The widening gap between urban and rural health outcomes is exacerbated by physician shortages that disproportionately affect rural communities.1-3 Residency training in rural and underserved settings has been shown to increase physicians’ sense of preparedness for and entry into rural practice.4-11 Recent data has suggested that rural graduate medical education (GME) increases the likelihood of rural practice for trainees of both urban and rural backgrounds. 7 Up to 45% of rural family medicine graduates enter rural practice, and trainees who spend more than 50% of graduate training in rural areas are five times more likely to enter rural practice. 4-7 Despite this impact, rural family medicine residencies comprise fewer than 15% of all programs and 11% of all family medicine training positions.4, 12 More rural residencies are needed for growth in the physician workforce to reach rural and underserved areas. 4-7 The federally funded Teaching Health Center Graduate Medical Education (THCGME) program supports community-based residencies sponsored by health centers or consortia, but not by academic institutions.13, 14 Recognizing the importance of academic institutions in building systems of health for vulnerable communities, community health center/academic medicine partnerships (CHAMPs) are proposed as a collaborative framework for expansion of academic primary care residencies into health centers, creating rural residencies outside of traditional Medicare or THCGME-funded models.15-17
BRIEF REPORTS
Ten-Year Outcomes: Community Health Center/Academic Medicine Partnership for Rural Family Medicine Training
Maria Gabriela Castro, MD | Caroline Roberts, MD | Emily M. Hawes, PharmD, BCPS, CPP | Evan Ashkin, MD | Cristen P. Page, MD, MPH
Fam Med. 2024;56(3):185-189.
DOI: 10.22454/FamMed.2024.400615
Background and Objectives: The widening gap between urban and rural health outcomes is exacerbated by physician shortages that disproportionately affect rural communities. Rural residencies are an effective mechanism to increase physician placement in rural and medically underserved areas yet are limited in number due to funding. Community health center/academic medicine partnerships (CHAMPs) can serve as a collaborative framework for expansion of academic primary care residencies outside of traditional funding models. This report describes 10-year outcomes of a rural training pathway developed as part of a CHAMP collaboration.
Methods: Using data from internal registries and public sources, our retrospective study examined demographic and postgraduation practice characteristics for rural pathway graduates. We identified the rates of postgraduation placement in rural (Federal Office of Rural Health Policy grant-eligible) and federally designated Medically Underserved Areas/Populations (MUA/Ps). We assessed current placement for graduates >3 years from program completion.
Results: Over a 10-year period, 25 trainees graduated from the two residency expansion sites. Immediately postgraduation, 84% (21) were in primary care Health Professional Shortage Areas (HPSAs), 80% (20) in MUA/Ps, and 60% (15) in rural locations. Sixteen graduates were >3 years from program completion, including 69% (11) in primary care HPSAs, 69% (11) in MUA/Ps, and 50% (5) in rural locations.
Conclusions: This CHAMP collaboration supported development of a rural pathway that embedded family medicine residents in community health centers and effectively increased placement in rural and MUA/Ps. This report adds to national research on rural workforce development, highlighting the role of academic-community partnerships in expanding rural residency training outside of traditional funding models.
Rural Training Pathway
North Carolina has the second largest rural population in the nation and the highest proportion of persons living in rural areas (33%); 92 of its 100 counties encompass Health Professional Shortage Areas (HPSAs), and 38 fall short of the minimum 1:1500 primary care provider per capita target.18-22 Given the effectiveness of rural residencies in physician placement, the University of North Carolina (UNC) Department of Family Medicine endeavored to expand its existing residency program through the addition of a rural pathway, aiming to increase postgraduation rural placement above a historical maximum rate of 25%. Expansion was limited by Medicare funding caps and ineligibility for THCGME funding as an academic institution. Therefore, the CHAMP framework was leveraged to formalize the relationship with a local community health center (CHC) network for collaborative program development. 23,24
Incremental Expansion
A rural pathway, developed through incremental expansion, added a total of 18 slots at two rural CHC training sites over a 10-year period.24 The training sites are in Prospect Hill, NC (unincorporated community, population 1,109, 24% living in poverty) and Siler City, NC (population 8,074, 26% living in poverty), each approximately 35 miles (45 minutes) from the academic center.25, 26 Each site hosts nine residents (three per year) who maintain a continuity practice throughout the 3 years of residency; all other training requirements are completed along with the larger residency cohort. In total, rural pathway residents spend 51% (18.3 months) of their residency training time in rural settings including the CHCs, a rural hospital with a maternity care center, and a migrant farmworker program.
This report describes 10-year practice outcomes of a nonseparately accredited rural training pathway developed as part of a CHAMP collaboration.
This study was approved by the UNC Institutional Review Board (#20-2162). Demographic and postgraduation practice characteristics for all graduates of the rural pathway since implementation (2012-2022) were obtained from internal registries, state medical board websites, and other public sources. Primary care was defined as practicing family medicine in the ambulatory setting. Designations of sites as primary care HPSAs, Medically Underserved Areas/Populations (MUA/Ps), and/or rural were determined using Rural Health Information Hub’s Am I Rural? tool.27-30 The Federal Office of Rural Health Policy (FORHP) definition of rural was selected to determine placement in areas eligible for federal grants. Rural-Urban Commuting Area (RUCA) and Rural-Urban Continuum Codes (RUCC) were evaluated to allow comparison with other measures of rurality. Current practice locations and designations were assessed for graduates at least 3 years from program completion.
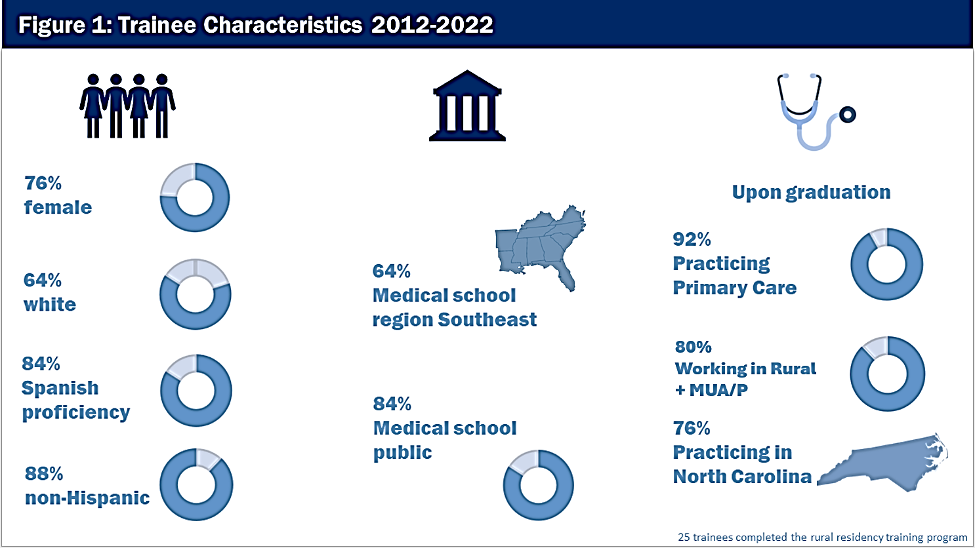
Over a 10-year period, the program recruited and trained a total of 25 family physicians at two sites: Prospect Hill CHC (RUCA 2.0, RUCC 8) and Siler City CHC (RUCA 7.0, RUCC 2). Among graduates, 76% (19) were female, 20% (5) Black/African American, 16% (4) Asian/Pacific Islander, and 12% (3) Hispanic; 72% (18) reported a rural background, and 84% (21) reported Spanish proficiency prior to residency. Eighty-four percent (21) attended a public medical school, and 64% (16) attended medical schools in the Southeast United States (Table 1, Figure 1).
|
Characteristics |
Number of graduates (N=25), n (%) |
|
|
Sex |
||
|
Female |
19 (76) |
|
|
Male |
6 (24) |
|
|
Race |
||
|
African American/Black |
5(20) |
|
|
White |
16 (64) |
|
|
Asian |
4 (16) |
|
|
Ethnicity |
||
|
Hispanic/Hispanic Heritage |
3 (12) |
|
|
Non-Hispanic |
22 (88) |
|
|
Spanish proficiency |
||
|
Yes |
21 (84) |
|
|
No |
4 (16) |
|
|
Rural background |
||
|
No |
18 (72) |
|
|
Yes |
7 (28) |
|
|
Medical school |
||
|
Public |
21 (84) |
|
|
Private |
4 (16) |
|
|
Medical school region |
||
|
Southeast |
16 (64) |
|
|
Northeast |
4 (16) |
|
|
Midwest |
4 (16) |
|
|
West |
1 (4) |
|
Immediate Postgraduation Practice
Upon graduation, 92% (23) of graduates entered primary care practice. Among all practice sites, 84% (21) were primary care HPSAs, 80% (20) MUA/Ps, and 60% (15) rural. Most graduates (76%, 19) remained in-state. Fifteen graduates (60%) joined the training sites: 10 as part of fellowship training and 5 as rural residency faculty (Table 2).
|
|
1 year after graduation, n (%) |
3 years after graduation, n (%) |
|---|---|---|
|
Total number of graduates |
25 |
16 |
|
Practice type |
||
|
Academic medical center |
5(20) |
3 (19) |
|
Public/nonprofit |
15(60) |
7 (44) |
|
Private |
5(20) |
5 (31) |
|
Critical access hospital |
0 |
1 (6) |
|
Practice state |
|
|
|
In-state (North Carolina) |
19(76) |
12 (75) |
|
Out-of-state |
6(24) |
4 (25) |
|
Practice designation |
|
|
|
HPSA |
21(84) |
11 (69) |
|
MUA/P |
20(80) |
11 (69) |
|
Rural |
|
|
|
FORHP |
15(60) |
9 (50) |
|
RUCC ≥4 |
11(44) |
6 (38) |
|
RUCA ≥4.0 |
7(28) |
5 (31) |
|
Practice scope |
|
|
|
Primary care |
23(92) |
15 (94) |
|
Prenatal care |
17(68) |
10 (63) |
|
Obstetrics |
8(32) |
5 (31) |
|
Surgical obstetrics |
1(4) |
3 (19) |
|
Inpatient |
11(44) |
8 (50) |
|
|
|
|
Abbreviations: HPSA, Health Professional Shortage Area; MUA/P, MedicallyUnderserved Areas/Populations, FORHP, Federal Office of Rural Health Policy; RUCC, Rural-Urban Continuum Codes; RUCA, Rural-Urban Commuting Area
Current Practice Characteristics
At the time of this study, 16 graduates were >3 years from completion of training. Among them, 94% (15) were practicing primary care, 69% (11) were in primary care HPSAs, 69% (11) in MUA/Ps, and 50% (9) in rural locations. Twelve graduates (75%) remained in North Carolina, including 5 (31%) as faculty at the training sites (Table 2).
By embedding family medicine residents into CHCs and a rural hospital, this CHAMP collaboration supported development of a rural pathway within an accredited program and effectively increased rural and medically underserved practice placement following residency. Until the Consolidated Appropriations Act of 2021 (CAA), rural hospitals or partnering urban hospitals could qualify for Medicare GME funding only by participating in separately accredited rural residencies, resulting in financial constraints for lower-resourced facilities.31 However, the new CAA provision for the definition of Rural Track Program (RTP) to encompass all programs (separately accredited or not) where residents spend time in both urban and rural settings but greater than 50% of training time in rural settings has created new opportunities for rural GME expansion.32 Furthermore, CAA supports cap expansion for urban hospitals with existing RTPs if they develop them in the same specialty at new locations. These changes have direct implications for urban programs looking to establish new training in rural health facilities, as in the aforementioned case.
The success of this program is founded on the academic-community collaboration that leveraged the strengths of each partner to achieve the outcomes of the CHAMP partnership to equip physicians to practice in medically underserved settings years after graduation. Study limitations included a single program, small sample, and potential effect of factors such as rural background known to influence rural placement. Numerous definitions of rural exist, each with its own advantages and disadvantages. This analysis included FORHP, RUCA, and RUCC to allow for comparison with other measures of rurality.7, 30
This report can inform development of other programs by encouraging rural health facilities, including CHCs and rural hospitals, to consider partnerships with academic institutions to develop rural pathways and newly instituted RTPs. 33 Private and state start-up grants contributed to the launch of this rural pathway,24 and federal start-up grants are available through programs such as the Rural Residency Planning and Development and Teaching Health Center Planning and Development programs. 24, 34, 35, 36 This case affirms the enduring need to improve rural GME funding and offers a pathway for THCGME-ineligible institutions.
In conclusion, this report adds to existing evidence of the impact of rural training on future practice and highlights the role of academic-community partnerships in expanding GME into rural and underserved areas.
Presentations
Brief descriptions of our program and plan for evaluation were included as part of the following presentations:
-
Roberts C, Castro MG, Brown M, Smith J, DeVries A. Rural Underserved Track’s Influence on Post Residency Practice. Peer presentation adapted to virtual session. Society of Teachers of Family Medicine, Annual Spring Conference, August 2020.
-
Castro MG, Roberts C. Rural Program Development Through a Community Health Center and Academic Medical Partnership: Outcomes 4 years Post-Implementation. Rural Residency Planning & Development Program–Technical Assistance Program Webinar. May 10, 2022.
Financial Support
Health Resources & Services Administrations Primary Care Training Enhancement Award #D58HP37585 (7/1/2020-6/30/2025); UNC Health support for Chatham Residency; Blue Cross Blue Shield of North Carolina Foundation; The Duke Endowment; Golden Leaf Foundation, Kate B. Reynolds Charitable Trust.
References
-
Gong G, Phillips SG, Hudson C, Curti D, Philips BU. Higher US rural mortality rates linked to socioeconomic status, physician shortages, and lack of health insurance. Health Aff (Millwood). 2019;38(12):2,003-2,010. doi:10.1377/hlthaff.2019.00722
-
Engel-Smith L. Rural-urban divide continues to widen, report finds. North Carolina Health News. November 18, 2019. Accessed September 19, 2023. https://www.northcarolinahealthnews.org/2019/11/18/rural-urban-divide-widens-cdc-finds
-
Pender J, Hertz T, Cromartie J, Farrigan T. Rural America at a Glance, 2019 Edition. US Department of Agriculture, Economic Research Service; November 2019. Economic Information Bulletin No. 212.
-
Russell DJ, Wilkinson E, Petterson S, Chen C, Bazemore A. Family medicine residencies: how rural training exposure in GME is associated with subsequent rural practice. J Grad Med Educ. 2022;14(4):441-450. doi:10.4300/JGME-D-21-01143.1
-
Hawes EM, Fraher E, Crane S, et al. Rural residency training as a strategy to address rural health disparities: barriers to expansion and possible solutions. J Grad Med Educ. 2021;13(4):461-465. doi:10.4300/JGME-D-21-00274.1
-
Schmitz D. The role of rural graduate medical education in improving rural health and health care. Fam Med. 2021;53(7):540-543. doi:10.22454/FamMed.2021.792533
-
Patterson DG, Shipman SA, Pollack SW, et al. Growing a rural family physician workforce: the contributions of rural background and rural place of residency training. Health Serv Res. 2023;1475-6773.14168. doi:10.1111/1475-6773.14168
-
Pollack SW, Andrilla CHA, Peterson L, et al. Rural versus urban family medicine residency scope of training and practice. Fam Med. 2023;55(3):162-170. doi:10.22454/FamMed.2023.807915
-
Phillips RL Jr, George BC, Holmboe ES, Bazemore AW, Westfall JM, Bitton A. Measuring graduate medical education outcomes to honor the social contract. Acad Med. 2022;97(5):643-648. doi:10.1097/ACM.0000000000004592
-
United States Government Accountability Office. Graduate Medical Education: Programs and Residents Increased During Transition to Single Accreditor; Distribution Largely Unchanged. Report to Congressional Requesters, GAO-21-329. April 2021. Accessed September 20, 2023. https://www.gao.gov/assets/gao-21-329.pdf
-
Mullan F, Chen C, Steinmetz E. The geography of graduate medical education: imbalances signal need for new distribution policies. Health Aff (Millwood). 2013;32(11):1,914-1,921. doi:10.1377/hlthaff.2013.0545
-
Meyers P, Wilkinson E, Petterson S, et al. Rural workforce years: quantifying the rural workforce contribution of family medicine residency graduates. J Grad Med Educ. 2020;12(6):717-726. doi:10.4300/JGME-D-20-00122.1
-
Strasser JH, Jewers MM, Kepley H, Chen C, Erikson C, Regenstein M. A mixed-methods study of teaching health center residents’ experiences of mentorship, career planning, and postresidency practice environments. Acad Med. 2022;97(1):129-135. doi:10.1097/ACM.0000000000004419
-
Davis CS, Roy T, Peterson LE, Bazemore AW. Evaluating the teaching health center graduate medical education model at 10 years: practice-based outcomes and opportunities. J Grad Med Educ. 2022;14(5):599-605. doi:10.4300/JGME-D-22-00187.1
-
Rieselbach RE, Crouse BJ, Neuhausen K, Nasca TJ, Frohna JG. Academic medicine: a key partner in strengthening the primary care infrastructure via teaching health centers. Acad Med. 2013;88(12):1,835-1,843. doi:10.1097/ACM.0000000000000035
-
Rieselbach RE, Epperly T, Friedman A, et al. A new community health center/academic medicine partnership for Medicaid cost control, powered by the mega teaching health center. Acad Med. 2018;93(3):406-413. doi:10.1097/ACM.0000000000001901
-
Fraher EP, Lombardi B, Brandt B, Hawes E. Improving the health of rural communities through academic-community partnerships and interprofessional health care and training models. Acad Med. 2022;97(9):1,272-1,276. doi:10.1097/ACM.0000000000004794
-
US Census Bureau. Demographic profile and demographic and housing characteristics. 2020. Accessed September 27, 2023. https://data.census.gov/table?g=040XX00US37&d=DEC+Demographic+Profile
-
Beck Dallaghan GL, Spero JC, Byerley JS, Rahangdale L, Fraher EP, Steiner B. Efforts to recruit medical students from rural counties: a model to evaluate recruitment efforts. Cureus. 2021;13(8):e17464. doi:10.7759/cureus.17464
-
Campbell HA, Tilson HH Jr. Outcomes of NC Medical School Graduates: How Many Stay in Practice in NC, in Primary Care, and in High Needs Areas? 2022.
-
Fraher EP, Spero JC. The State of the Physician Workforce in North Carolina: Overall Physician Supply Will Likely Be Sufficient but Is Maldistributed by Specialty and Geography. University of North Carolina Chapel Hill, The Cecil G. Sheps Center for Health Services Research; August 2015. Accessed September 27, 2023. https://www.shepscenter.unc.edu/wp-content/uploads/2015/08/MedicalEducationBrief-ShepsCenter-August20151.pdf
-
Petterson S, Cai A, Moore M, Bazemore A. North Carolina: projecting primary care physician workforce. Robert Graham Center; September 2013. Accessed September 28, 2023. https://www.graham-center.org/content/dam/rgc/documents/maps-data-tools/state-collections/workforce-projections/North%20Carolina.pdf
-
Ashkin E, Devries A. Spotlight on the safety net: creation of a family medicine residency track in care of the underserved: a collaboration between the University of North Carolina Department of Family Medicine and Piedmont Health Services. N C Med J. 2014;75(1):81-82. doi:10.18043/ncm.75.1.81
-
Ashkin EA, Newton WP, Toomey B, Lingley R, Page CP. Cost of incremental expansion of an existing family medicine residency program. Fam Med. 2017;49(7):544-547. https://www.stfm.org/familymedicine/vol49issue7/Ashkin544
-
North Carolina Institute of Medicine. Caswell County: North Carolina health profile. Accessed June 29, 2023. https://nciom.org/counties/caswell-county
-
US Census Bureau. Quickfacts Siler City town, North Carolina. July 2022. Accessed June 29, 2023. https://www.census.gov/quickfacts/fact/table/silercitytownnorthcarolina,NC/PST045222
-
Health Resources & Services Administration, US Department of Health and Human Services. HPSA Find. Accessed September 28, 2023. https://data.hrsa.gov/tools/shortage-area/hpsa-find
-
Longenecker R. Rural medical education programs: a proposed nomenclature. J Grad Med Educ. 2017;9(3):283-286. doi:10.4300/JGME-D-16-00550.1
-
Rural Health Information Hub. Am I Rural? tool. Accessed September 28, 2023. https://www.ruralhealthinfo.org/am-i-rural
-
Long JC, Delamater PL, Holmes GM. Which definition of rurality should I use? the relative performance of 8 federal rural definitions in identifying rural-urban disparities. Med Care. 2021;59:S413-S419. doi:10.1097/MLR.0000000000001612
-
Hawes EM, Holmes M, Fraher EP, et al. New opportunities for expanding rural graduate medical education to improve rural health outcomes: implications of the Consolidated Appropriations Act of 2021. Acad Med. 2022;97(9):1,259-1,263. doi:10.1097/ACM.0000000000004797
-
Accreditation Council for Graduate Medical Education. Rural track program designation. Accessed September 28, 2023. https://www.acgme.org/initiatives/medically-underserved-areas-and-populations/rural-tracks
-
Page CP, Chetwynd E, Zolotor AJ, Holmes GM, Hawes EM. Building the clinical and business case for opening maternity care units in critical access hospitals. NEJM Catal. 2021;2(5):CAT.21.0027. doi:10.1056/CAT.21.0027
-
Rural graduate medical education. Accessed September 28, 2023. https://www.ruralgme.org
-
Health Resources & Services Administration. Teaching health center planning and development program. Accessed September 28, 2023. https://www.hrsa.gov/grants/find-funding/HRSA-23-015
-
Health Resources & Services Administration. Rural residency planning and development (RRPD) program. Accessed June 29, 2023. https://www.hrsa.gov/rural-health/grants/rural-health-research-policy/rrpd
Lead Author
Maria Gabriela Castro, MD
Affiliations: Maria Gabriela Castro, Department of Family Medicine, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC
Co-Authors
Caroline Roberts, MD - Department of Family Medicine, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC | Piedmont Health Services at Prospect Hill Community Health Center, Prospect Hill, NC
Emily M. Hawes, PharmD, BCPS, CPP - Department of Family Medicine, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC | University of North Carolina Eshelman School of Pharmacy, Chapel Hill, NC
Evan Ashkin, MD - Department of Family Medicine, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC | Piedmont Health Services at Prospect Hill Community Health Center, Prospect Hill, NC
Cristen P. Page, MD, MPH - Department of Family Medicine, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC
Corresponding Author
Maria Gabriela Castro, MD
Correspondence: Maria Gabriela Castro, Department of Family Medicine, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC
Email: gabriela_castro@med.unc.edu
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.