Background and Objectives: Medical scribes are an increasingly popular strategy for reducing clerical burden, but little is known about their effect on medical student education. We aimed to evaluate the impact of scribes on medical students’ self-reported learning experience.
Methods: We conducted a mixed-methods pilot study. Participants were medical students (third and fourth years) on a family medicine clerkship who worked with an attending physician who practiced with a scribe. Students did not work directly with scribes. Scribes charted for attending physicians during encounters that did not involve a student. Outcomes were three 7-point Likert scale questions about teaching quality and an open-ended written reflection. Qualitative data was analyzed using a constant comparative method and grounded theory approach.
Results: A total of 16 medical students returned at least one questionnaire, yielding 28 completed surveys. Students reported high satisfaction with their learning experience and time spent face-to-face with their attending, and found scribes nondisruptive to their learning. Major themes of the open-ended reflections included more time for teaching and feedback, physicians who were less stressed and more attentive, appreciation for a culture of teamwork, and scribes serving as an electronic health records (EHR) resource.
Conclusions: To our knowledge, this is the first study evaluating the effect of scribes on medical student education from the students’ perspective. Our findings suggest that scribes may allow for greater teaching focus, contribute to a teamwork culture, and serve as an EHR resource. Scribes appear to benefit medical students’ learning experience. Larger and more rigorous studies are needed.
Primary care physicians experience some of the highest rates of burnout, a growing problem now affecting over half of US physicians.1 The causes of burnout are complex, but a key contributor is increasing clerical burden brought on by electronic health record (EHR) systems.2 Physicians now spend nearly twice as much time on EHR and desk work as they do on face-to-face patient care,3 and evidence suggests that EHR use detracts substantially from professional satisfaction.4
One increasingly popular approach to reducing clerical burden has been the adoption of scribes who assist with EHR documentation under a provider’s supervision.5 The evidence on scribes is encouraging—two systematic reviews found that scribes may improve productivity, efficiency, revenue, and patient and physician satisfaction.6,7 Recently, a randomized controlled trial of scribes found improvements in charting efficiency, overall physician satisfaction, and satisfaction with chart quality and accuracy.8
Scribes could be especially valuable for academic physicians, whose teaching duties present an additional time burden on top of charting. While teaching students is enriching and enjoyable to many academic physicians, it can also result in higher stress and longer office days, cutting into both patient care time and personal time. In turn, time pressure can negatively impact the quality of teaching, and EHR tasks can distract from giving feedback. By assisting with time-consuming documentation, scribes could plausibly improve the experience for both students and physicians.
Despite their potential value in academic settings, little is known about the impact of scribes on medical students. A study in the emergency department showed that, when paired with scribes, faculty reported spending more time teaching and giving feedback to students9; however, there have been no studies from medical students’ perspective. The objective of this pilot study was to explore the effects of scribes on medical students’ self-reported learning experience.
Design
The study was conducted from July 1, 2015 to May 31, 2016 at a single family medicine clinic associated with an academic medical center in California. Participants included all medical students (third and fourth years) on the family medicine clerkship who worked with an attending physician who practiced with a scribe. Scribes were college graduates who completed an 80-hour training administered by a commercial company (Elite Medical Scribes, Minnesota). All students rotating at the clinic during the study period were invited to participate; participation was entirely voluntary and anonymous. Students were instructed to do an initial assessment of the patient (ie history and physical), present their findings to the attending physician, and wrap up the visit with their preceptor and patient in the exam room. Students did not work directly with scribes. Scribes charted only for attending physicians during encounters that did not involve a student.
Survey
Medical students were asked to complete a questionnaire at the end of each 4-hour clinic session if their attending physician had a scribe. The questionnaire had three 7-point Likert scale questions about the quality of teaching they received, as well as an open-ended written reflection about their overall learning experience. No identifying information about the student or attending physician was collected.
Data
To analyze the free response data, a codebook was developed using a constant comparative method and grounded theory approach. One author (XW) identified the recurring themes using a data-driven strategy. The codebook was iteratively refined until there was unanimous agreement on the final categories. The content units for data analysis were words and phrases. Two authors (SL, XW) independently reviewed each unit and coded it according to the codebook. Interrater agreement was 100%. This work was granted a formal exemption by the Institutional Review Board of Stanford University School of Medicine.
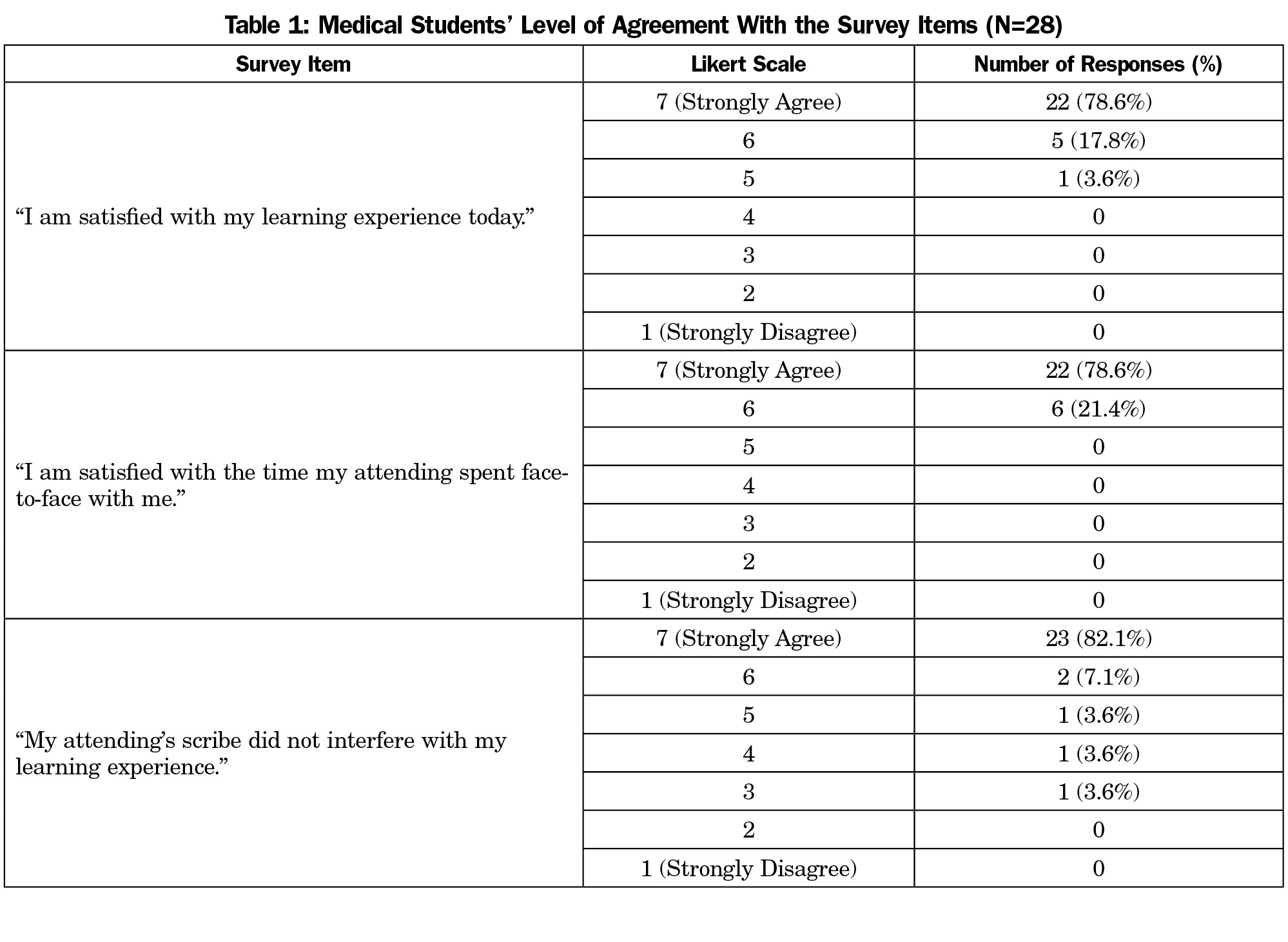
A total of 16 medical students returned at least one questionnaire, yielding 28 completed surveys. Overall, participants were highly satisfied with their learning experience: 27/28 (96.4%) surveys indicated strong agreement (6 or 7 on a 7-point Likert scale) for “I am satisfied with my learning experience today”; 28/28 (100%) surveys indicated strong agreement for “I am satisfied with the time my attending spent face-to-face with me”; and 25/28 (89.3%) reported strong agreement for “My attending’s scribe did not interfere with my learning experience” (Table 1).
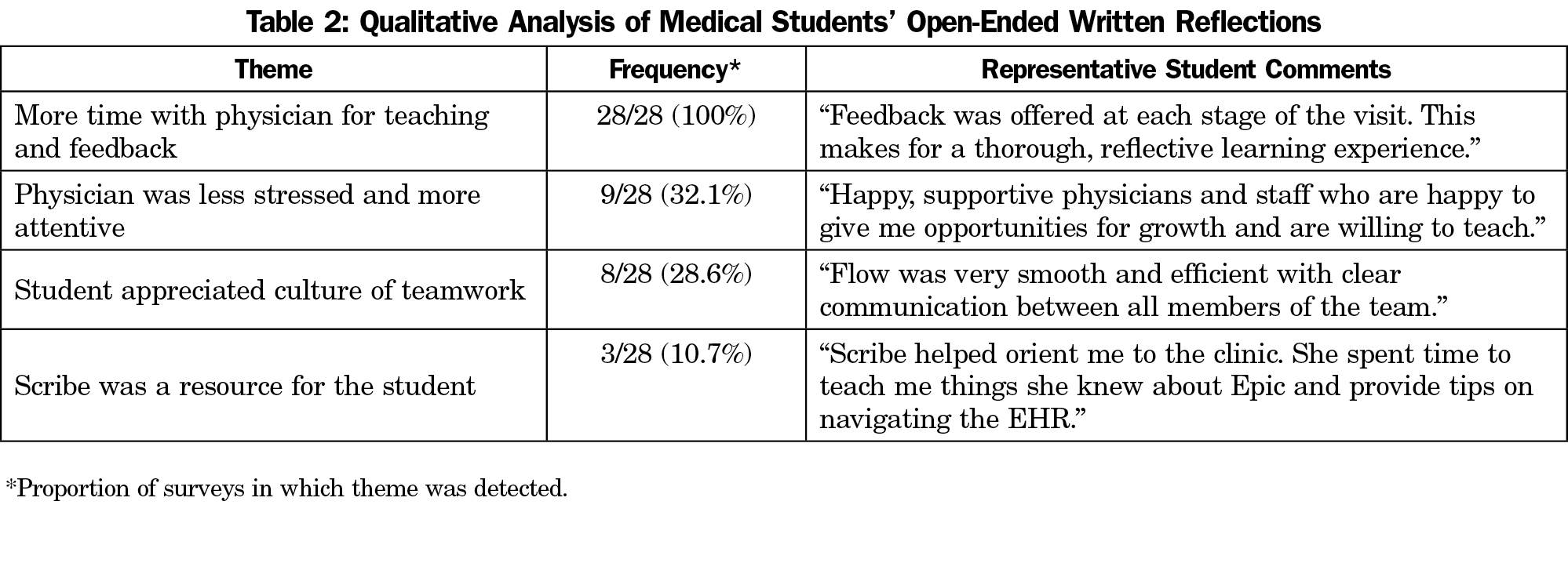
Four distinct themes emerged from the qualitative analysis. The most frequently recurring theme was “more time with physician for teaching and feedback,” which was detected in 28/28 (100%) of surveys. The remaining themes were “physician was less stressed and more attentive” (9/28 or 32.1% of surveys), “student appreciated culture of teamwork” (8/28 or 28.6%), and “scribe was a resource for the student” (3/28 or 10.7%). Representative student comments are shown (Table 2).
This small pilot study suggests that scribes may have a positive impact on medical student education, with a primary benefit being that scribes allow for greater teaching focus. Students unanimously expressed that scribes allowed physicians to dedicate more time to teaching and feedback, and to a lesser extent, they described physicians with scribes as being more relaxed and attentive. This finding is consistent with a study suggesting that scribes increase faculty perception of time available for teaching and feedback.9 Our study corroborates this finding by adding the perspective of medical students, and is the first to do so in the family medicine setting.
Scribes had other auxiliary effects; medical students appreciated their contribution to a culture of teamwork, which has been shown to decrease burnout.10 Also, scribes served as an EHR resource for medical students, who often struggle with changing environments during clinical rotations, in part due to inadequate EHR and documentation training.11,12
Limitations
Our study is limited by a small sample size and lack of an appropriate control group. Since participation was voluntary, there may be selection bias. The Likert scale questions lacked specificity and should be refined in future studies based on findings from our qualitative analysis and others. Our rudimentary results would be strengthened by future work with more participants in well-designed prospective cohort studies.
In this pilot study, medical students reported several potential benefits of scribes on their learning experience. Larger and more rigorous studies are needed.
Acknowledgments
Part of this study was presented as a poster at the Society of Teachers of Family Medicine (STFM) Annual Spring Conference, May 5-9, 2017 in San Diego, CA.
References
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613.
https://doi.org/10.1016/j.mayocp.2015.08.023.
- Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91(7):836-848.
https://doi.org/10.1016/j.mayocp.2016.05.007.
- Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165(11):753-760.
https://doi.org/10.7326/M16-0961.
- Friedberg MW, Chen PG, Van Busum KR, et al. Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy. Santa Monica, CA: Rand Corp; 2013.
- Gellert GA, Ramirez R, Webster SL. The rise of the medical scribe industry: implications for the advancement of electronic health records. JAMA. 2015;313(13):1315-1316.
https://doi.org/10.1001/jama.2014.17128.
- Shultz CG, Holmstrom HL. The use of medical scribes in health care settings: a systematic review and future directions. J Am Board Fam Med. 2015;28(3):371-381.
https://doi.org/10.3122/jabfm.2015.03.140224.
- Heaton HA, Castaneda-Guarderas A, Trotter ER, Erwin PJ, Bellolio MF. Effect of scribes on patient throughput, revenue, and patient and provider satisfaction: a systematic review and meta-analysis. Am J Emerg Med. 2016;34(10):2018-2028.
https://doi.org/10.1016/j.ajem.2016.07.056.
- Gidwani R, Nguyen C, Kofoed A, et al. Impact of scribes on physician satisfaction, patient satisfaction, and charting efficiency: a randomized controlled trial. Ann Fam Med. 2017;15(5):427-433.
https://doi.org/10.1370/afm.2122.
- Hess JJ, Wallenstein J, Ackerman JD, et al. Scribe impacts on provider experience, operations, and teaching in an academic emergency medicine practice. West J Emerg Med. 2015;16(5):602-610.
https://doi.org/10.5811/westjem.2015.6.25432.
- Willard-Grace R, Hessler D, Rogers E, Dubé K, Bodenheimer T, Grumbach K. Team structure and culture are associated with lower burnout in primary care. J Am Board Fam Med. 2014;27(2):229-238.
https://doi.org/10.3122/jabfm.2014.02.130215.
- O’Brien B, Cooke M, Irby DM. Perceptions and attributions of third-year student struggles in clerkships: do students and clerkship directors agree? Acad Med. 2007;82(10):970-978.
https://doi.org/10.1097/ACM.0b013e31814a4fd5.
- Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: causes, consequences, and proposed solutions. Mayo Clin Proc. 2005;80(12):1613-1622.
https://doi.org/10.4065/80.12.1613.



There are no comments for this article.