice are more positively influential, so recruitment of clerkship preceptors with a wider scope of practice may be important. However, it may be practically difficult for educational leaders to selectively recruit such faculty as preceptors, particularly in communities where a focused scope of practice is more common.
Two studies demonstrated that student attitudes toward family medicine increased after the clerkship, but then declined over time. This is concerning, particularly because many of the included articles used surveys of student attitudes immediately after clerkships as their outcome measure. Further research examining how to best sustain student interest in primary care beyond the clerkship is needed. Implementation and evaluation of the impact of a required primary care clerkship followed by a required primary care rotation in the final clinical year would elucidate this issue further. Future research on clerkships should use robust outcomes data, such as match data or primary care practice, when possible.
There were several limitations to this narrative review. Only studies that took place in the United States, Canada, New Zealand, and Australia were included. Studies not published in English and non-peer reviewed literature were not included. Because of the heterogeneous nature of the literature, a quantitative synthesis was not attempted. More than half of the included articles were published before the year 2000. Much of the research on this topic was either descriptive, a single institution evaluation, or of low to medium quality. Some reported outcomes, such as student self-report of interest or career intention, were likely prone to bias due to the timing or perceived nonanonymity of student responses and their possible impact on student grades and may not have ultimately correlated with primary care practice. Those studies utilizing retrospective surveys may have experienced recall bias. However, the results of the higher-quality articles were congruent and reinforced by the entire body of included articles, telling a consistent story.
Required primary care clerkships were associated with primary care specialty choice. More specifically, the relationship between a required family medicine clerkship in the core clerkship year and family medicine specialty choice has been supported by decades of research. Future high-quality studies evaluating specific features and aspects of clerkships are needed to help medical educators develop clerkships that successfully promote primary care specialty choice.
Acknowledgments
The authors thank Shelby Walker, MD, Virginia Young, MLS, and Morgan Pratte, MPH, for their substantial contributions to the literature search, literature retrieval, and data organization.
Financial Support: This project was partially supported by a grant from the American Board of Family Medicine (ABFM) Foundation (J. Phillips, PI), and also partially by the Health Resources and Services Administration (HRSA) of the United States Department of Health and Human Services (HHS) under grant number D54HP23297, “Academic Administrative Units” (C. Morley, PI). This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by the ABFM, HRSA, HHS, or the US Government.
Presentations: Some portions of this research were presented at the STFM Virtual Conference on Medical Student Education, February 1-4, 2021.
References
- HIS Markit Ltd. The Complexities of Physician Supply and Demand: Projections from 2019-2034. Washington, DC: Association of American Medical Colleges; 2021. Accessed September 3, 2021. https://www.aamc.org/media/54681/download
- Council on Graduate Medical Education. Towards the Development of a National Strategic Plan for Graduate Medical Education, 23rd report. Washington DC: COGME; 2017. Accessed September 3, 2021. https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/graduate-medical-edu/reports/April2017.pdf
- American Academy of Family Physicians. Family Physician Workforce Reform: Recommendations of the American Academy of Family Physicians. Leawood, KS: AAFP; 2014. Accessed September 3, 2021. https://www.aafp.org/about/policies/all/workforce-reform.html
- Bazemore A, Wilkinson E, Petterson S, Green LA. Proportional erosion of the primary care physician workforce has continued since 2010. Am Fam Physician. 2019;100(4):211-212.
- Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of primary care physician supply with population mortality in the United States, 2005-2015. JAMA Intern Med. 2019;179(4):506-514. doi:10.1001/jamainternmed.2018.7624
- Rabinowitz HK. The relationship between medical student career choice and a required third-year family practice clerkship. Fam Med. 1988;20(2):118-121.
- Stine CC, Sheets KJ, Calonge BN. Association between clinical experiences in family practice or in primary care and the percentage of graduates entering family practice residencies. Acad Med. 1992;67(7):475-477. doi:10.1097/00001888-199207000-00014
- Whitcomb ME, Cullen TJ, Hart LG, Lishner DM, Rosenblatt RA. Comparing the characteristics of schools that produce high percentages and low percentages of primary care physicians. Acad Med. 1992;67(9):587-591. doi:10.1097/00001888-199209000-00009
- Clerkship Requirements by Discipline. Association of American Medical Colleges. Washington, DC: AAMC; 2021. Accessed September 3, 2021. https://www.aamc.org/data-reports/curriculum-reports/interactive-data/clerkship-requirements-discipline
- Liaison Committee on Medical Education. Functions and Structure of a Medical School. Washington, DC: LCME; 2021. Accessed September 3, 2021. www.lcme.org
- Elliott J. A review of strategies to improve family medicine as a specialty choice among medical students. Osteopathic Family Physician. 2012; April. doi:10.1016/j.osfp.2012.02.001
- Meurer LN, Bland CJ, Maldonado G. The state of the literature on primary care specialty choice: where do we go from here? Acad Med. 1996;71(1):68-77. doi:10.1097/00001888-199601000-00020
- Pfarrwaller E, Sommer J, Chung C, et al. Impact of interventions to increase the proportion of medical students choosing a primary care career: a systematic review. J Gen Intern Med. 2015;30(9):1349-1358. doi:10.1007/s11606-015-3372-9
- Bennett KL, Phillips JP. Finding, recruiting, and sustaining the future primary care physician workforce: a new theoretical model of specialty choice process. Acad Med. 2010;85(10)(suppl):S81-S88. doi:10.1097/ACM.0b013e3181ed4bae
- Bland CJ, Meurer LN, Maldonado G. Determinants of primary care specialty choice: a non-statistical meta-analysis of the literature. Acad Med. 1995;70(7):620-641. doi:10.1097/00001888-199507000-00013
- Sutton A, Clowes M, Preston L, Booth A. Meeting the review family: exploring review types and associated information retrieval requirements. Health Info Libr J. 2019;36(3):202-222. doi:10.1111/hir.12276
- Phillips JP, Wendling AL, Young V, et al. Medical school characteristics and practices that support primary care specialty choice: a scoping review. Fam Med. 2022;54(7):xxx-xx.
- Sirriyeh R, Lawton R, Gardner P, Armitage G. Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Pract. 2012;18(4):746-752. doi:10.1111/j.1365-2753.2011.01662.x
- Alavi M, Ho T, Stisher C, et al. Factors that influence student choice in family medicine: a national focus group. Fam Med. 2019;51(2):143-148. doi:10.22454/FamMed.2019.927833
- Amundson LH, Hancock BW. The rural family medicine clerkship (RFMC) at the University of South Dakota School of Medicine: a six year review 1977-1982. S D J Med. 1983;36(9):5-11.
- Bass RL, Paulman PM. The rural preceptorship as a factor in the residency selection: the Nebraska experience. J Fam Pract. 1983;17(4):716-719, 719.
- Beck JD, Stewart WL, Graham R, Stern TL. The effect of the organization and status of family practice undergraduate programs on residency selection. J Fam Pract. 1977;4(4):663-669.
- Brearley WD, Simpson W, Baker RM. Family practice as a specialty choice: effect of premedical and medical education. J Med Educ. 1982;57(6):449-454. doi:10.1097/00001888-198206000-00004
- Campos-Outcalt D, Senf JH. Characteristics of medical schools related to the choice of family medicine as a specialty. Acad Med. 1989;64(10):610-615.
- Campos-Outcalt D, Senf J. Medical school financial support, faculty composition, and selection of family practice by medical students. Fam Med. 1992;24(8):596-601.
- Campos-Outcalt D, Senf J, Pust R. Family practice specialty preference before and after a required clerkship. Fam Pract Res J. 1992;12(2):213-221.
- Campos-Outcalt D, Senf J. A longitudinal, national study of the effect of implementing a required third-year family practice clerkship or a department of family medicine on the selection of family medicine by medical students. Acad Med. 1999;74(9):1016-1020. doi:10.1097/00001888-199909000-00016
- Campos-Outcalt D, Senf J, Kutob R. A comparison of primary care graduates from schools with increasing production of family physicians to those from schools with decreasing production. Fam Med. 2004;36(4):260-264.
- Chaulk CP, Bass RL, Paulman PM. Physicians’ assessments of a rural preceptorship and its influence on career choice and practice site. J Med Educ. 1987;62(4):349-351.
- Duerson MC, Crandall LA, Dwyer JW. Impact of a required family medicine clerkship on medical students’ attitudes about primary care. Acad Med. 1989;64(9):546-548.
- Friedman CP, Baker RM, Ilderton EP. Functions of a family medicine preceptorship. J Med Educ. 1979;54(7):567-575.
- Geske JA, Hartman T, Goodman B, Paulman P. Influence of a rural family medicine rotation on residency selection: MS3 versus MS4. Fam Med. 2011;43(8):556-559.
- Godkin M, Quirk M. Why students chose family medicine: state schools graduating the most family physicians. Fam Med. 1991;23(7):521-526.
- Kassebaum DG, Haynes RA. Relationship between third-year clerkships in family medicine and graduating students’ choices of family practice careers. Acad Med. 1992;67(3):217-219. doi:10.1097/00001888-199203000-00018
- Levy BT, Hartz A, Merchant ML, Schroeder BT. Quality of a family medicine preceptorship is significantly associated with matching into family practice. Fam Med. 2001;33(9):683-690.
- Musham C, Chessman A. Changes in medical students’ perceptions of family practice resulting from a required clerkship. Fam Med. 1994;26(8):500-503.
- Paulman PM, Davidson-Stroh L. The effect of a rural family practice preceptorship on medical students’ residency selection. Fam Pract Res J. 1993;13(4):385-389.
- Paulus R, Byler D, Casapulla S. Student and preceptor experiences in a mini longitudinal integrated clerkship: A participatory self-study. PRiMER Peer-Rev Rep Med Educ Res. 2020;4:24. doi:10.22454/PRiMER.2020.439679
- Phillips J, Charnley I. Third- and fourth-year medical students’ changing views of family medicine. Fam Med. 2016;48(1):54-60.
- Scott I, Wright B, Brenneis F, Brett-Maclean P, McCaffrey L. Why would I choose a career in family medicine?: reflections of medical students at 3 universities. Can Fam Physician. 2007;53(11):1956-1957.
- Wimsatt LA, Cooke JM, Biggs WS, Heidelbaugh JJ. Institution-specific factors associated with family medicine residency match rates. Teach Learn Med. 2016;28(3):269-278. doi:10.1080/10401334.2016.1159565
- Barish AM. The influence of primary care preceptorships and other factors on physicians’ career choices. Public Health Rep. 1979;94(1):36-47.
- Bazargan M, Lindstrom RW, Dakak A, Ani C, Wolf KE, Edelstein RA. Impact of desire to work in underserved communities on selection of specialty among fourth-year medical students. J Natl Med Assoc. 2006;98(9):1460-1465.
- Blue AV, Chessman AW, Geesey ME, Garr DR, Kern DH, White AW. Medical students’ perceptions of rural practice following a rural clerkship. Fam Med. 2004;36(5):336-340.
- Brooks CH. Do area health education center programs produce primary care specialists? Results of a longitudinal study. Int J Health Serv. 1992;22(3):567-578. doi:10.2190/FLCX-NYD9-MBUA-FYJ5
- Dever GE, Eveland AP, Tedders SH, Fehlenberg RD, Laurens MB, Harrelson JC. Impact of a population-based medical curriculum on specialty choice. J Health Care Poor Underserved. 2001;12(3):261-271. doi:10.1353/hpu.2010.0817
- Dogbey GY, Collins K, Russ R, Brannan GD, Mivsek M, Sewell S. Factors associated with osteopathic primary care residency choice decisions. J Am Osteopath Assoc. 2018;118(4):225-233.
- Gaufberg E, Hirsh D, Krupat E, et al. Into the future: patient-centredness endures in longitudinal integrated clerkship graduates. Med Educ. 2014;48(6):572-582. doi:10.1111/medu.12413
- Gazewood JD, Owen J, Rollins LK. Effect of generalist preceptor specialty in a third-year clerkship on career choice. Fam Med. 2002;34(9):673-677.
- Harris DL, Bluhm HP. An evaluation of primary care preceptorships. J Fam Pract. 1977;5(4):577-579.
- Kassebaum DG, Szenas PL. Factors influencing the specialty choices of 1993 medical school graduates. Acad Med. 1994;69(2):163-170. doi:10.1097/00001888-199402000-00027
- Latessa R, Beaty N, Royal K, Colvin G, Pathman DE, Heck J. Academic outcomes of a community-based longitudinal integrated clerkships program. Med Teach. 2015;37(9):862-867. doi:10.3109/0142159X.2015.1009020
- Poole P, McHardy K, Janssen A. General physicians: born or made? The use of a tracking database to answer medical workforce questions. Intern Med J. 2009;39(7):447-452. doi:10.1111/j.1445-5994.2008.01717.x
- Potts MJ, Brazeau NK. The effect of first clinical clerkship on medical students’ specialty choices. Med Educ. 1989;23(5):413-415. doi:10.1111/j.1365-2923.1989.tb00895.x
- Rucker L, Morgan C, Ward KE, Bell BM. Impact of an ambulatory care clerkship on the attitudes of students from five classes (1985-1989) toward primary care. Acad Med. 1991;66(10):620-622. doi:10.1097/00001888-199110000-00019
- Senf JH, Campos-Outcalt D, Watkins AJ, Bastacky S, Killian C. A systematic analysis of how medical school characteristics relate to graduates’ choices of primary care specialties. Acad Med. 1997;72(6):524-533. doi:10.1097/00001888-199706000-00020
- Shore WB, Rodnick JE. A required fourth-year ambulatory clerkship: a 10-year experience with family practice and primary care internal medicine sites. Fam Med. 1993;25(1):34-40.
- Thistlethwaite J, Kidd MR, Leeder S, Shaw T, Corcoran K. Enhancing the choice of general practice as a career. Aust Fam Physician. 2008;37(11):964-968.
- Vohra A, Ladyshewsky R, Trumble S. Factors that affect general practice as a choice of medical speciality: implications for policy development. Aust Health Rev. 2019;43(2):230-237. doi:10.1071/AH17015
- Wamsley MA, Dubowitz N, Kohli P, Cooke M, O’Brien BC. Continuity in a longitudinal out-patient attachment for Year 3 medical students. Med Educ. 2009;43(9):895-906. doi:10.1111/j.1365-2923.2009.03424.x
- Xu G, Veloski JJ, Politzer RM, Pathman D. Factors influencing learners’ specialty decisions. Acad Med. 1997;72(6):469-470. doi:10.1097/00001888-199706000-00001
- Arora V, Wetterneck TB, Schnipper JL, et al. Effect of the inpatient general medicine rotation on student pursuit of a generalist career. J Gen Intern Med. 2006;21(5):471-475. doi:10.1111/j.1525-1497.2006.00429.x
- Babbott D, Levey GS, Weaver SO, Killian CD. Medical student attitudes about internal medicine: a study of U.S. medical school seniors in 1988. Ann Intern Med. 1991;114(1):16-22. doi:10.7326/0003-4819-114-1-16
- Davidson RA, Harris JO, Schwartz MD. A simple ambulatory-care experience and students’ residency choices and attitudes toward general internal medicine. Acad Med. 1993;68(4):311-312. doi:10.1097/00001888-199304000-00026
- Durning SJ, Elnicki DM, Cruess DF, et al. Almost internists: analysis of students who considered internal medicine but chose other fields. Acad Med. 2011;86(2):194-200. doi:10.1097/ACM.0b013e3182045ee5
- Hauer KE, Durning SJ, Kernan WN, et al. Factors associated with medical students’ career choices regarding internal medicine. JAMA. 2008;300(10):1154-1164. doi:10.1001/jama.300.10.1154
- Hauer KE, Fagan MJ, Kernan W, Mintz M, Durning SJ. Internal medicine clerkship directors’ perceptions about student interest in internal medicine careers. J Gen Intern Med. 2008;23(7):1101-1104. doi:10.1007/s11606-008-0640-y
- Marple RI, Pangaro L, Kroenke K. Third-year medical student attitudes toward internal medicine. Arch Intern Med. 1994;154(21):2459-2464. doi:10.1001/archinte.1994.00420210097011
- Ramsbottom-Lucier M, Martin D, Carline J, Shannon N, Ramsey P. Influence of an office-based internal medicine clerkship on selection of primary care training programs: A 5-year experience. Teach Learn Med. 1996;8(4):200-207. doi:10.1080/10401339609539798
- Schwartz MD, Linzer M, Babbott D, Divine GW, Broadhead WE; The Society of General Internal Medicine Task Force on Career Choice in Internal Medicine. The impact of an ambulatory rotation on medical student interest in internal medicine. J Gen Intern Med. 1995;10(10):542-549. doi:10.1007/BF02640362
- Schwartz MD, Durning S, Linzer M, Hauer KE. Changes in medical students’ views of internal medicine careers from 1990 to 2007. Arch Intern Med. 2011;171(8):744-749. doi:10.1001/archinternmed.2011.139
- Jospe N, Kaplowitz PB, McCurdy FA, Gottlieb RP, Harris MA, Boyle R. Third-year medical student survey of office preceptorships during the pediatric clerkship. Arch Pediatr Adolesc Med. 2001;155(5):592-596. doi:10.1001/archpedi.155.5.592
- Kaplowitz PB, Boyle R, Lu J. The effect of the pediatric clerkship on medical student attitudes toward pediatrics at 11 medical schools. Arch Pediatr Adolesc Med. 1996;150(4):435-439. doi:10.1001/archpedi.1996.02170290101018
- Wilson WG. Possible influences of clerkship timing and site on residency choice. Acad Med. 1997;72(7):567. doi:10.1097/00001888-199707000-00006
- Seehusen D, Raleigh M, Phillips JP, et al. Institutional Characteristics Influencing Medical Student Selection of Primary Care Careers: A Narrative Review and Synthesis. Fam Med. 2022;54(7):xxx-xx.



There are no comments for this article.