Background and Objectives: Despite the efforts of many organizations to increase the volume of rural health care providers, rural communities continue to experience a shortage of physicians. To address this shortage, more information is needed as to how specific factors contribute to family physicians’ choice to purse rural full-spectrum practice.
Methods: Interviews with 21 key informants guided a grounded theory analysis around the question of “What factors contribute to the decision to, and maintenance of, practicing full-spectrum rural medicine?”
Results: Analysis revealed two categories of factors that influenced choice of scope and maintenance of scope across a career: contextual and developmental factors. Contextual factors included the national health care landscape, the local setting, and personal factors. The developmental factors pertained to the point in the physician’s career, and include preprofessional envisioned scope, current scope, and ideal future scope of practice.
Conclusions: Results describe how a rural physician’s scope of practice generally narrows as her/his career progresses. The results elaborate on how the larger health care landscape, local community, and personal factors all intersect to inform a physician’s decision to pursue and/or continue practice. Results of the study were consistent with preexisting literature, but provide additional depth and suggest a theoretical relationship among factors.
Health care in rural communities is confronted with a constant shortage of physicians.1 While nearly one-fifth of the US population resides in rural areas, only nine percent of US physicians practice in these same rural communites.1 This shortage persists despite the efforts of many medical schools, governmental groups, and health care agencies to identify and train medical students for rural health care practice.2-4
A small number of matriculating medical students plans to practice in a rural setting; even fewer of these medical students complete their residency in a rural setting.1,4 Rural communities lack many resources, which in turn negatively impacts patient health, health care access, and physician satisfaction. It has been well documented that individuals residing in rural communities experience exacerbated health issues, requiring a higher level of health care and physician involvement. 5,6
Many physicians contemplating a rural practice fear being overworked by these increased patient needs. Furthermore, the unique rural health care infrastructure may also present a challenge to physicians.5-7 In rural areas, physician reimbursement, both in private practices and hospitals, is lower and often delayed, creating more stress for the physician.5 All of these barriers decrease the likelihood of a physician’s choice to practice rural medicine. This creates a less attractive environment for medical specialists in which to practice, and an increased need for full-spectrum physicians who are competent in many different parts of patients’ health care.
This demand for full-spectrum health care providers contrasts with the growing trend of physicians narrowing their scope of practice.5 Narrowing the scope of practice is a phenomenon in which a physician chooses, often as a response to the demands of a specific community, a specified field of practice narrower than the one in which the physician was originally trained. This can result in a decrease of knowledge and practice application for specified fields of practice, along with many other consequences. Evidence for this phenomenon is based on a research study of 13,884 family physicians taking the American Board of Family Medicine Maintenance of Certification for Family Physicians Examination. The researchers compared physicians taking the exam for the first time to those retaking it to recertify their medical competence. Results of the study documented a significant decrease in intent to practice many aspects of full-spectrum family medicine. For example, intent to practice obstetric medicine dropped from 23.7% to 7.7%, inpatient care dropped from 54.9% to 33.6%, and prenatal care dropped from 50.2% to 9.9%.5 An official cause for this phenomenon is undetermined, but potential contributing factors include training, individual preference, lack of insurance reimbursement, employer-employee contract margins, and time constraints.
Many researchers, attempting to ameliorate the lack of rural physicians, have identified predictive factors of eventual rural practice of medical students (ie, individuals raised in a rural environment, plan to practice in a rural setting, and those who have training experience in a rural residency).5,7-10 Some medical school programs have utilized these predictive factors to build specific rural medicine training programs.2,3,8 Furthermore, trainees in rural residency programs are three times more likely to practice in rural areas, compared to other residency programs.11 Although the barriers to rural health care improvement are persistent and pervasive, efforts toward funneling more physicians into these communities have demonstrated moderate success.5
Despite the success of the aforementioned programs, much is still unknown about how and why rural full-spectrum physicians persist in their practice. The purpose of this study is to identify factors that contribute to family physicians’ choice in pursuing rural full-spectrum practice. Furthermore, through the analysis of qualitative interviews with physicians from multiple stages of their career, this study organizes these factors into a cohesive model that describes the decision-making process to continue practicing full-spectrum rural medicine.
This study utilized grounded theory as the basis for design. Grounded theory is a process that guides the creation of new theories.12 Developed as a primarily qualitative methodology, grounded theory is inductive in nature, in that the aim of the study is not to test a particular hypothesis, but rather to create a hypothesis (ie, the theory). Using a grounded theory approach allows the researchers to not only consider which factors influence the decision to pursue rural full-spectrum medicine, but also to understand the relationship among those factors. This understanding leads to the organization of these factors into a cohesive theoretical model.
Grounded theory utilizes key informants from similar situations applying similar problem-solving techniques to develop a theoretical model. The question driving our inquiry and analysis was “What factors contribute to the decision to, and maintenance of practicing full-spectrum rural medicine?” Thus, we identified “key informants” as individuals who began their residency with the intent of practicing full-spectrum rural medicine. For the purposes of this study, we utilized the US Census Bureau’s definition of “rural” as “all population, housing, and territory not included within an urban area. Typically this includes all areas that are not in or near cites of 50,000 or more inhabitants.”13 Participants were also welcome to define this term how they saw fit. Furthermore, researchers defined “full-spectrum” as a practice that includes many or all the domains that a family physician’s scope of practice can include as outlined by he American Academy of Family Physicians: clinical/outpatient, inpatient, urgent and emergency care, maternity care, sports medicine, public health, international medicine, wilderness medicine, procedures, education, and research.14 Again, participants were welcome to define these terms as they saw fit. Participants in this study were recruited through emails to residency programs that self-identified as training sites for rural full-spectrum family physicians. Given our interest in the decision-making process over time, recruited participants were grouped into three different categories: those in their third year of residency, those 4 to 10 years post-residency, and those more than 10 years post-residency. Participant selection criteria included having practiced in full-spectrum family medicine in one of the three mentioned time frames, and agreeing to a 10 to 25-minute interview.
Prior to the interview, participants were presented with informed consent outlining the research study. Prior to the interviews, the research was reviewed and provided an IRB exemption from the St Mary’s Hospital Institutional Review Board in Grand Junction, CO. Consenting participants then took part in a phone interview. We created an interview guide that consisted of six base questions and follow-up questions to clarify and expand on key themes. The guide was based on interview guides from similar grounded theory studies, with the intent of balancing the needs of requesting similar data from all key informants while allowing the interviewer to pursue potential themes as they emerged. The six questions and subquestions were:
- When you were applying for residency, was it your intent to practice full-spectrum rural family medicine at that time? What experiences and values from life before residency would help me to understand how you made this decision?
- Please describe your career as a family physician, starting with residency and including the places you’ve practiced and the scope of practice at each point.
- Now, let’s go back and look at those practice locations and your scope of practice so I can understand what factors affected those decisions. How would you describe the emphasis of your residency (or later practice)? By the end of your time there, how had your intent regarding future scope of practice and preferred setting changed? What factors or events led to any changes in those decisions that occurred during residency (or later practice setting)?
- Looking forward, do you foresee changing your scope of practice? If so, why and how?
- In an ideal world, what supports or other factors would have been helpful in maintaining broad-spectrum, rural practice?
- Looking back at your career, how do you feel about the changes in your scope of practice and your current practice?
The interviews lasted from 10 to 25 minutes. Phone interviews were conducted, audio recorded, transcribed, and then coded in NVivo 10 software for data analysis.15 Interviews were conducted in a three-stage process, with each consecutive stage allowing for further refinement of the research questions and interview procedure. The first stage included three interviews and focused on creating the protocol and building interviewer consistency. The second stage included 13 interviews. After these interviews, researchers designated valuable themes and constructed their initial theoretical model. The third stage consisted of five interviews and focused on following up on themes that were identified in the first two stages and further refinement with the developed model. Interviews were conducted by one or more of the researchers. Coding and analysis of the data were conducted successively to direct exploration of concepts in subsequent interviews and to further model development. Coding disagreement was resolved through team discussion until unanimous decision was obtained.
Participants included 21 “key informants,” or individuals who stated that they started residency with the intent of practicing full-spectrum, rural family medicine. Nine identified as male, and 12 identified as female. Eight were still within their third year of residency, nine were less than 10 years out of residency, and more than 10 years out of residency. At the time of the interviews, 18 practiced in rural or semirural areas, and three practiced in urban areas. They represented states from across the United States including Alaska, Alabama, California, Colorado, Maine, Montana, Oregon, and Utah.
The coding and analysis of participant interview transcripts identified two overarching categories of factors that influenced choice of scope and maintenance of scope across a career: contextual and developmental factors. Contextual factors were external elements of the individual’s life that influenced their practice considerations. Contextual factors noted by participants include the national health care landscape, the local setting, and personal factors. The developmental factors pertained to the point in the physician’s career and include preprofessional envisioned scope, current scope, and ideal future scope.
Regarding developmental stage, our key informants described envisioning a very broad scope before entering residency, delimiting scope in their current position, and envisioning continuing to narrow scope as they move toward retirement. Regarding the context, some influences on scope of practice are at the national and regional level (eg, national policy, insurance, malpractice, major trends across time), some occur at the local level (eg, hospital policy, relationships with specialists, local needs), and some at the personal level (eg, preferences among the areas of scope, demands of family and life). Participants stated that there is limited opportunity to reclaim areas of scope once they have been let go, but other areas for growth open with advancement (eg, opportunities for leadership, taking on new projects).
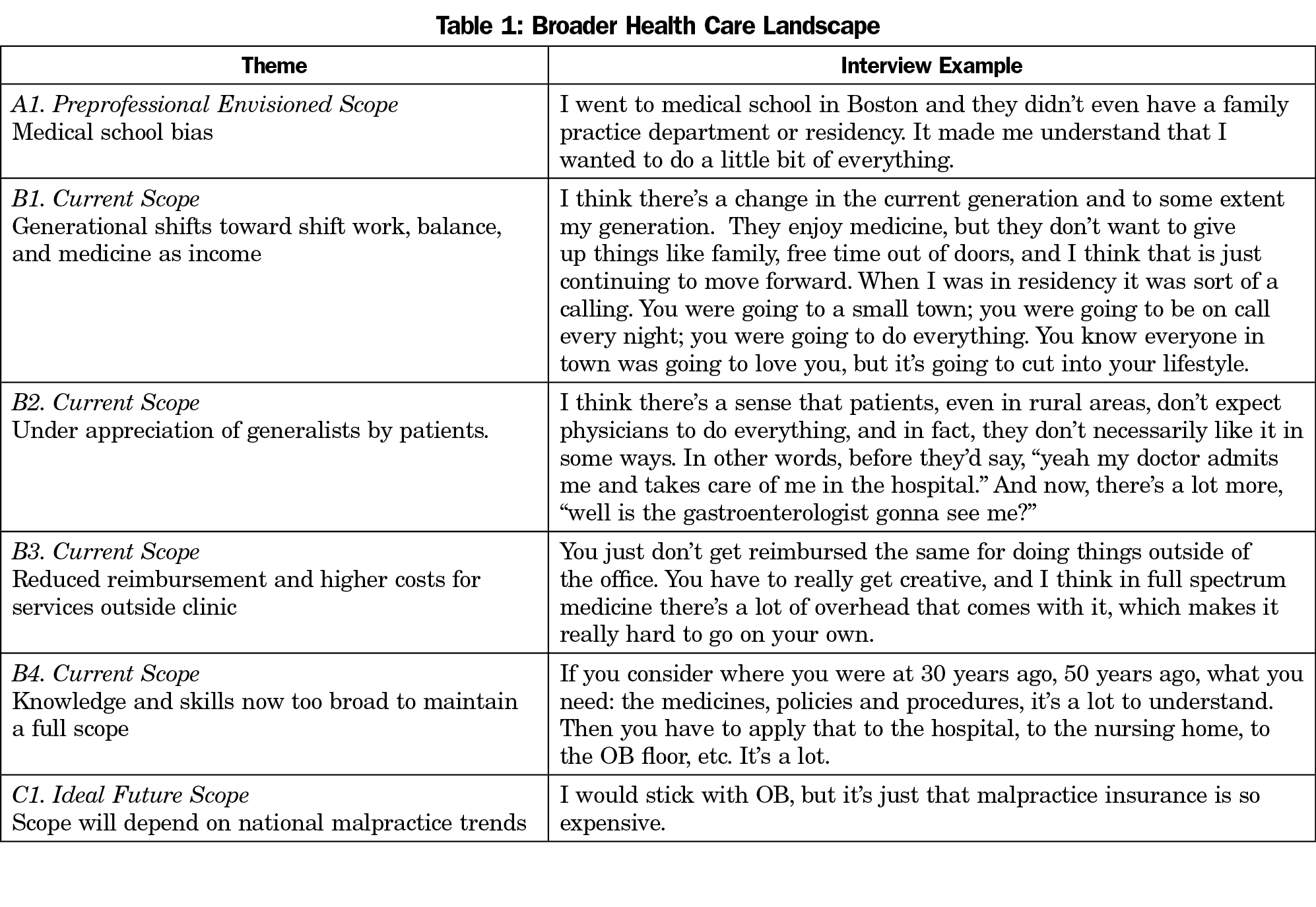
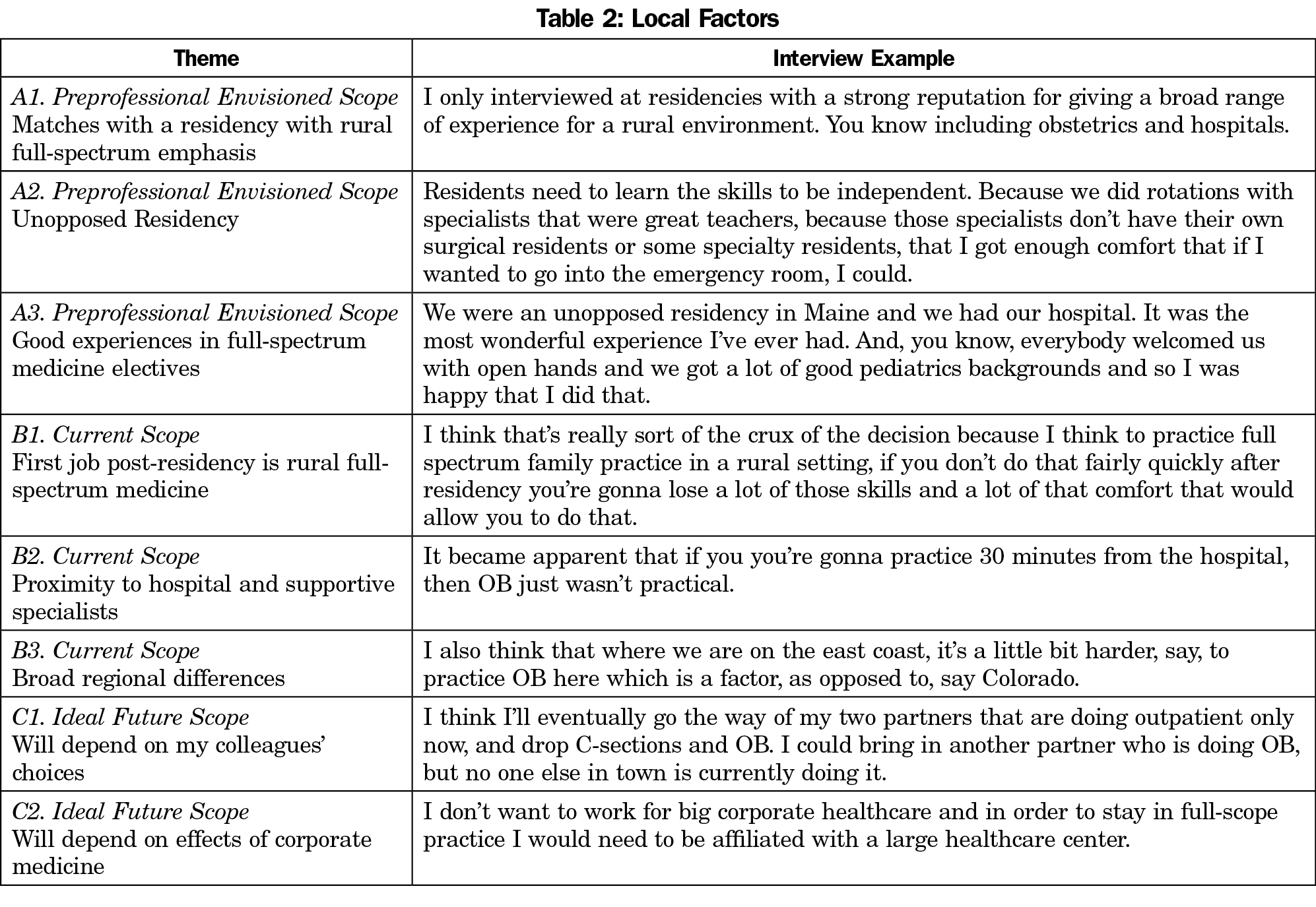
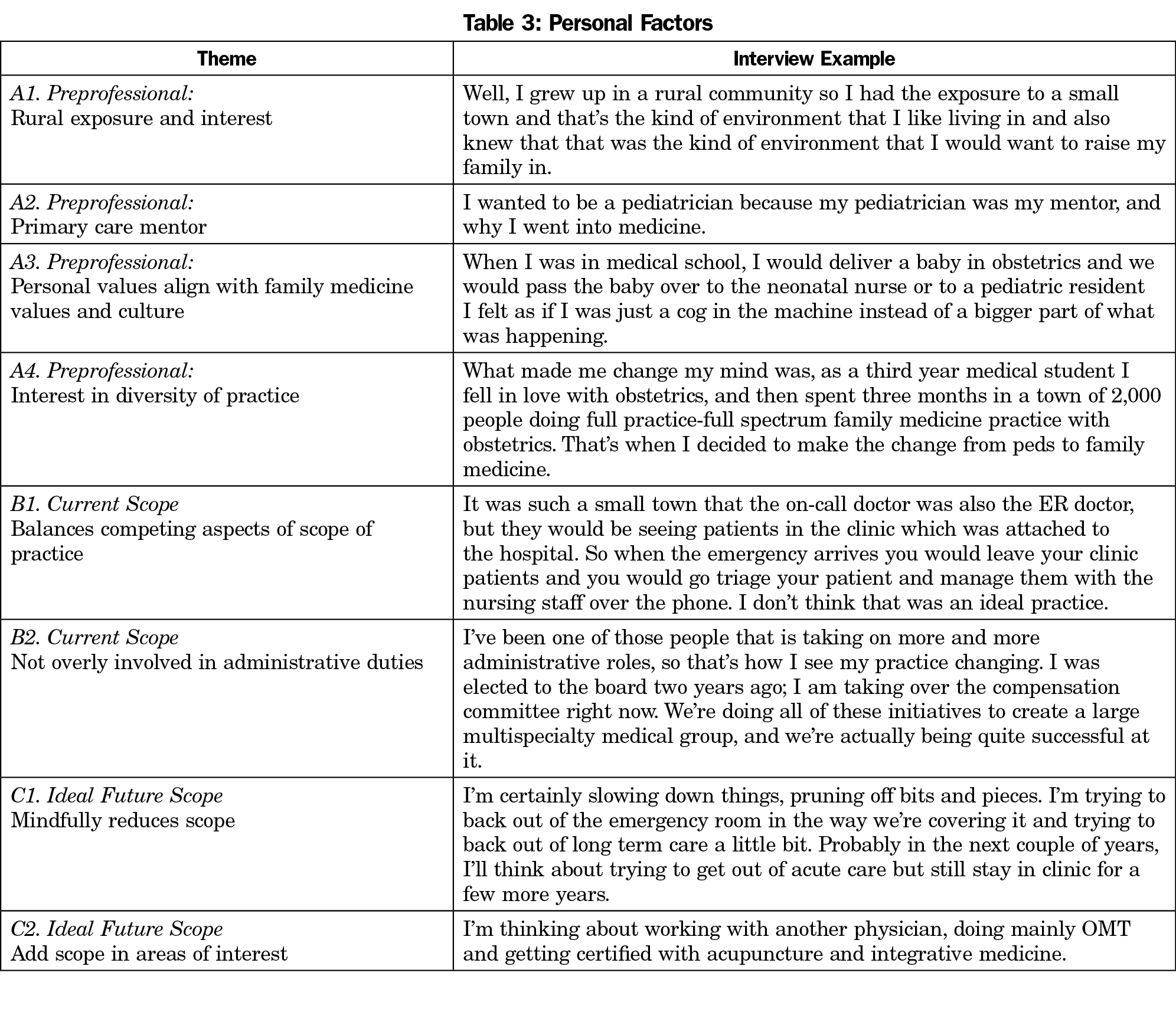
The five themes identified within the broader health care landscape describe policies and generational shifts in health care that affect physicians nationwide (Table 1). These factors are mostly external to the individual. The eight themes that comprise local factors are also external contributors that modify the desire and feasibility to pursue rural full-spectrum medicine in the physician’s locale (Table 2). Seven themes group together as personal factors. These are experiences and internal motivators that affect the decision to pursue rural full-spectrum medicine (Table 3). The broader health care landscape influences the contextual factors, which in turn influence the personal factors.
Results from the current study indicate that a physician’s scope of practice generally narrows as her/his career progresses, moving toward larger health systems and clinical medicine and away from hospitals, emergency departments, and specialization areas (ie, obstetrics). However, with this narrowing of their scope of practice, most physicians mindfully retain at least one area outside of ambulatory medicine. The vast majority of key informants reported feeling satisfied with their choice of family medicine and their current scope of practice. They describe large shifts in their scope across a career, but took satisfaction in their autonomy to make these changes at their pace and level of readiness.
The data presented here is largely supported by the preexisting literature, but provides additional richness and personal perspectives to this field of study. Results of the present study would be useful at all levels of advocacy for full-spectrum and rural family medicine services. Medical schools may consider these experiences in screening applicants and guiding students toward family medicine. They might consider adding discussion about how a varied level of factors may influence a student’s decision, giving them an opportunity to be intentional about their future practice setting. Residencies could benefit from identifying curricular and social elements that would encourage their trainees to matriculate to full-spectrum practice. Local communities and health care systems can use these experiences in recruiting family physicians. Decision-makers can propose laws and policies that support family physicians in maintaining full-spectrum rural practice.
This research suggests a number of implications for training programs and physicians who wish to practice rural, full-spectrum family medicine. For residencies, there would be a benefit to modeling an environment conducive to rural, full-spectrum family medicine. This would include a daily routine similar to the eventual practice environment, productive relationships with other specialties, and promoting positive experiences in a variety of rural and/or full-spectrum environments.
For physicians practicing in rural areas, there seems to be a benefit from continually reassessing the evolving needs of the community, the local health care system, and the preferences of the family physician. Many key informants described seemingly unsustainable demands on their time and expertise. In urban areas, these pressures can be addressed through narrowing scope and moving to shift work. Based on our research, these same trends are also occurring in rural areas, and none of our key informants described a yearning to return to the “old ways.”
The limitations of this research stem from research considerations inherent in grounded theory. That is, our sample was comparatively small and lacked a comparison group. It is impossible to know if the sample represents the perspectives of the entire population of family physicians who envisioned a career in full-spectrum and rural practice. However, we are confident that our methodology adheres to standards that are typical for grounded theory.
As is the goal of much theoretical research, this model provides a framework for other studies to develop workable hypotheses. A first step would be to replicate this research on a larger group of similar participants with differing methodology. As this study is mostly retrospective, it would be informative to test the model (ie, the new hypothesis) in a prospective study to verify whether the interventions that address the identified themes result in more family physicians adopting and sustaining a full-scope practice.
Acknowledgments
We presented this research at the Society of Teachers of Family Medicine Annual Spring Conference in Orlando, FL, April 25-29, 2015.
References
- Rosenblatt RA, Schneeweiss R, Hart LG, Casey S, Andrilla CHA, Chen FM. Family medicine training in rural areas. JAMA. 2002;288(9):1063-1064.
https://doi.org/10.1001/jama.288.9.1063.
- Trickett-Shockey AK, Wilson CS, Lander LR, et al. A study of rural upbringing and education on the intent of health professional students to work in rural settings. Int J Med Educ. 2013;4:18-25.
https://doi.org/10.5116/ijme.50f1.48cf.
- Kane KY, Quinn KJ, Stevermer JJ, et al. Summer in the country: changes in medical students’ perceptions following an innovative rural community experience. Acad Med. 2013;88(8):1157-1163.
https://doi.org/10.1097/ACM.0b013e318299fb5d.
- Cook DA, Holmboe ES, Sorensen KJ, Berger RA, Wilkinson JM. Getting maintenance of certification to work: a grounded theory study of physicians’ perceptions. JAMA Intern Med. 2015;175(1):35-42.
https://doi.org/10.1001/jamainternmed.2014.5437.
- Coutinho AJ, Cochrane A, Stelter K, Phillips RL Jr, Peterson LE. Comparison of Intended Scope of Practice for Family Medicine Residents With Reported Scope of Practice Among Practicing Family Physicians. JAMA. 2015;314(22):2364-2372.
https://doi.org/10.1001/jama.2015.13734.
- Pacheco M, Weiss D, Vaillant K, et al. The impact on rural New Mexico of a family medicine residency. Acad Med. 2005;80(8):739-744.
https://doi.org/10.1097/00001888-200508000-00007.
- Chen F, Fordyce M, Andes S, Hart LG. Which medical schools produce rural physicians? A 15-year update. Acad Med. 2010;85(4):594-598.
https://doi.org/10.1097/ACM.0b013e3181d280e9.
- Quinn KJ, Kane KY, Stevermer JJ, et al. Influencing residency choice and practice location through a longitudinal rural pipeline program. Acad Med. 2011;86(11):1397-1406.
https://doi.org/10.1097/ACM.0b013e318230653f.
- Shapiro J, Longenecker R. Country doctors in literature: helping medical students understand what rural practice is all about. Acad Med. 2005;80(8):724-727.
https://doi.org/10.1097/00001888-200508000-00003.
- Pretorius RW, Milling DA, McGuigan D. Influence of a rural background on a medical student’s decision to specialize in family medicine. Rural Remote Health. 2008;8(3):928.
- Rabinowitz HK, Diamond JJ, Markham FW, Santana AJ. The relationship between matriculating medical students’ planned specialties and eventual rural practice outcomes. Acad Med. 2012;87(8):1086-1090.
https://doi.org/10.1097/ACM.0b013e31825cfa54.
- Birks M, Mills J. Ground Theory: A Practical Guide. Thousand Oaks, CA: Sage; 2011.
- US Census Bureau. 2010 Census Urban and Rural Classification and Urban Area Criteria. https://www.census.gov/geo/reference/ua/urban-rural-2010.html. Published September 1, 2012. Accessed November 10, 2017.
- American Academy of Family Physicians. Medical School and Residency. http://www.aafp.org/medical-school-residency.html. Published August 6, 2015. Accessed November 10, 2017.
- NVivo Qualitative Data Analysis Software. Version 10, 2012. Melbourne, Australia: QSR International Pty Ltd.



There are no comments for this article.