Background and Objectives: The United States, like many other nations, faces a chronic shortage of primary care physicians. The purpose of this scoping review was to synthesize literature describing evidence-based institutional practices and interventions that support medical students’ choices of primary care specialties, published in the United States, Canada, Australia, and New Zealand.
Methods: We surveyed peer-reviewed, published research. An experienced medical librarian conducted searches of multiple databases. Articles were selected for inclusion based on explicit criteria. We charted articles by topic, methodology, year of publication, journal, country of origin, and presence or absence of funding. We then scored included articles for quality. Finally, we defined and described six common stages of development of institutional interventions.
Results: We reviewed 8,083 articles and identified 199 articles meeting inclusion criteria and 41 related articles. As a group, studies were of low quality, but improved over time. Most were quantitative studies conducted in the United States. Many studies utilized one of four common methodologic approaches: retrospective surveys, studies of programs or curricula, large-scale multi-institution comparisons, and single-institution exemplars. Most studies developed groundwork or examined effectiveness or impact, with few studies of planning or piloting. Few studies examined state or regional workforce outcomes.
Conclusions: Research examining medical school interventions and institutional practices to support primary care specialty choice would benefit from stronger theoretical grounding, greater investment in planning and piloting, consistent use of language, more qualitative methods, and innovative approaches. Robust funding mechanisms are needed to advance these goals.
The United States, like many other nations, faces a chronic shortage of primary care physicians that negatively impacts population health and contributes to rising health care costs.1-3 Patients with access to primary care are less likely to use emergency care3,4 or be hospitalized,3,5 receive better preventive care,6-8 and live longer.9 However, primary care careers remain unpopular among US medical students.10 Eroding student interest in primary care is contributing to the decline of primary care services in the United States, leading to greater health inequities and poor public health outcomes, even in the context of extraordinary health care spending.11 Notably, a minority of medical schools consistently graduate large numbers of students who become primary care physicians,12 suggesting that institutional culture and practices can profoundly impact the future primary care workforce.13
Our purpose was to review published research literature to identify evidence-based institutional practices and interventions that support primary care specialty choices among medical students in the United States, Canada, Australia, and New Zealand. Previous reviews have described the complex range of influences that shape students’ primary care career interests.14-16 Building on that work, this study focuses on medical school institutional characteristics and practices that promote primary care. This next step is important because medical schools control both entry to the profession and the learning environment in which physicians become professionals and choose longitudinal career specialties. A review of this nature moves the focus away from the decisions of individual students and brings it toward institutional and collective solutions.
Medical schools are drivers of innovation and have a clear ethical obligation to attend to the physician workforce needs of the populations they serve.17-19 Although structural shifts, policy change, cultural change, and educational innovation represent real investments of time and financial resources, they are feasible. Medical schools and programs founded on innovative models have produced meaningful results,20,21 and traditional institutions that have undertaken real change have made a substantial impact.22 In this comprehensive study, we specifically focused on policies, courses, programs, and academic structures that are modifiable by medical schools.
This scoping review presents an overview of the historical evolution of literature on this topic, describes common topics of study and methodologic approaches, describes key gaps and areas of weakness, and suggests further opportunities for institutional innovation and scholarship. In additional narrative reviews, we examined the findings in greater depth, evaluating each of the major topic areas identified in the scoping process.23-29
Approach
We developed an unregistered study protocol at the time of study initiation (2016) and modified it accordingly as the study evolved. We selected scoping review methodology because this approach fit best with the goals of identifying common topics, methodologies, and gaps in literature.30 We consulted methodologic sources, including the PRISMA guidelines for scoping reviews, during study development, implementation, and manuscript preparation.31-33 Consistent with scoping review methodology, we allowed our methods to evolve iteratively, reflecting the literature discovery process.34 We focused on primary scholarship, and thus included only peer-reviewed published research. Our primary interest was in the United States. We also included studies from Canada, Australia, and New Zealand because these countries have similar educational structures and workforce challenges.35 We did not limit the literature by year of publication.
Search Strategy, Filters, and Limits
An experienced medical librarian (V.Y.) conducted an initial MEDLINE (PubMed) search. Search terms were compiled using exemplar articles identified in a basic literature review. The search was modified iteratively in collaboration with researchers (authors C.M., J.P.P., J.P., and A.W.)* who are experienced in this topic. We focused on capturing the literature with a high degree of sensitivity, capturing the diversity of educational programs developed to influence specialty choice and including research that examined the varied financial, social, psychological, and academic factors of student choice (Appendix 1: https://journals.stfm.org/media/4915/phillips-july22-appendix-1.pdf). We limited results to English language availability. We internally validated the initial search by ensuring that many key publications on the topic, identified by content experts, had been captured.
We then conducted a comprehensive MEDLINE (PubMed) search on April 20, 2016. The MEDLINE search strategy was translated into both the Scopus database (Elsevier) and the Cumulative Index to Nursing and Allied Health (CINAHL), and conducted December 21, 2017. With our focus on identifying peer-reviewed scholarship, we did not search gray literature.36
To ensure currency while the review was being conducted, we reran the search several times, using the same databases and search strategy, with the final search conducted in June 2019. Review articles were identified both through the search process and by hand-review conducted by content experts (authors J.P.P., J.P., and A.W.), and bibliographies of these reviews were also searched. The scoping review search was used as a foundation for searches examining five distinct topics, defined below, which are described in subsequent manuscripts.23-29 Each granular topic area used the base structure of the scoping review search and added additional subject-specific terms and controlled vocabulary to refine the scope, again in consultation with a medical librarian (author I.K.G.).
Article Selection
The results of the searches were sorted one by one, divided among the content experts (C.M., J.P.P., J.P., and A.W.). Before reviewing the articles, we developed and reviewed clear inclusion and exclusion criteria. Because of the broad scope of the study and the high sensitivity of the search, article titles and abstracts were initially reviewed by a single researcher familiar with primary care medical education and the existing literature (J.P.P., J.P., or A.W.). Where uncertainty about inclusion existed, each article was discussed with one or more additional researchers until consensus was reached. When necessary, the full text of the article was reviewed. We initially used Microsoft Excel as a data management tool; as the literature was sorted, we used Mendeley to organize the data set. Two medical librarians led manuscript retrieval, search strategy formulation and documentation, and collation of bibliographic data (V.Y. and I.K.G.).
After we identified the complete list of included articles, the abstract of each included article was again reviewed by a single researcher (J.P.P.) to ensure consistent application of the inclusion criteria through time. The full text of each included article was then reviewed by at least one author (A.K., C.L., A.L., B.N., D.S.). The entire research team met periodically (1-2 times per month) to discuss the manuscript selection process. In each instance, before making changes to the final set, two or more authors discussed the manuscripts, always with input from the study’s principal investigator (J.P.P.).
Inclusion and Exclusion Criteria
We excluded articles that studied students outside of the United States, Canada, Australia, and New Zealand; were not primary research; or were outside the study scope. Nonresearch articles, such as essays and commentaries, were excluded. Studies were not excluded based on quality. We excluded review articles from analysis, but we reviewed their bibliographies to ensure primary studies had not been missed.
Initially, the researchers focused exclusively on articles that explicitly evaluated an institutional practice, curriculum, or intervention, such as a family medicine clerkship. However, in taking this approach, we would have excluded many related articles that provided indirect evidence in support of such interventions, and could also be useful for identifying gaps in the research literature. For example, although a quantitative analysis of the impact of a structured mentoring program on student specialty choice would be considered an educational intervention, a qualitative study describing the importance of mentorship in students’ specialty choices would not be. Thus, we broadened the inclusion criteria to include evidence that contributed theoretical support to an intervention, such as a qualitative mentorship study, as well as interventions themselves. For purposes of mapping the scope of research, we kept these related studies separate from the studies of interventions.
In this literature, prospective interventional studies are rare. Thus, we included all research studies within the topic’s scope, including descriptive studies with no rigorous evaluation. However, studies that did not provide evidence pertinent to an educational intervention and student choice of primary care were not included, even if they described an issue important to medical students’ career decisions. For example, we did not include studies that described only the influence of specific aspects of various specialties (such as lifestyle, income, or procedural orientation). We also excluded graduate medical education interventions.
Included studies were required to describe an outcome pertinent to primary care specialty interest or choice. We broadly defined primary care specialty choice to include practice in primary care, general medicine, general practice, or family medicine; match in family medicine, general medicine, internal medicine, or pediatrics; student interest in primary care, general medicine, or family medicine; or student attitudes toward primary care or family medicine. We also allowed authors of each publication in the review to define primary care, allowing for a broad range of literature to be captured. However, studies that solely evaluated interest or match in internal medicine, pediatrics, or another discipline, without a general or primary care focus, were not included. Studies that solely examined geographic outcomes, such as rural practice interest, were also excluded, unless they also examined primary care interest or outcomes. We carefully considered each of these methodologic issues, but we concluded that inclusion of these manuscripts would dilute our ability to evaluate the primary research question, without adding meaningfully to study findings.
Data Charting
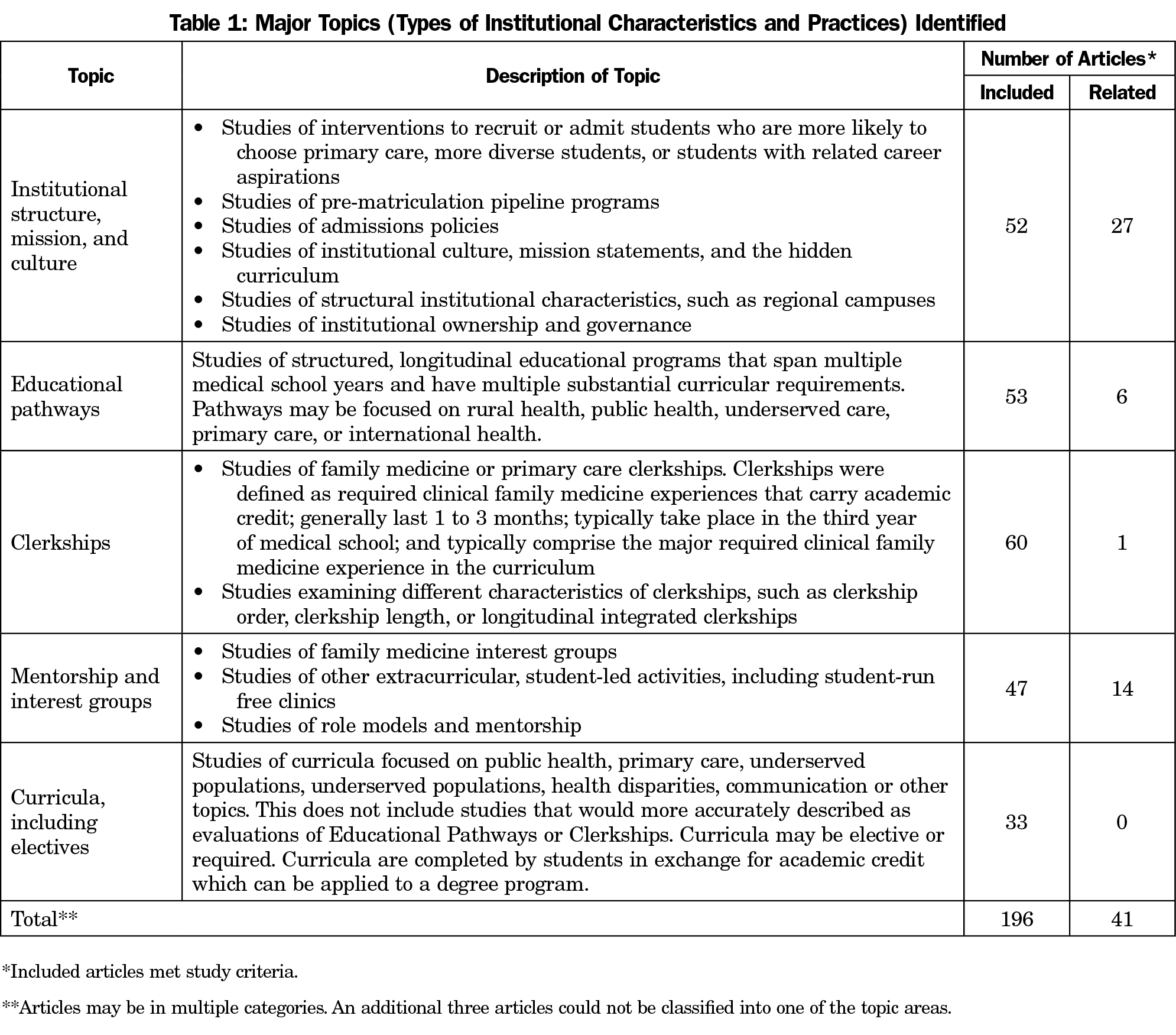
After initial review of the literature, we identified five major topic areas, each describing a particular type of institutional structure or practice. We sorted articles into these five groups: institutional features and admissions processes, educational pathways, clerkships, mentorship and interest groups, and other curricula, including electives (Table 1). We developed rigorous definitions of each topic before charting began and referenced these definitions continually. Throughout this charting process, all articles were charted by at least two researchers, using Excel as an organizing structure, and consulting a written rubric. Where there was disagreement between the two researchers, a third researcher was consulted, and difficult categorizations were discussed to consensus, consulting with the principal investigator when needed.
We charted articles based on their fit with the study definitions, not with the terminology used within each article. Topic classifications were not mutually exclusive. For example, a single study might include study of both curriculum and mentorship in influencing students’ career choices.
Included studies were also charted by a single investigator (S.W.) based on their use of qualitative methods, quantitative methods, or both; year of publication; journal of publication; country of origin; and presence or absence of a reported funding source. The principal investigator (J.P.P.) then charted the funded studies by their primary funding source.
Language Mapping
One researcher (J.P.P.) reviewed the full text of each included study and created a map of terms used to describe key educational interventions in each topic area.
Quality Assessment
The quality of included articles was quantitatively evaluated using a 16-item quality assessment tool developed by Sirriyeh et al.37 We chose this instrument because it was developed specifically for evaluating studies with a range of methodologies, was suitable for social science research, and had been assessed for reliability and validity. All authors were trained on use of the instrument by the central author team (C.M., J.P.P., J.P., A.W.). During training, group members asked clarifying questions which enabled the group to create a shared understanding of the application of the tool, including consensus definitions for the applied criteria. Each included article was reviewed independently by two researchers, and quality rankings for each were averaged. When the researchers disagreed in their ranking by more than a standard deviation, articles were discussed to a consensus quality ranking. When articles were descriptive only, with no formal qualitative or quantitative analyses, they were not assessed for quality.
We used Pearson correlations to analyze whether year of publication correlated with study quality. We used independent samples t tests to evaluate whether funded studies were of higher quality.
Synthesis of Results
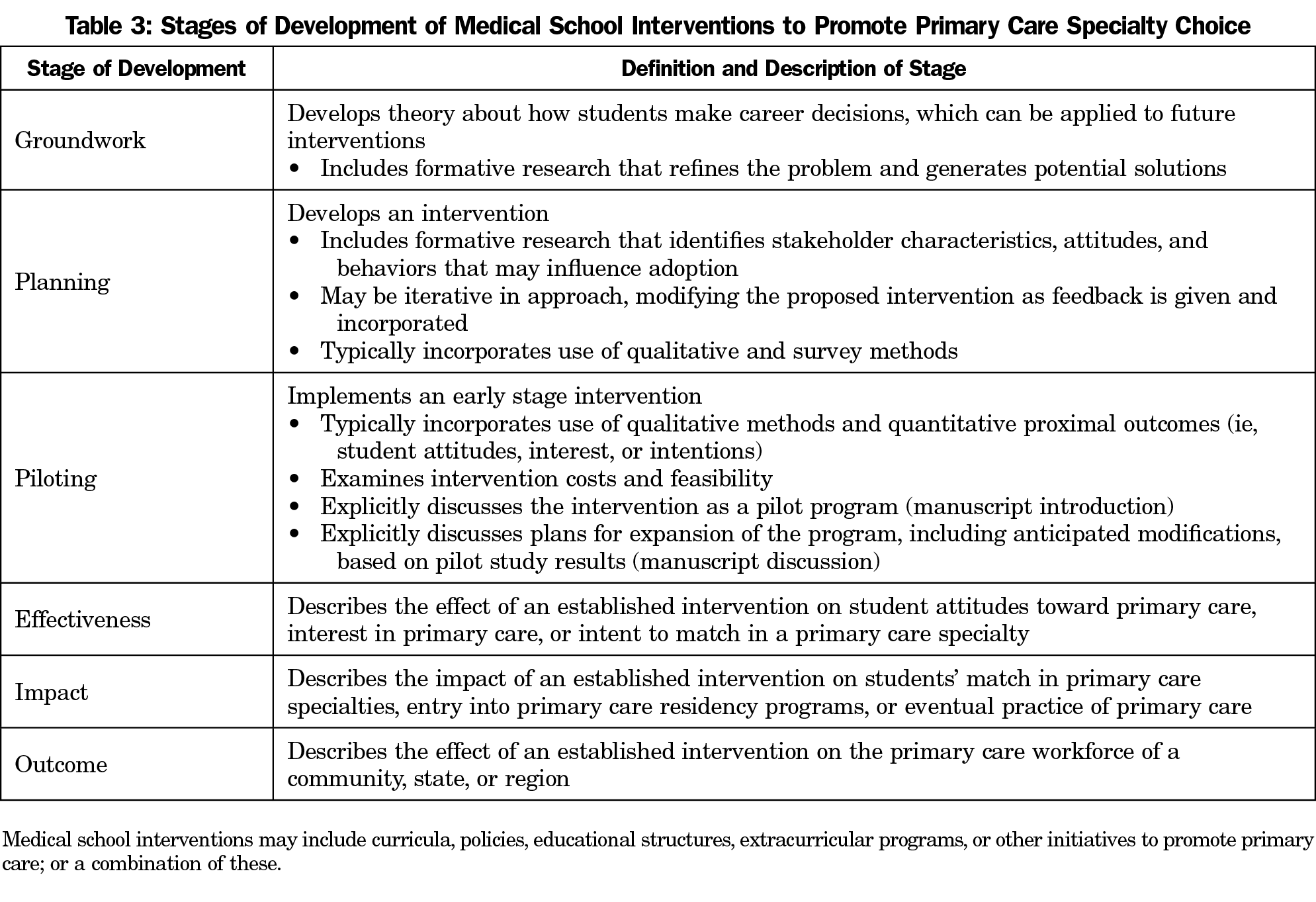
We reviewed and critiqued the quantitative results of the data charting and qualitative assessment. We used a communication science implementation framework to define common stages of development of institutional interventions, and then critiqued the literature in light of this framework.38,39 At this stage, we focused not only on the abstracts, methods, and results of the studies, but also critically examined the introductions and discussion sections, to best understand how authors of each manuscript framed their work. Finally, we reflected on the process of reviewing the included and related manuscripts, collectively discussed gaps in the literature, and critically reflected on the findings in order to create new discourse.
The Michigan State University Institutional Review Board determined the study to be non-human subjects research.
Search Results and Included Articles
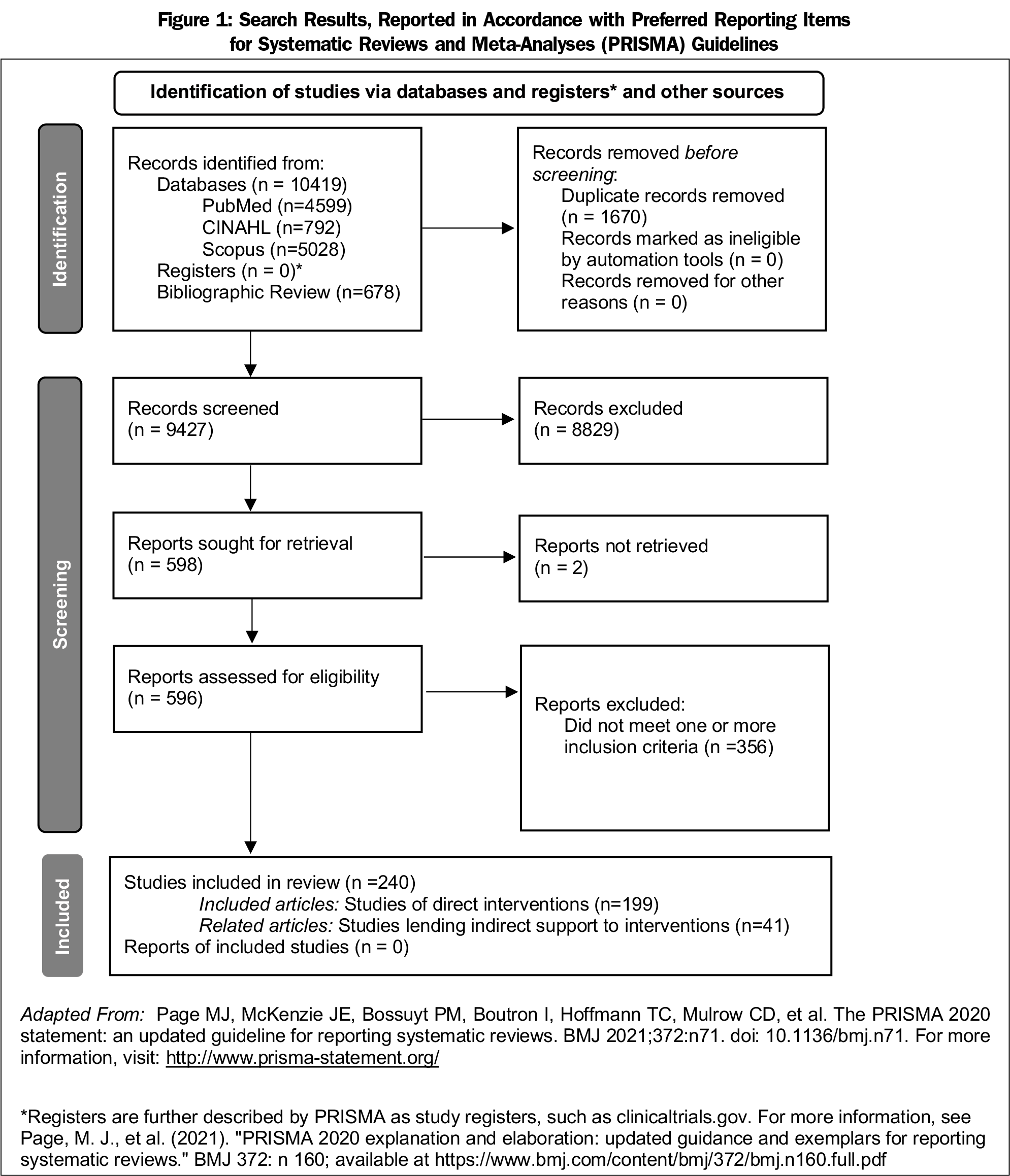
The initial comprehensive PubMed search (April 20, 2016) captured 3,309 articles. Searches of Scopus and CINAHL (December 21, 2017) yielded an additional 3,830 articles. Updates of the search, conducted in March 2017, January 2018, and June 2019, yielded an additional 1,581 articles. We identified 56 additional articles by searching for older articles published without abstracts. Searches of bibliographies of review articles yielded 678 additional articles. In total, we reviewed 9,427 titles, 1,334 abstracts, and 596 full-text articles. We excluded two articles because of an inability to find the source publication. After full-text review, we excluded 356 articles because they did not meet our inclusion criteria (not research studies or did not measure a primary care outcome). The final data set included 199 articles; 41 additional related articles were identified (Figure 1).
Topics and Terminology
We classified medical school practices into five key topic areas (Table 1). Three articles met inclusion criteria for the study but could not be classified into one of these topic areas.40-42
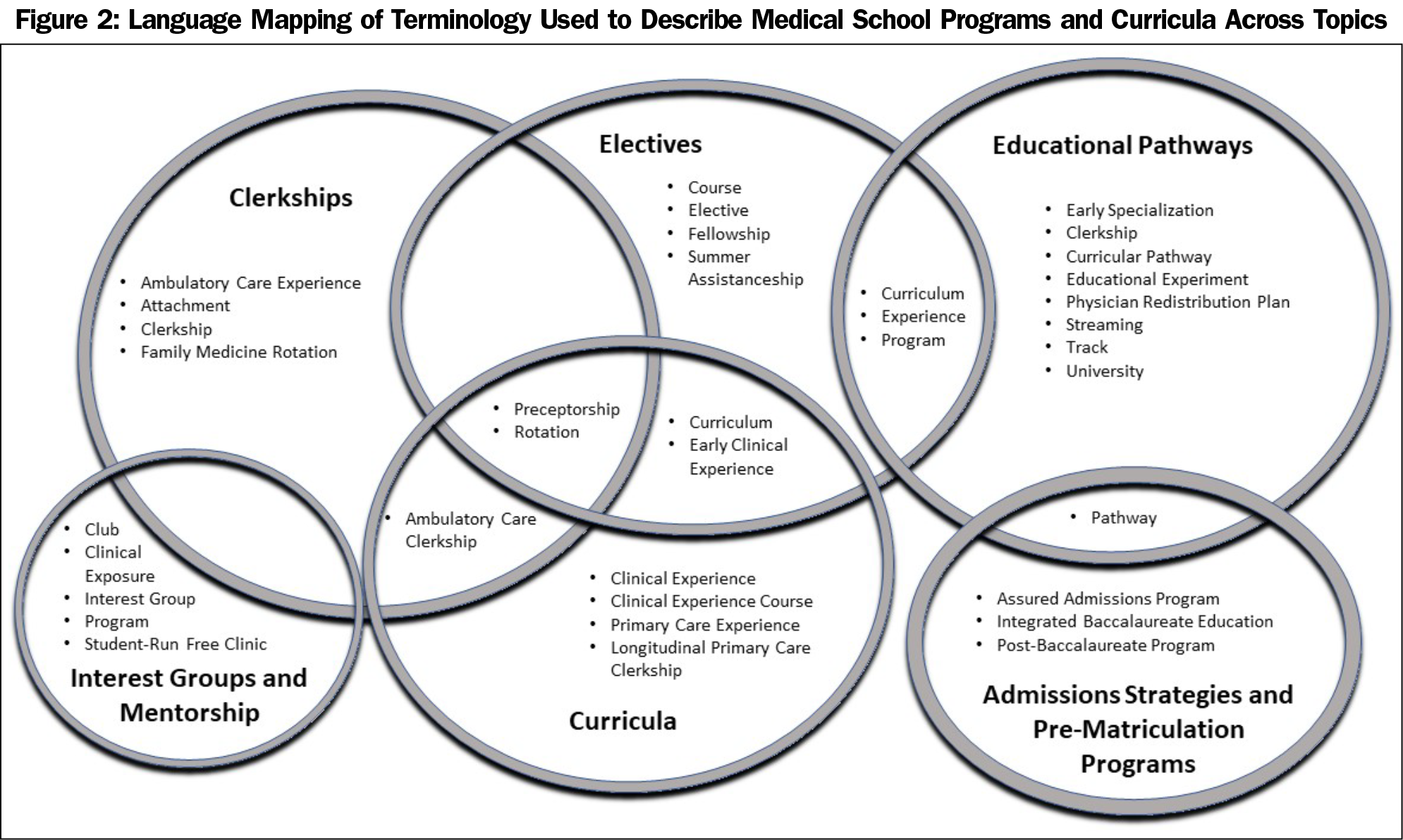
In the process of charting, we noted substantial variation and overlap in terminology used to describe medical school curricula and programs (Figure 2). Consistent use of terminology was noted for only one topic: clerkships. The term “clerkship” was first used in the late 1980s and used with extremely high consistency after 1990 when describing clerkships (as defined in Table 1). However, the term “clerkship” was still regularly used to describe other types of interventions.
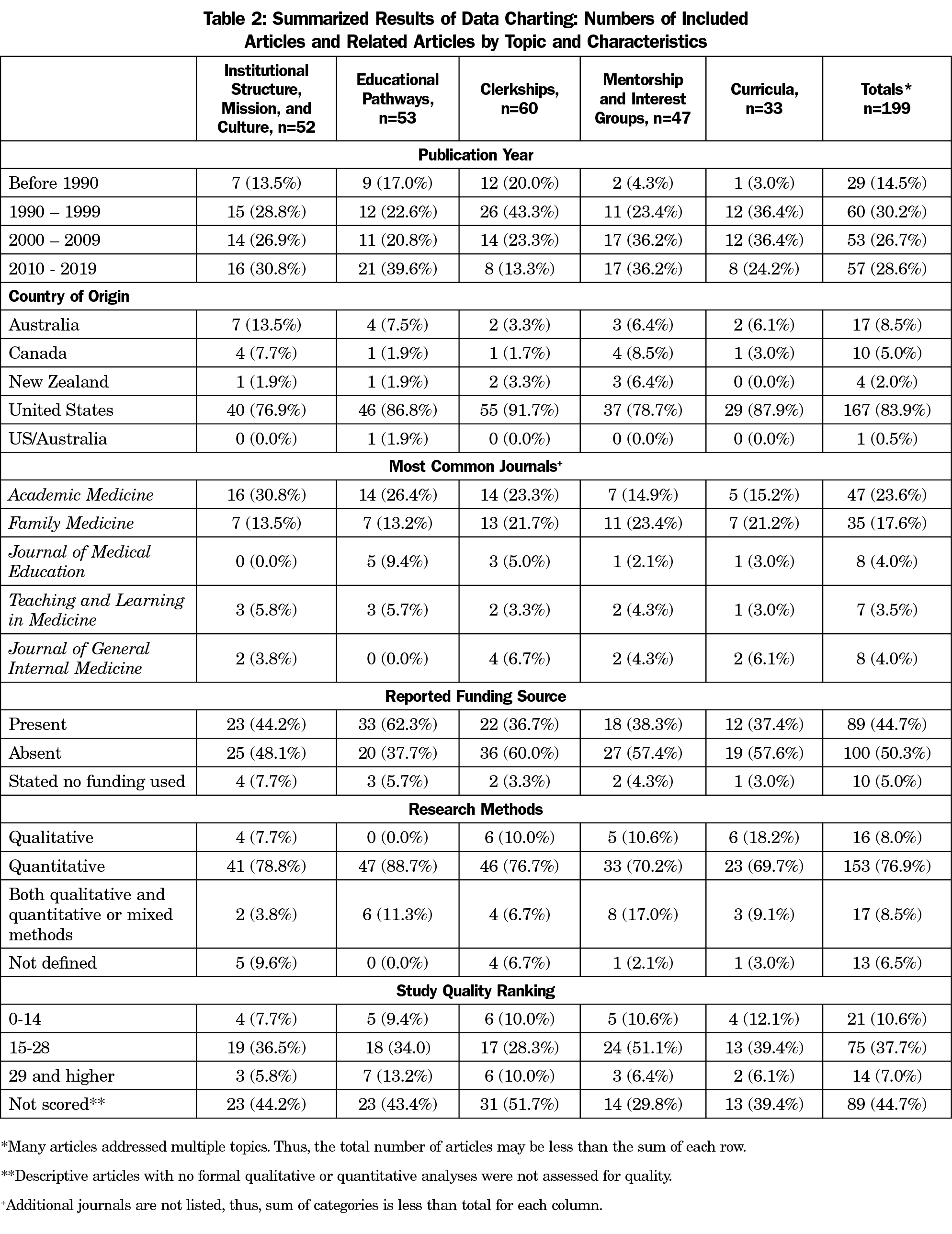
Historical Evolution
The first articles meeting inclusion criteria for the study were published in 1977. The number of publications per year steadily increased through the early 1990s, and the volume of research has stayed relatively consistent since that time (Table 2). On average, since 1990, 4.3 manuscripts have been published per year meeting study inclusion criteria. Published research on educational pathways has increased the most in the past decade: the number of manuscripts published between 2010 and mid-2019 was about twice the number published between 2000 and 2009. In contrast, the number of manuscripts published on clerkships and curricula has recently declined. The most common journals of publication were Academic Medicine (47 publications) and Family Medicine (35 publications).
Study Quality
As has been described previously,15,43 the studies often had relatively low quality scores. A total of 89 studies could not be scored because they included only description, without formal qualitative or quantitative analyses (Table 2). Among the 110 scored studies, the mean score was 20.3 (standard deviation 6.8, range 7-41) among a potential score range of 0-48. Most often, studies were assessed to be of poor quality based on absence of an explicit theoretical framework, lack of validation of study instruments, and lack of justification for the data collection and analysis methods selected. Quality did not vary substantially across topic areas. The assessed quality of the literature did improve with time (r=0.271; P=.004). Mean quality score by decade was: 1977-1989: 15.5; 1990-1999: 20.6; 2000-2009: 20.1; 2010-2019: 21.9.
Research Support
The majority of included studies (110 of 199, 55%) were unfunded or did not state a funding source (Table 2). Of the 89 funded studies, 36 (40.4%, or 18.0% of the total) indicated a primary federal (national government) funding source (Appendix 2: https://journals.stfm.org/media/4916/phillips-july22-appendix-2.pdf). The presence of funding did not vary significantly by decade of publication. Studies of institutional pathways were the most likely to have funding (33 of 53, 62%), followed by studies of institutional structure, mission, and culture (23 of 52, 44%). The most common funding sources were the US Health Resources and Services Administration; internal sources (such as medical schools and departments); and state, province, or city government. Three studies were supported by the National Institutes of Health. Funded studies did not have significantly higher quality scores (mean funded quality score 19.9; mean unfunded quality score 20.7; P=.55).
Common Research Approaches
Of the included articles, 16 utilized qualitative methods, 153 utilized quantitative methods, and 17 combined qualitative and quantitative methods or used mixed methods. Upon repeated immersive reading of the included studies, we noted four often-repeated methodological approaches. These were:
- Retrospective surveys. Many studies surveyed family physicians or primary care physicians in practice and asked them to identify key influences on their career choice.44,45 Surveys were typically written (or electronic) and self-reported. Some of these surveys were conducted with comparison groups in different specialties. Others surveyed residents or senior medical students, rather than practicing physicians.46-48 Usually the survey respondents were students or alumni from a single institution, although a few used larger samples.49 A few studies used rigorous qualitative methods to explore the experiences of students, residents, or physicians in practice about their career choice process;50-54 but this rigorous qualitative evaluation was uncommon.
- Studies of programs or curricula. Many studies examined programs or curricula for their relationship with medical student interest in primary care, match into a primary care specialty, or eventual practice of primary care.55-60 These were nearly all single-institution studies and usually had small sample sizes. Almost universally, these studies examined outcomes quantitatively. At times, participants in programs were compared to nonparticipants, but controlled comparisons (ie, controlling for student intent to participate or for other student characteristics) were rare. Often studies used a before-and-after comparison approach, typically examining change in student attitudes or intentions, using instruments without validity testing.
Some programmatic studies included detailed descriptions of the programs themselves, but these were written from the perspectives of the authors.61,62 With a few exceptions,63 the experiences of learners were usually absent. If learner perspectives were described, they generally had not been gathered and evaluated using rigorous qualitative methods.
- Large-scale multi-institution comparisons. Some studies quantitatively compared many medical schools, often all allopathic medical schools in the United States. These studies were most often secondary data analyses, typically using data collected by the Association of American Medical Colleges, using students’ career intentions at the time of medical school graduation as an outcome.64,65 Others used American Medical Association Masterfile data to compare the practices of physicians who had graduated from US medical schools.66,67 Osteopathic institutions were typically excluded. Most often, these studies compared institutions with a given structure, curriculum, or policy to institutions without that characteristic.
- Single-institution exemplar studies. A small number of studies described single medical schools in detail, often describing their missions, structure, curricula, and outcomes, holding them up as exemplars.68-70 These studies often characterized student career intentions, match, or practice outcomes using a descriptive approach. They also included description of curricula and programs from an institutional perspective, but qualitative examination of student experiences was generally absent.
The literature review included some manuscripts that did not fit into the common research approaches above,71-73 but most publications could be classified in these four groups.
Stages of Development
We defined six stages of intervention, based on an implementation framework,38,39 to develop strategies to promote primary care specialty choice: groundwork, planning, piloting, effectiveness, impact, and outcome (Table 3). The literature included many studies of groundwork: studies that developed theory about the ways that students make career choices.49,73 As described above, many of these were retrospective surveys; however, this literature also included some high-quality qualitative studies.50,71 Studies examining effectiveness and impact were also very common; these examined the relationships between structure or curricula and students’ attitudes, intentions, match, residency placement, or eventual primary care practice, usually using only quantitative methods.74-76
However, the developmental stages between developing theory, and examining the impact of an intervention, were largely missing. Groundwork studies sometimes described the applicability of their findings to potential interventions in the discussion sections, in a general way. However, authors of these studies rarely described a clear relationship to a specific intervention in which they, as educators, planned to invest. Planning and piloting studies were almost entirely absent. Even when authors had developed a small, single-institution intervention that did not have the impact they were expecting, they typically did not describe them as pilot studies, and rarely indicated plans to refine or expand them. The iterative process of program evaluation and improvement was often missing from manuscripts. It was also rare for authors to describe a specific theoretical approach or understanding of student career development when describing the development of curricular programs.
Finally, although many authors aimed to increase the proportion of primary care physicians in a specific region or state, few studies examined this outcome. Many demonstrated that programs had a high proportion of graduates practicing in a particular state or region, or practicing in primary care; but few quantitatively examined the impact of the program on the workforce of a state or region from a geographic or public health lens.70 No studies examined population health outcomes.
Gaps in Published Literature
Although we initiated this study with the goal of examining medical school curricula, policies, and structures, discussion of the development and impact of medical school policies was almost entirely absent. The exception was studies of mission statements, which have been examined by several authors.19 Notably, very few studies examined medical school admissions policies and procedures.
Relatively few studies of educational approaches were extracurricular (ie, activities not granted academic credit), but not student-led. For example, although a preponderance of groundwork scholarship indicates that mentorship is important, there were no examples of structured mentoring programs led by the institution. Similarly, no studies examined the impact of family medicine-led support for third- and fourth-year medical students during the residency application and match process.
Moving Beyond Historical Approaches
Studies within the scoping review’s body of literature were often of poor quality. At times we found it challenging to describe the research methods of a given study and had to work to avoid giving the authors the benefit of the doubt when scholarship lacked rigor. Indeed, many studies did not truly ask or answer a research question that can inform future scholarship. However, the rigor of published scholarship has improved with time (as demonstrated by increased quality scores). Seeing the evolution of the literature is heartening. Several factors may contribute to this problem, and understanding these influences may help all of us improve the rigor of our work in the future.
First, medical education research is often conducted by physicians, whose education has been strongly informed by a positivistic, reductionist approach to understanding the world.77 Many clinician researchers are not even aware of this ontological and epistemological foundation, because they are immersed in it; a positivistic approach is typically not acknowledged.
Many medical education journals do not expect authors to frame their work around a theoretical model. This omission is problematic because the process of how students experience medical education and ultimately make career choices is a social science question. Partnering with social scientists, strengthening our theoretical frameworks, and using alternative methodological approaches would help all medical educators conduct better research.
Investing more time and resources in the study of earlier stages of program development—planning and piloting—might also improve our educational programs. We believe that many of the educational programs described in this literature did undergo iterative evolution, responding to feedback from learners and educators, as they were developed. However, the description of this iterative process is nearly absent in our publications. By incorporating these processes, publicly and explicitly, we could develop better programs. Perhaps more importantly, we would also better understand why they are effective, which in turn would help others learn from our work.
Second, the majority of studies were conducted without financial support, and many funded studies were conducted with internal funds (state, local, province, and private foundation funds). The process of obtaining financial support often sharpens the methodological rigor of studies as they are developed; it also allows more resources and expertise to be brought to the work. The paucity of substantial funding to support medical education research has undoubtedly contributed to the weakness of the literature as a whole.
Third, many of the incentives for creating and studying educational interventions live at the local level. Educators conduct work like this, in part, to promote their own programs, to show that their programs are innovative and effective, and to achieve academic benchmarks for promotion. Institutions often support such work for the same reasons: to show that they are innovative, and perhaps that they have an impact on the workforce of their community, region, or state. Medical educators studying their own programs search the previous literature for examples of what can be studied and published, which leads to a pattern in which studies of the same type are published over and over again.
Because many of the incentives to study curricula and policies are local, rather than national or international, the literature includes many case studies, and few large-scale comparative studies of multiple institutions. This suggests that national or international organizations need to promote and fund this work, with a particular focus on larger studies with innovative methodology.78 A substantial amount of work has been previously funded by the Health Resources and Services Administration HRSA, particularly through Title VII mechanisms,79 but this type of support has been contracting for more than a decade.80,81 The Affordable Care Act included a National Health Care Workforce Commission that was never funded. Establishing a funding source that could sponsor large-scale, high-quality studies of medical education, specifically focused on advancing the primary care workforce,11 could have a revolutionary impact on this body of work. This funding should also include training grants to support scholars focused on development of the future physician workforce.
To some extent, this local focus is simply the reality of our world: just as health care, fundamentally, is local, education in health care settings lives in the local context. At the same time, a focus on local curricula limits the scope of our scholarly work and our potential impact as a discipline of primary care educators. We are educating a generation of students in an interconnected, global world, and our educational and research methods must evolve to reflect this reality.
The review also reveals our bias toward studying aspects of the student experience that we, as faculty, intentionally create. Studies of curricula and programming abound, but relatively few examine institutional culture, community influences, and student-led experiences.
Consistent Use of Language and Definitions
Our review and synthesis of the literature was made more challenging and complex by the wide range of language used to describe the interventions, and by the frequent use of overlapping terms (Figure 2). We recommend that future researchers share a common language; this paper proposes definitions that may be useful (Table 1). Describing development of interventions using the proposed staging framework (Table 3) may also help us to better understand and learn from one another’s work.
Broadening the Focus of Scholarship
Beginning with a broad research question, we identified five key ways that institutional practices are described and defined in the literature, and four common methodologic approaches. Describing all the gaps in this literature would be an infinite task. Yet, consideration of the whole scope of this literature suggests additional feasible research questions, many of which have not been studied in a significant way. For example:
- As federal funding for medical education research (such as HRSA grants) has changed through time, how has this impacted student career choice?
- Do state legislative support and funding for family medicine departments correlate with the proportion of students entering family medicine?
- How does the availability of family medicine preceptors affect student experiences on their clerkships, and how does this, in turn, affect career decision-making?
- How do medical student peer networks influence career decision-making, and how can institutions support networks that promote primary care?
- What admissions committee structures, policies, and approaches are most useful in supporting the future primary care workforce?
- How can financial incentives, such as scholarships, most effectively support student choice of primary care?
- How can institutions best manage the backlash against primary care career choice when it is strongly promoted?
- How does student longitudinal exposure to primary care faculty throughout the medical school curriculum influence student choice?
- How does the bias against primary care manifest in our curricula, and how can we best overcome it?
Limitations
Although we have endeavored to use a robust methodology, some limitations should be acknowledged. First, the review excludes studies examining student perceptions of specific aspects of various specialties (such as lifestyle, income, or procedural orientation). Although these clearly influence student career choices, they are not directly shaped by medical schools, and were thus outside the scope of our research question. Second, the most recent search was conducted in June of 2019. We considered repeating the search, but had confidence that little published in the last 2 years would impact the general findings, which encompass 50 years of scholarship. The topic papers, published alongside this manuscript, have more contemporary searches and examine aspects of student career decision-making in greater depth.
This scoping review summarizes the areas of study and methodologic approaches of scholarship describing medical school practices to advance primary care specialty choice. The literature described encompasses 5 decades of research. In subsequent manuscripts, we describe topics of study in greater depth, using a series of narrative reviews to summarize our knowledge to date. We invite educational researchers to consider new topics and innovative approaches to future scholarship. We suggest institutions support, incentivize, and train educational researchers in interinstitutional, large-scale, outcomes-based scholarship that has potential meaningful impact. Finally, we challenge policy makers to consider building more robust funding mechanisms to support impactful medical education research focused on primary care.
*J.P.P. denotes author Julie P. Phillips. J.P. denotes author Jacob Prunuske.
Acknowledgments
Financial Support: This project was partially supported by a grant from the American Board of Family Medicine (ABFM) Foundation (J. Phillips, PI), and also partially by the Health Resources and Services Administration (HRSA) of the United States Department of Health and Human Services (HHS) under grant number D54HP23297, “Academic Administrative Units” (C. Morley, PI). This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by the ABFM, HRSA, HHS, or the US Government.
References
- Petterson SM, Liaw WR, Phillips RL Jr, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010-2025. Ann Fam Med. 2012;10(6):503-509. doi:10.1370/afm.1431
- Baicker K, Chandra A. Medicare spending, the physician workforce, and beneficiaries’ quality of care. Health Aff (Millwood). 2004;23(Suppl Web Exclusives):W4-184-97. doi:10.1377/hlthaff.W4.184
- Kravet SJ, Shore AD, Miller R, Green GB, Kolodner K, Wright SM. Health care utilization and the proportion of primary care physicians. Am J Med. 2008;121(2):142-148. doi:10.1016/j.amjmed.2007.10.021
- Petterson SM, Rabin D, Phillips RL Jr, Bazemore AW, Dodoo MS. Having a usual source of care reduces ED visits. Am Fam Physician. 2009;79(2):94.
- Chetty VK, Culpepper L, Phillips RL Jr, et al. FPs lower hospital readmission rates and costs. Am Fam Physician. 2011;83(9):1054.
- Jackson GL, Powers BJ, Chatterjee R, et al. The patient centered medical home. A systematic review. Ann Intern Med. 2013;158(3):169-178. doi:10.7326/0003-4819-158-3-201302050-00579
- Alexander JA, Markovitz AR, Paustian ML, et al. Implementation of patient-centered medical homes in adult primary care practices. Med Care Res Rev. 2015;72(4):438-467. doi:10.1177/1077558715579862
- Markovitz AR, Alexander JA, Lantz PM, Paustian ML. Patient-centered medical home implementation and use of preventive services: the role of practice socioeconomic context. JAMA Intern Med. 2015;175(4):598-606. doi:10.1001/jamainternmed.2014.8263
- Shi L, Starfield B, Kennedy B, Kawachi I. Income inequality, primary care, and health indicators. J Fam Pract. 1999;48(4):275-284.
- Phillips JP, Wendling A, Bentley A, Marsee R, Morley CP. Trends in US medical school contributions to the family physician workforce: 2018 update from the American Academy of Family Physicians. Fam Med. 2019;51(3):241-250. doi:10.22454/FamMed.2019.395617
- National Academies of Science, Engineering, and Medicine. Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care. Washington, DC: The National Academies Press; 2021.
- Biggs WS, Crosley PW, Kozakowski SM. Entry of US medical school graduates into family medicine residencies: 2012--2013. Fam Med. 2013;45(9):642-646.
- Erikson CE, Danish S, Jones KC, Sandberg SF, Carle AC. The role of medical school culture in primary care career choice. Acad Med. 2013;88(12):1919-1926. doi:10.1097/ACM.0000000000000038
- Bennett KL, Phillips JP. Finding, recruiting, and sustaining the future primary care physician workforce: a new theoretical model of specialty choice process. Acad Med. 2010;85(10)(suppl):S81-S88. doi:10.1097/ACM.0b013e3181ed4bae
- Meurer LN, Bland CJ, Maldonado G. The state of the literature on primary care specialty choice: where do we go from here? Acad Med. 1996;71(1):68-77. doi:10.1097/00001888-199601000-00020
- Reed VA, Jernstedt GC, Reber ES. Understanding and improving medical student specialty choice: a synthesis of the literature using decision theory as a referent. Teach Learn Med. 2001;13(2):117-129. doi:10.1207/S15328015TLM1302_7
- Valsangkar B, Chen C, Wohltjen H, Mullan F. Do medical school mission statements align with the nation’s health care needs? Acad Med. 2014;89(6):892-895. doi:10.1097/ACM.0000000000000241
- Chen C, Petterson S, Phillips RL, Mullan F, Bazemore A, O’Donnell SD. Toward graduate medical education (GME) accountability: measuring the outcomes of GME institutions. Acad Med. 2013;88(9):1267-1280. doi:10.1097/ACM.0b013e31829a3ce9
- Morley CP, Mader EM, Smilnak T, et al. The social mission in medical school mission statements: associations with graduate outcomes. Fam Med. 2015;47(6):427-434.
- Park Y, Ryan MH, Santen SA, Sabo R, Blondino C, Magee ML. Nurturing the student, sustaining the mission: 20 years of the international/inner-city/rural preceptorship program. Fam Med. 2019;51(10):823-829. doi:10.22454/FamMed.2019.358223
- Walker JH, Dewitt DE, Pallant JF, Cunningham CE. Rural origin plus a rural clinical school placement is a significant predictor of medical students’ intentions to practice rurally: a multi-university study. Rural Remote Health. 2012;12:1908-1908. doi:10.22605/RRH1908
- Campos-Outcalt D, Senf J. A longitudinal, national study of the effect of implementing a required third-year family practice clerkship or a department of family medicine on the selection of family medicine by medical students. Acad Med. 1999;74(9):1016-1020. doi:10.1097/00001888-199909000-00016
- Kost A, Morley C, Phillips J, Prunuske J, Kovar-Gough I, Sarenji T. The influence of rule modeling and mentoring on primary care career choice: a narrative synthesis of 30 years of research. Fam Med. 2022;54(7):555-563.
- Sairenji T, Kost A, Kovar-Gough I, Polverento M, Morley C, Phillips J. The impact of family medicine interest groups and student run free clinics on primary care career choice. Fam Med. 2022;54(7):531-535.
- Lee A, Erlich D, Wendling A, et al. The relationship between medical school clerkships and primary care specialty choice: a narrative review. Fam Med. 2022;54(7):564-571.
- Seehusen D, Phillips J, Prunuske J, Morley C, Polverento M, Kovar-Gough I. Institutional characteristics influencing medical student selection of primary care careers: a narrative review and synthesis. Fam Med. 2022;54(7):522-530.
- Nguyen M, Liaw W, Phillips J, et al. Impact of curricula and electives on primary care specialty choice: a narrative synthesis. Fam Med. 2022;54(7):572-577.
- Raleigh M, Seehusen D, Phillips J, et al. Influences of medical school admissions practices on primary care career choice. Fam Med. 2022;54(7):572-577.
- Ledford C, Guard E, Phillips J, Morley C, Prunuske J, Wendling A. How medical education pathways influence primary care specialty choice. Fam Med. 2022;54(7):512-521.
- Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi:10.1186/s12874-018-0611-x
- Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371-385. doi:10.1002/jrsm.1123
- Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and Explanation. Ann Intern Med. 2018;169(7):467-473. doi:10.7326/M18-0850
- Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Implement. 2021;19(1):3-10. doi:10.1097/XEB.0000000000000277
- Arksey H, O’Malley L; H A. L OM. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19-32. doi:10.1080/1364557032000119616
- Wijnen-Meijer M, Burdick W, Alofs L, Burgers C, ten Cate O. Stages and transitions in medical education around the world: clarifying structures and terminology. Med Teach. 2013;35(4):301-307. doi:10.3109/0142159X.2012.746449
- Mahood Q, Van Eerd D, Irvin E. Searching for grey literature for systematic reviews: challenges and benefits. Res Synth Methods. 2014;5(3):221-234. doi:10.1002/jrsm.1106
- Sirriyeh R, Lawton R, Gardner P, Armitage G. Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Pract. 2012;18(4):746-752. doi:10.1111/j.1365-2753.2011.01662.x
- Evans WD. How social marketing works in health care. BMJ. 2006;332(7551):1207-1210. doi:10.1136/bmj.332.7551.1207-a
- N KPRNL. Social Marketing: Improving the Quality of Life. Thousand Oaks, CA: Sage Publications; 2002.
- Brooker R, Hu W, Reath J, Abbott P. Medical student experiences in prison health services and social cognitive career choice: a qualitative study. BMC Med Educ. 2018;18(1):3. doi:10.1186/s12909-017-1109-7
- Elnicki DM, Halbritter KA, Antonelli MA, Linger B. Educational and career outcomes of an internal medicine preceptorship for first-year medical students. J Gen Intern Med. 1999;14(6):341-346. doi:10.1046/j.1525-1497.1999.00352.x
- Fournier GM, Henderson C. Incentives and physician specialty choice: a case study of Florida’s Program in Medical Sciences. Inquiry. 2005;42(2):160-170. doi:10.5034/inquiryjrnl_42.2.160
- Pfarrwaller E, Sommer J, Chung C, et al. Impact of interventions to increase the proportion of medical students choosing a primary care career: a systematic review. J Gen Intern Med. 2015;30(9):1349-1358. doi:10.1007/s11606-015-3372-9
- Dogbey GY, Collins K, Russ R, Brannan GD, Mivsek M, Sewell S. Factors associated with osteopathic primary care residency choice decisions. J Am Osteopath Assoc. 2018;118(4):225-233.
- Gatipon BB, Euans DW, Randall HM. Why graduates of the LSU School of Medicine, New Orleans choose primary care careers. J La State Med Soc. 1996;148(7):291-295.
- Kost A, Bentley A, Phillips J, Kelly C, Prunuske J, Morley CP. Graduating medical student perspectives on factors influencing specialty choice: an aafp national survey. Fam Med. 2019;51(2):129-136. doi:10.22454/FamMed.2019.136973
- Marple RI, Pangaro L, Kroenke K. Third-year medical student attitudes toward internal medicine. Arch Intern Med. 1994;154(21):2459-2464. doi:10.1001/archinte.1994.00420210097011
- Schafer S, Shore W, French L, Tovar J, Hughes S, Hearst N. Rejecting family practice: why medical students switch to other specialties. Fam Med. 2000;32(5):320-325.
- Kassebaum DG, Szenas PL. Factors influencing the specialty choices of 1993 medical school graduates. Acad Med. 1994;69(2):163-170. doi:10.1097/00001888-199402000-00027
- Burack JH, Irby DM, Carline JD, Ambrozy DM, Ellsbury KE, Stritter FT. A study of medical students’ specialty-choice pathways: trying on possible selves. Acad Med. 1997;72(6):534-541. doi:10.1097/00001888-199706000-00021
- Jordan J, Brown JB, Russell G. Choosing family medicine. What influences medical students? Can Fam Physician. 2003;49:1131-1137.
- Parker JE, Hudson B, Wilkinson TJ. Influences on final year medical students’ attitudes to general practice as a career. J Prim Health Care. 2014;6(1):56-63. doi:10.1071/HC14056
- Scott I, Wright B, Brenneis F, Brett-Maclean P, McCaffrey L. Why would I choose a career in family medicine?: reflections of medical students at 3 universities. Can Fam Physician. 2007;53(11):1956-1957.
- Vohra A, Ladyshewsky R, Trumble S. Factors that affect general practice as a choice of medical speciality: implications for policy development. Aust Health Rev. 2019;43(2):230-237. doi:10.1071/AH17015
- Rabinowitz HK, Diamond JJ, Markham FW, Santana AJ. Increasing the supply of rural family physicians: recent outcomes from Jefferson Medical College’s Physician Shortage Area Program (PSAP). Acad Med. 2011;86(2):264-269. doi:10.1097/ACM.0b013e31820469d6
- Haq C, Stearns M, Brill J, et al. Training in Urban Medicine and Public Health: TRIUMPH. Acad Med. 2013;88(3):352-363. doi:10.1097/ACM.0b013e3182811a75
- Kane KY, Quinn KJ, Stevermer JJ, et al. Summer in the country: changes in medical students’ perceptions following an innovative rural community experience. Acad Med. 2013;88(8):1157-1163. doi:10.1097/ACM.0b013e318299fb5d
- Bruno DM, Imperato PJ, Szarek M. The correlation between global health experiences in low-income countries on choice of primary care residencies for graduates of an urban US medical school. J Urban Health. 2014;91(2):394-402. doi:10.1007/s11524-013-9829-4
- Matthews C, Bagg W, Yielder J, Mogol V, Poole P. Does Pukawakawa (the regional-rural programme at the University of Auckland) influence workforce choice? N Z Med J. 2015;128(1409):35-43.
- Wendling AL, Phillips J, Short W, Fahey C, Mavis B. Thirty years training rural physicians: outcomes from the Michigan State University College of Human Medicine Rural Physician Program. Acad Med. 2016;91(1):113-119. doi:10.1097/ACM.0000000000000885
- MacDowell M, Glasser M, Hunsaker M. A decade of rural physician workforce outcomes for the Rockford Rural Medical Education (RMED) Program, University of Illinois. Acad Med. 2013;88(12):1941-1947. doi:10.1097/ACM.0000000000000031
- Eidson-Ton WS, Rainwater J, Hilty D, et al. Training medical students for rural, underserved areas: A rural medical education program in California. J Health Care Poor Underserved. 2016;27(4):1674-1688. doi:10.1353/hpu.2016.0155
- Wilkinson JE, Hoffman M, Pierce E, Wiecha J. FaMeS: an innovative pipeline program to foster student interest in family medicine. Fam Med. 2010;42(1):28-34.
- Campos-Outcalt D, Senf JH. Characteristics of medical schools related to the choice of family medicine as a specialty. Acad Med. 1989;64(10):610-615.
- Stine CC, Sheets KJ, Calonge BN. Association between clinical experiences in family practice or in primary care and the percentage of graduates entering family practice residencies. Acad Med. 1992;67(7):475-477. doi:10.1097/00001888-199207000-00014
- Whitcomb ME, Cullen TJ, Hart LG, Lishner DM, Rosenblatt RA. Comparing the characteristics of schools that produce high percentages and low percentages of primary care physicians. Acad Med. 1992;67(9):587-591. doi:10.1097/00001888-199209000-00009
- Tong STC, Phillips RL, Berman R. Is exposure to a student-run clinic associated with future primary care practice? Fam Med. 2012;44(8):579-581.
- Hays R, Bowles S, Brown T, Lawler A, Vickers J. The impact after 50 years of a new medical education programme with a regional workforce mission. Aust J Rural Health. 2017;25(6):332-337. doi:10.1111/ajr.12360
- Woolley T, Larkins S, Sen Gupta T. Career choices of the first seven cohorts of JCU MBBS graduates: producing generalists for regional, rural and remote northern Australia. Rural Remote Health. 2019;19(2):4438. doi:10.22605/RRH4438
- Phillips JP, Wendling AL, Fahey CA, Mavis BE. The effect of a community-based medical school on the state and local physician workforce. Acad Med. 2018;93(2):306-313. doi:10.1097/ACM.0000000000001823
- Osborn EH, O’Neil EH. “Bimodal” medical schools: excelling in research and primary care. Acad Med. 1996;71(9):941-949. doi:10.1097/00001888-199609000-00007
- Henderson MC, Hunt DK, Williams JW Jr. General internists influence students to choose primary care careers: the power of role modeling. Am J Med. 1996;101(6):648-653. doi:10.1016/S0002-9343(96)00334-8
- Block SD, Clark-Chiarelli N, Singer JD. Mixed messages about primary care in the culture of U.S. medical schools. Acad Med. 1998;73(10):1087-1094. doi:10.1097/00001888-199810000-00020
- Senf JH, Campos-Outcalt D, Watkins AJ, Bastacky S, Killian C. A systematic analysis of how medical school characteristics relate to graduates’ choices of primary care specialties. Acad Med. 1997;72(6):524-533. doi:10.1097/00001888-199706000-00020
- Stearns JA, Stearns MA, Glasser M, Londo RA. Illinois RMED: a comprehensive program to improve the supply of rural family physicians. Fam Med. 2000;32(1):17-21.
- Musham C, Chessman A. Changes in medical students’ perceptions of family practice resulting from a required clerkship. Fam Med. 1994;26(8):500-503.
- Park YS, Konge L, Artino AR Jr. The positivism paradigm of research. Acad Med. 2020;95(5):690-694. doi:10.1097/ACM.0000000000003093
- Buerhaus PI, Retchin SM. The dormant National Health Care Workforce Commission needs congressional funding to fulfill its promise. Health Aff (Millwood). 2013;32(11):2021-2024. doi:10.1377/hlthaff.2013.0385
- Morley CP, Cameron BJ, Bazemore AW. The impact of administrative academic units (AAU) grants on the family medicine research enterprise in the United States. Fam Med. 2016;48(6):452-458.
- Harrison B, Bazemore AW, Dodoo MS, Teevan B, Wittenburg H, Phillips RL Jr. Title VII’s decline: shrinking investment in the primary care training pipeline. Am Fam Physician. 2009;80(8):872.
- Heisler EJ. Health Resources and Services Administration (HRSA) FY2020 President’s Budget Request and Agency Funding History: In Brief. November 12, 2019. Accessed April 8, 2022. https://crsreports.congress.gov/product/pdf/R/R46001



There are no comments for this article.