Background and Objectives: High rates of unintended pregnancy and poor pregnancy outcomes can be ameliorated by improved access to contraceptive and preconception care. Little data exists regarding application of routine pregnancy intention (PI) screening to reduce unintended pregnancy and optimize preconception health in family medicine residency education. This quality improvement (QI) project evaluated the rate at which family medicine residents and providers (attending physicians and nurse practitioners) addressed women’s unmet reproductive health needs identified through PI screening.
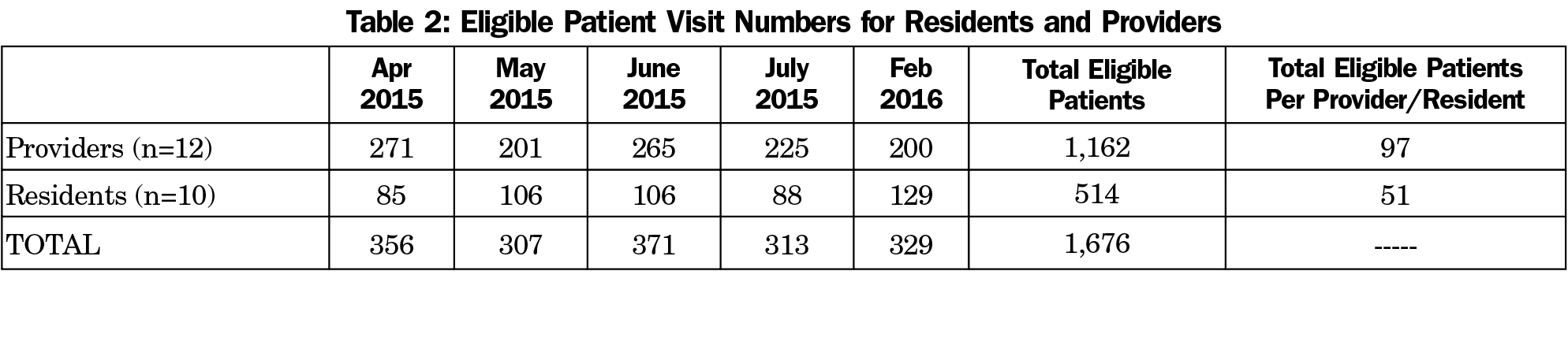
Methods: In April 2015 routine PI screening was implemented at a teaching health center. From April through July chart review was performed of patient encounters for eligible women age 12 to 45 to assess the rate of addressing unmet reproductive health needs, including contraception and/or preconception care, based on provider documentation. Individual resident and provider performance feedback was given monthly. Follow-up chart review was performed in February 2016 to evaluate postintervention performance.
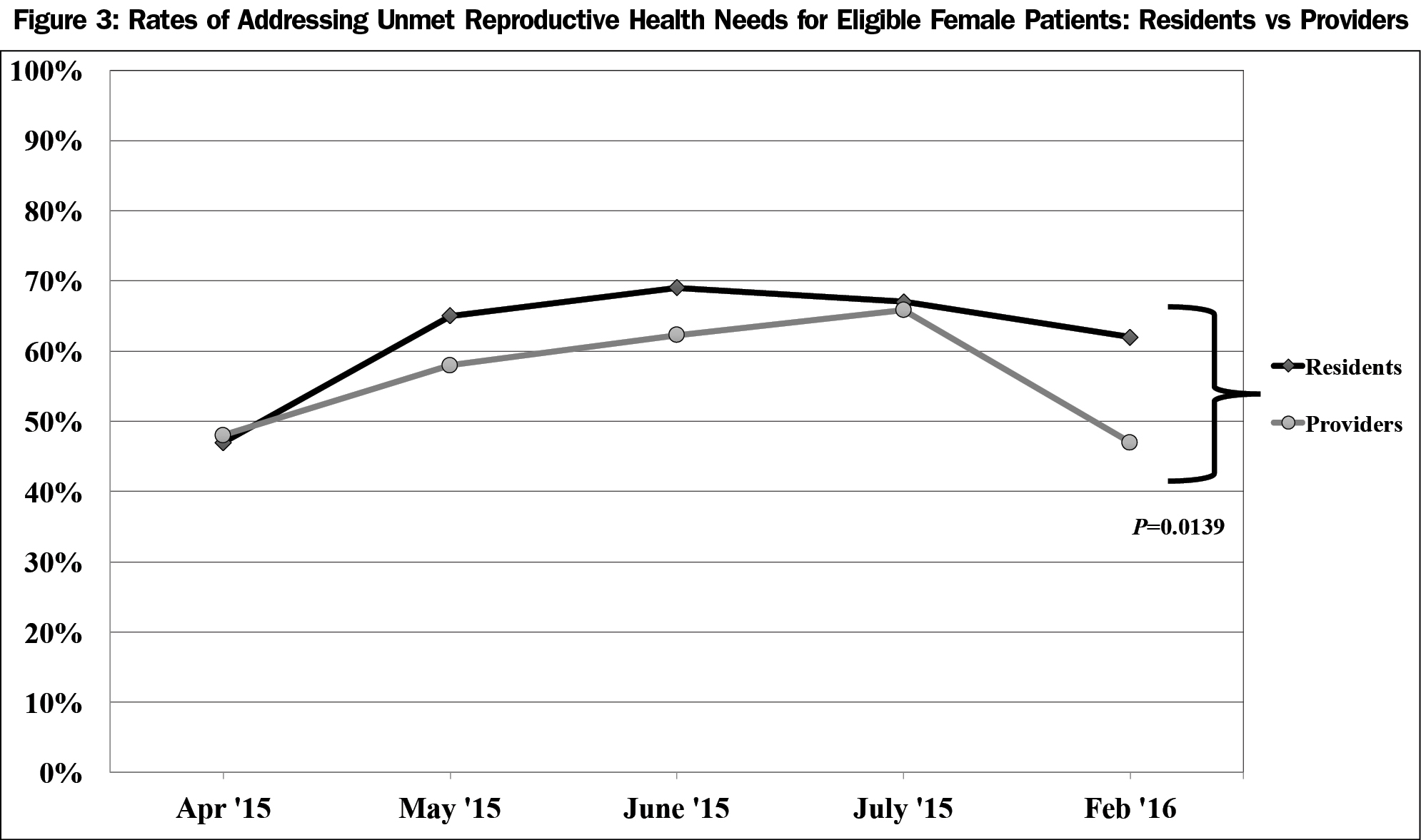
Results: Residents and providers had 1,676 eligible patient visits, and respectively increased their rates of addressing unmet reproductive health care needs from 47% to 48% in April to 66% to 67% in July 2015. Residents had a sustained increased rate of 62% in February 2016 (P=0.0139), while providers did not.
Conclusions: Resident and provider rates of addressing women’s unmet reproductive health needs increased with a simple QI intervention. Residents, but not providers, sustained these rates at 6-month follow-up. Routine PI screening combined with performance evaluation is a promising approach to promote preventive reproductive health education in family medicine residency teaching clinics, but requires further study of long-term outcomes.
Women in the United States have high rates of unintended pregnancy, low contraception utilization, and poor preconception care,1-4 though reliable access to contraceptive and preconception services reduces unintentional pregnancy and improves perinatal outcomes.5-6 Primary care providers are ideally suited to provide these services, yet offer them infrequently. One study found that only 14% of ambulatory care visits with reproductive-aged women included reproductive health services.7
The American Academy of Family Physicians’ curriculum guidelines for residencies includes recommendations for comprehensive training in preconception and contraceptive care.8 A 2011 survey of 245 family medicine residencies reported the majority offered training for most available contraceptive methods.9 Despite this, there is a demonstrated gap between training and desire to provide contraceptive services with adherence to evidence-based practice guidelines.10,11 Minimal data exists evaluating the quality and frequency of reproductive health care provided by family medicine residents (FMR).
Pregnancy intention (PI) screening is one approach to identify women’s unmet reproductive health needs. Women of reproductive age are routinely asked, “Do you want to become pregnant in the next 12 months?” Depending on the response, health care providers offer preconception and/or contraception counseling.12,13 We reported successful implementation of routine PI screening by medical assistants in a family medicine residency teaching clinic.14 In this paper we describe the second part of this quality improvement (QI) project, which aimed to increase rates at which FMRs and providers (attending physicians and nurse practitioners) addressed and documented unmet reproductive health needs revealed by PI screening.
The project setting is a teaching health center in Denver, Colorado. Title X funding makes available low-cost contraceptive services and a family planning health educator.
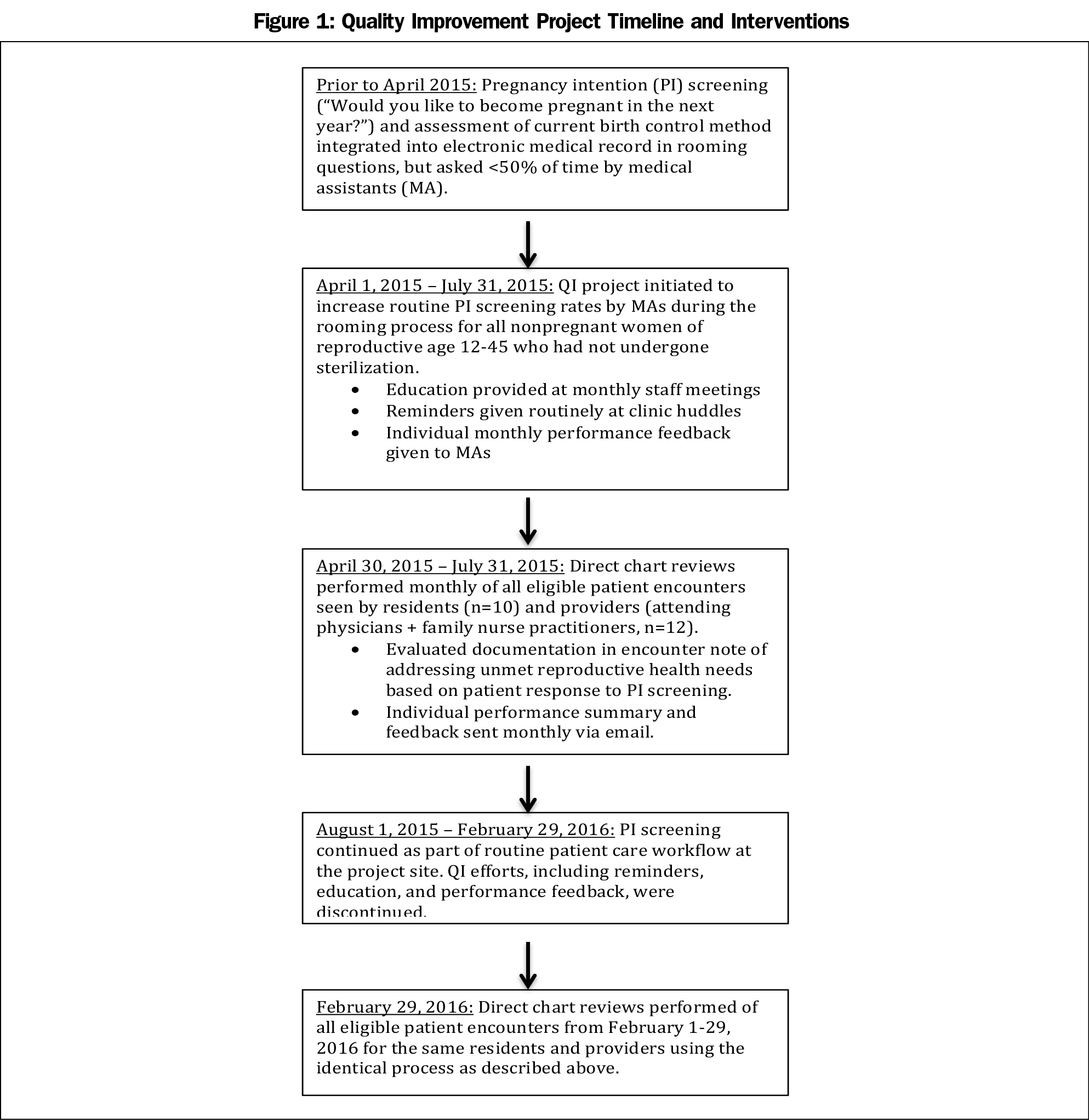
From April 1, 2015 to July 31, 2015, we launched a QI project to implement routine PI screening. Eligible patients included premenopausal, nonpregnant women age 12 to 45 who were not sterilized. Those who had a sterilized male partner, or did not desire pregnancy and had a long-acting reversible contraceptive method were excluded. Prior to project onset, PI screening had been integrated into the electronic medical record (EMR), but medical assistants screened patients inconsistently during rooming.14 For this project, charts of all eligible patient encounters were reviewed monthly from April through July 2015 and February 2016 to assess whether FMRs and providers had documented addressing unmet reproductive health needs. Monthly individual performance feedback was provided through email. The QI timeline and interventions are detailed in Figure 1. Unmet reproductive health needs were defined as having (1) unsure pregnancy desires without use of birth control or prenatal vitamins; (2) no desire for pregnancy and not using an effective form of birth control (eg, combined hormonal contraception, injection, implant, or IUD); or (3) a desire for pregnancy with an uncontrolled chronic illness (eg, hypertension), teratogenic medication use, or lack of prenatal vitamin use (Figure 2).
Three reviewers manually extracted data from the EMR. We determined that FMRs and providers addressed the needs based on the algorithm in Figure 2. We calculated performance rates by the number of visits with eligible women with a documented plan addressing needs divided by the total number of visits with eligible women per month. The April 2015 performance rate was assumed to be equivalent to the baseline rate prior to project initiation. Differences in outcomes were analyzed by provider type (resident vs provider). Data was based on patient visits, deidentified of any protected health information, and pooled anonymously. P values for statistical significance were calculated with a two-proportion z-test.
The Colorado Multiple Institutional Review Boards through University of Colorado-Denver determined this project was not human subjects research.
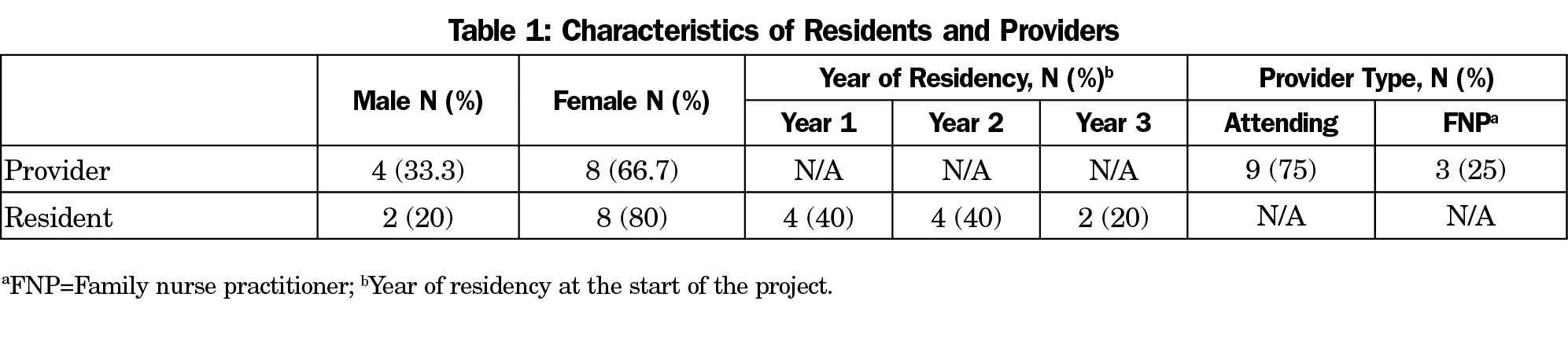
Twelve providers and 10 FMRs were included in the project (Table 1). Two third-year FMRs stayed for fourth-year (nonreproductive health) fellowships after July 2015 and were included in the resident analysis. A total of 1,676 visits with eligible female patients took place during the project (Table 2).
For FMRs, rates of addressing unmet reproductive health needs, as documented in the chart review, rose from a baseline of 47% in April to 67% at the end of the project in July (P=0.0025). Rates dropped to 62% at 6-month follow-up, which was a statistically significant increase from baseline (P=0.0307). Providers’ rates increased from 48% to 66% from April to July (P<0.0001), but these were not sustained at 6 months. Residents had a significantly increased sustained rate at 6 months compared to providers (62% vs 47%; P=0.0139; Figure 3).
Our findings suggest a brief QI intervention to evaluate FMRs and providers regarding documenting contraception and preconception counseling for women with unmet reproductive needs identified through routine PI screening can result in significantly improved monthly performance rates. A modest increase was sustained at 6-month follow-up for FMRs, but not for providers.
Chart review of all eligible patients seen by FMRs allowed for direct, routine application of reproductive care guidelines for women in continuity patient panels as a teaching tool. Our findings may indicate that QI measures to improve performance during residency—an impressionable learning period—are more likely to sustain longer-term practice changes. However, providers’ lack of sustained improvement could be related to the nature of the intervention. A Cochrane review of the “audit and feedback” method of physician performance improvement found enhanced effectiveness with low-performing individuals, ongoing verbal and written feedback from supervisors or colleagues, and clear targets/action plans.15 Further study of verbal feedback in combination with defined performance targets could result in improved rates.
We interpret these findings with caution given the small numbers and brief follow-up period. Higher performance rates could reflect increased documentation rather than actual performance improvement. Additional limitations include lack of reviewer blinding, unknown impacts on patient outcomes, and lack of a control group to assess whether improved performance was secondary to feedback, or clinic reminders.
In conclusion, implementation of routine PI screening with regular performance evaluation in FM teaching clinics is a promising approach to reduce women’s unmet reproductive health needs, and train family physicians that provide holistic, patient-centered women’s health care. However, the long-term outcomes of this approach require further study.
Acknowledgments
This project was funded in part by a grant from the Centers for Disease Control entitled, “Utilizing Health Information Technology and Clinical Decision Support to Improve Reproductive Health Services.” We are grateful to the staff at the project site for their patience and participation in the project. We thank Jennifer Feng for help with data collection, and Brandy Mitchell, the Colorado Community Health Network, and the National Association of Community Health Centers for ancillary support.
Presentations: A poster presentation based on this manuscript was presented at the Society of Teachers of Family Medicine Annual Spring Conference from May 5-9, 2017 in San Diego, CA.
References
- Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478-485.
https://doi.org/10.1016/j.contraception.2011.07.013.
- Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38(2):90-96.
https://doi.org/10.1363/3809006.
- Gipson JD, Koenig MA, Hindin MJ. The effects of unintended pregnancy on infant, child, and parental health: a review of the literature. Stud Fam Plann. 2008;39(1):18-38.
https://doi.org/10.1111/j.1728-4465.2008.00148.x.
- D’Angelo D, Williams L, Morrow B, et al; Centers for Disease Control and Prevention (CDC). Preconception and interconception health status of women who recently gave birth to a live-born infant--Pregnancy Risk Assessment Monitoring System (PRAMS), United States, 26 reporting areas, 2004. MMWR Surveill Summ. 2007;56(10):1-35.
- Atrash HK, Johnson K, Adams M, Cordero JF, Howse J. Preconception care for improving perinatal outcomes: the time to act. Matern Child Health J. 2006;10(5)(suppl):S3-S11.
https://doi.org/10.1007/s10995-006-0100-4.
- Institute of Medicine. Clinical preventive services for women: closing the gaps. Washington, DC: The National Academies Press; 2011. www.nap.edu/read/13181/chapter/1. Accessed February 27, 2017.
- Bello JK, Rao G, Stulberg DB. Trends in contraceptive and preconception care in United States ambulatory practices. Fam Med. 2015;47(4):264-271.
- American Academy of Family Physicians. Women’s Health and Gynecologic Care. AAFP Reprint No. 282. http://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint282_Women.pdf. Accessed February 2, 2017.
- Herbitter C, Greenberg M, Fletcher J, Query C, Dalby J, Gold M. Family planning training in US family medicine residencies. Fam Med. 2011;43(8):574-581.
- Schubert FD, Herbitter C, Fletcher J, Gold M. IUD knowledge and experience among family medicine residents. Fam Med. 2015;47(6):474-477.
- Harper CC, Henderson JT, Raine TR, et al. Evidence-based IUD practice: family physicians and obstetrician-gynecologists. Fam Med. 2012;44(9):637-645.
- Bellanca HK, Hunter MS. One key question: preventive reproductive health is part of high quality primary care. Contraception. 2013;88(1):3-6.
https://doi.org/10.1016/j.contraception.2013.05.003.
- Allen D, Hunter MS, Wood S, Beeson T. One key question: first things first in reproductive health. Matern Child Health J. 2017;21(3):387-392.
https://doi.org/10.1007/s10995-017-2283-2.
- Kvach E, Lose J, Marcus H, Loomis L. Routine screening for pregnancy intention to address unmet reproductive health needs in two urban federally qualified health centers. J Health Care Poor Underserved. 2017;28(4):1477-1486.
https://doi.org/10.1353/hpu.2017.0128.
- Jamtvedt G, Young JM, Kristoffersen DT, O’Brien MA, Oxman AD. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2006;2(2):CD000259.