Background and Objectives: Nearly one-half (46%) of physicians report at least one symptom of burnout. Family medicine residency program directors may have similar and potentially unique levels of burnout as well as resiliency. The primary aims of this study were to examine burnout and resiliency among family medicine residency directors and characterize associated factors.
Methods: The questions used were part of a larger omnibus survey conducted by the Council of Academic Family Medicine (CAFM) Educational Research Alliance (CERA) in 2016. Program and director-specific characteristics were obtained. Symptoms of burnout were assessed using two single-item measures adapted from the full Maslach Burnout Inventory, and level of resiliency was assessed using the Brief Resilience Scale.
Results: The overall response rate for the survey was 53.7% (245/465). Symptoms of high emotional exhaustion or high depersonalization were reported in 27.3% and 15.8% of program directors, respectively. More than two-thirds of program directors indicated that they associated themselves with characteristics of resiliency. Emotional exhaustion and depersonalization were significantly correlated with never having personal time, an unhealthy work-life balance, and the inability to stop thinking about work. The presence of financial stress was significantly correlated with higher levels of emotional exhaustion and depersonalization. In contrast, the level of resiliency reported was directly correlated with having a moderate to great amount of personal time, healthy work-life balance, and ability to stop thinking about work, and negatively correlated with the presence of financial stress.
Conclusions: Levels of emotional exhaustion, depersonalization, and resiliency are significantly related to personal characteristics of program directors rather than characteristics of their program.
Professional burnout is a syndrome characterized by a triad of emotional exhaustion, feelings of cynicism or depersonalization, and decreased sense of personal accomplishment.1-3 A national survey of all physician types found 46% of physicians reported at least one symptom of burnout.1 Family, internal, and emergency medicine physicians had the highest rates of burnout (>50%). When compared to nonphysician, employed population control groups, physicians worked longer hours and struggled more with work-life balance than their nonphysician counterparts, suggesting that this issue is not simply a societal trend.
Physicians in academia are tasked with patient care, research, education, and administrative duties. As providers of medical training as well as mentors and supervisors, physicians model attitudes and behaviors for students under them, influencing the next generation of physicians. One survey of medical school faculty found 42% of respondents were “seriously considering leaving academic medicine in the next 5 years” and 40% were not satisfied with their career progression.4 In another study, 34% of academic faculty members met burnout criteria and burnout was strongly associated with the amount of time faculty were able to focus on the aspect of their careers they found most meaningful, being a younger physician, the number of hours worked per week, and being a generalist instead of a specialist.5 Those physicians with burnout were found to be at an increased risk of leaving academic medicine.
A nationwide study on internal medicine clerkship directors found more than 60% demonstrated burnout, which was associated with having less than 10 hours per week of protected time for their educational role.2 A study of internal medicine residency directors found about 30% of program directors reported burnout. Distress was more common among young program directors, women, and those who spent more hours working per week.6
In contrast to burnout, resiliency is the “ability of an individual to respond to stress in a healthy, adaptive way such that personal goals are achieved at minimal psychological and physical cost,” which may be an important characteristic for academic physicians in their roles as teachers and mentors as they address the issue of burnout.7 Further study of resiliency in these physicians is particularly needed.8
Family medicine residency program directors may have similar and potentially unique levels of burnout and resiliency compared to other groups of physicians. The primary aims of this study were to examine burnout and resiliency among family medicine residency directors and characterize factors that may influence whether one experiences burnout or resiliency.
The questions were part of a larger omnibus survey conducted by the Council of Academic Family Medicine (CAFM) Educational Research Alliance (CERA). The survey methods and sample demographics have previously been presented.9
The CERA steering committee evaluated questions for consistency with the overall subproject aim, readability, and existing evidence of reliability and validity. Pretesting was done on family medicine educators who were not part of the target population. Questions were modified following pretesting for flow, timing, and readability. The project was approved by the American Academy of Family Physicians Institutional Review Board in December 2015. Data was collected from July to August 2016.
The sampling frame for the survey was all Accreditation Council for Graduate Medical Education (ACGME)-accredited US family medicine residency program directors as identified by the Association of Family Medicine Residency Directors (AFMRD). Email invitations to participate were delivered with the survey utilizing the online program Survey Monkey. Four follow-up emails to encourage nonrespondents to participate were sent after the initial email invitation. There were 495 program directors at the time of the survey. Eleven had previously opted out of CERA surveys. The survey was emailed to 484 individuals. Nine emails could not be delivered, nine individuals opted out of the survey, and one individual replied that she was no longer a program director. The final sample size was therefore 465.
Survey Items
Respondents were asked demographic information about their program including type, approximate size of the community, proportion of current residents in program who are graduates of non-US medical schools, and program director tenure and gender. Program location was reported as within one of the five geographic regions. Respondents provided the number of years of service as program director.
In this study, the survey included 13 questions addressing burnout and resiliency. The Maslach Burnout Inventory (MBI) is considered the reference standard for the assessment of burnout.10 Many evaluations of burnout have focused on high levels of either emotional exhaustion or depersonalization as the foundation of burnout among high-achieving medical professionals.11,12 In this study, symptoms of burnout were assessed using two single-item measures adapted from the full MBI. Emotional exhaustion was assessed by the question “How often do you feel burned out from your work?”, and depersonalization was assessed by the question “How often do you feel you’ve become more callous toward people since you took this job?” Each question was answered on a 7-point Likert scale, with response options ranging from “Never” to “Every day”. Symptoms of high emotional exhaustion or high depersonalization were defined by a frequency of at least weekly on the single-item emotional exhaustion and depersonalization measure, respectively. These single items correlate strongly with the emotional exhaustion and depersonalization domains of burnout as measured by the full MBI.13 The single items have also been shown to perform well as predictive factors relative to the full MBI.13
For the present analysis, predictive associations within each study for the single-item burnout measures versus the full MBI were compared. Because emotional exhaustion is measured on a 0-54 scale on the full MBI and the single emotional exhaustion item score ranges from 0–6 (response options for each question on the MBI are on a 7-point Likert scale ranging from “Never” to “Daily”), each 1-point change on this single-item measure equates to a 9-point change in the emotional exhaustion domain of the full MBI. Similarly, because depersonalization is measured on a 0-30 scale on the full MBI and the single depersonalization item score ranges from 0-6, each 1-point change on this single-item measure equates to a 5-point change in the depersonalization domain of the full MBI. Thus, to obtain model estimates comparable with the full MBI subscale scores, the emotional exhaustion and depersonalization scores on the single-item measures were multiplied by 9 and 5, respectively. This method has been previously described elsewhere.14
The Brief Resilience Scale (BRS) has been found to be a reliable means of assessing resilience as the ability to bounce back or recover from stress and may provide unique and important information about individuals coping with health-related stressors.14 The BRS consists of six items. Items 1, 3, and 5 are positively worded, and items 2, 4, and 6 are negatively worded. The BRS was scored by reverse-coding items 2, 4, and 6, and finding the mean of the six items. The following instructions were used to administer the scale: “Please indicate the extent to which you agree with each of the following statements by using the following scale: 1=strongly disagree, 2=disagree, 3=neutral, 4=agree, 5=strongly agree.”
To attempt to identify additional factors that may predispose to burnout or add to resiliency, several additional items to assess personal characteristics of the program directors were developed and included the following statements: “I have personal time for myself after work (leisure, fitness, health maintenance)”; “I have a healthy balance between work and personal commitments”; “I am able to stop thinking about work once I go home for the day”; and “I feel overwhelmed by my personal responsibilities.” These items were scored from 0–5 (response options for each question were on Likert scale ranging from “Never” to “Usually”). Finally, the survey included questions regarding number of children, number of vacation days taken during the past year, and the presence of financial stress (for financial stress, the response options were “None,” “Some,” “Considerable,” or “Severe”).
As noted in previous studies, scores are often categorized into varying levels based upon published normative scoring. As such, a comparative analysis for categorical burnout domains comparing emotional exhaustion and depersonalization was conducted. Similar to the method described by West14 that dichotomized the responses, high levels of emotional exhaustion and depersonalization on the single items were defined as occurring at least weekly, consistent with previously reported thresholds.13 A similar categorization was used for the personal characteristics with “moderate” and “great deal” serving as one level (“occasionally” by our definition would not occur at least weekly). The responses to the question regarding financial stress were dichotomized into “none/some” or “considerable/severe”.
Analysis
Descriptive statistics were performed on characteristics provided, such as program location, program size, initial year of program establishment, program directors’ years of experience, type of residency program (community vs university-based), and percentage of residents trained at international medical schools. Two-sample Wilcoxon rank sum test was used to test whether two groups share the same distribution of a burnout or resilience response. Statistical significance was defined as P<0.05 level of confidence. The data was stored in a secure file and all statistical analyses were performed with the statistical computer package R (version 3.3.0).
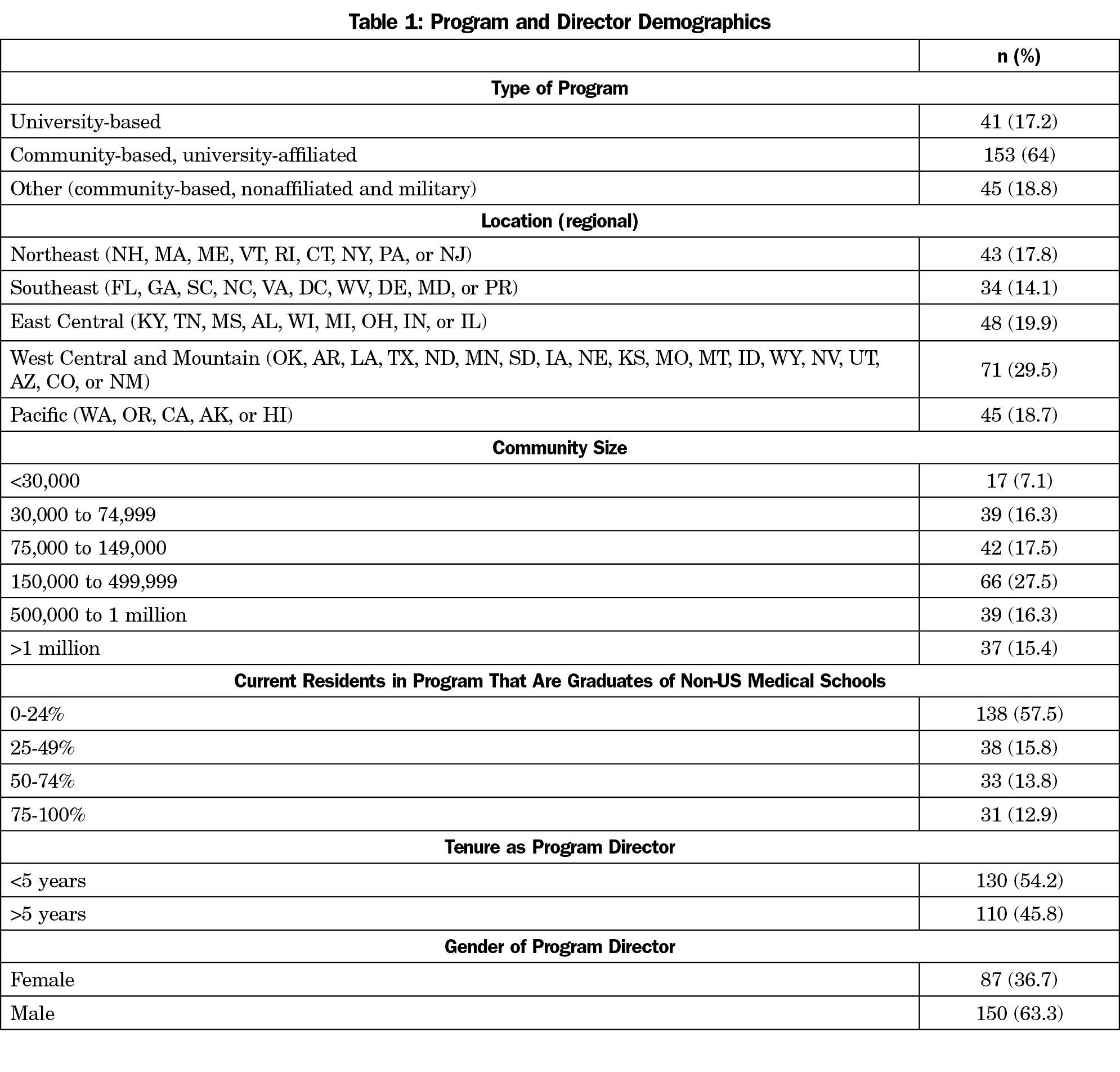
The overall response rate for the survey was 53.7% (245/465). In summary, the responding directors mostly represented community-based, university-affiliated programs located in communities with a population greater than 150,000, had less than 25% of the current residents as graduates of non-US medical schools, served as program director for less than 5 years, and were male (Table 1).
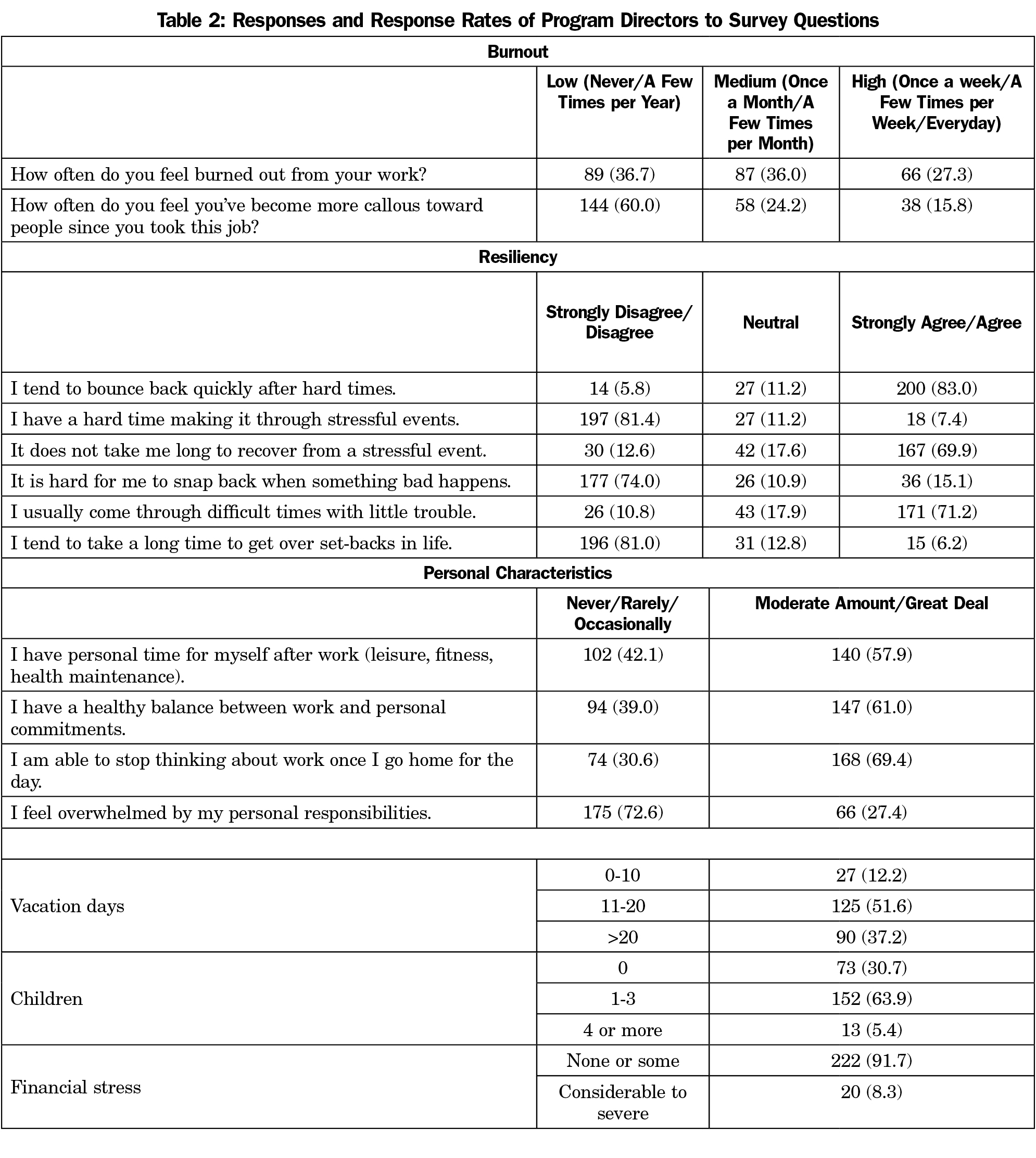
Symptoms of high emotional exhaustion or high depersonalization were reported in 27.3% and 15.8% of program directors, respectively (Table 2). More than two-thirds of program directors indicated that they associated themselves with characteristics of resiliency. Most program directors indicated they had a moderate amount or a great deal of personal time (58%), healthy balance between work and personal commitments (61%), and ability to stop thinking of work once at home for the day (69%). Over one-quarter of program directors (27%) felt they were moderately to greatly overwhelmed by personal responsibilities. Finally, most program directors had 11 to 20 days of vacation during the past year (52%), one to three children (64%), and some to severe financial stress (52%).
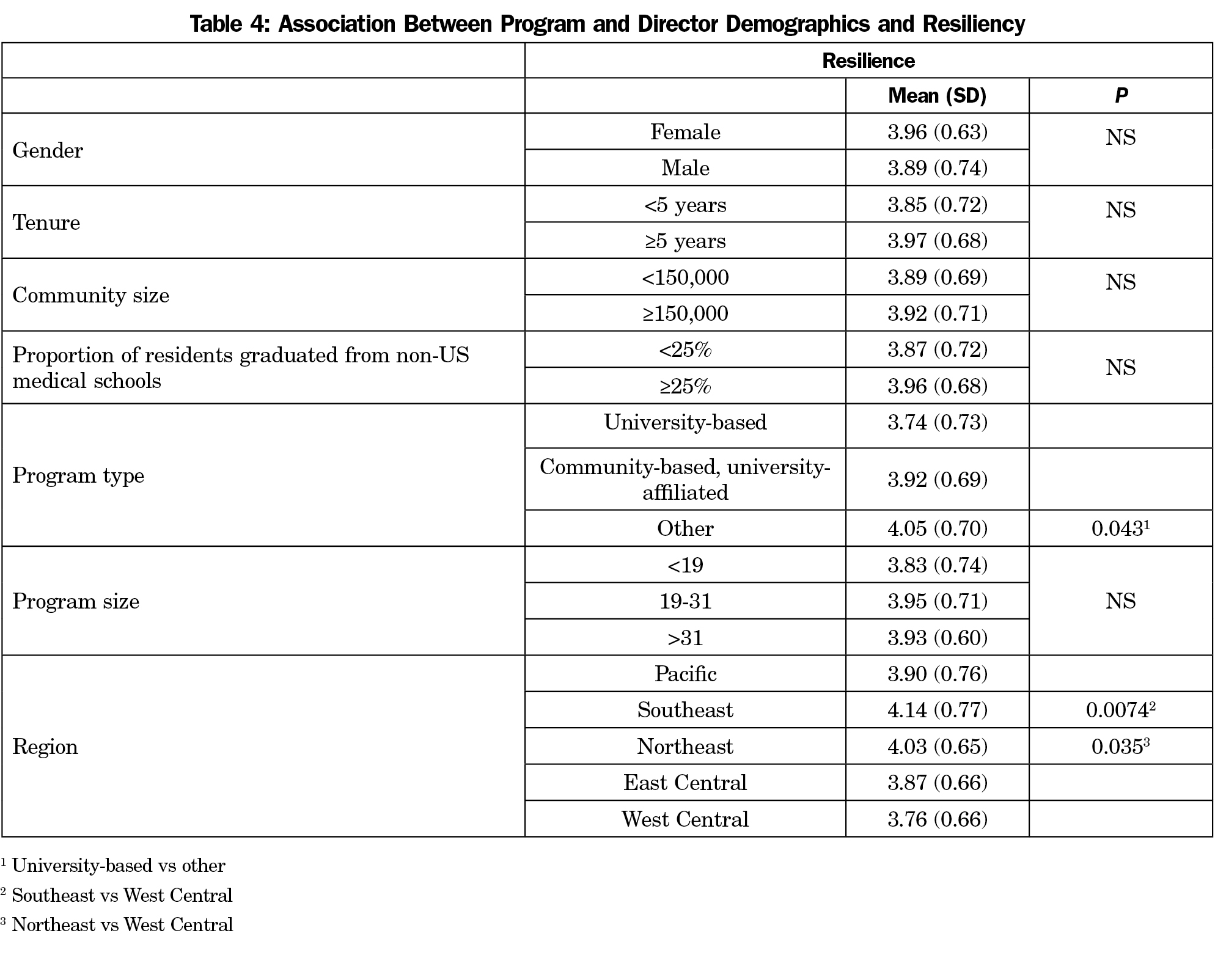
Few significant associations with program demographics and characteristics of burnout or resiliency were found (Tables 3 and 4). The significant associations were noted in the responses from directors based upon certain program type and specific geographic region of the program.
Higher levels of emotional exhaustion and depersonalization were significantly correlated with program directors who reported occasionally to never having personal time (27.58+15.31 vs 18.71+14.59, P<0.02; 9.75+8.55 vs 7.25+7.40, P=0.03), a healthy work-life balance (27.90+15.48 vs 17.19+13.50, P<0.01; 10.05+8.65 vs 6.50+6.85, P<0.01), and ability to stop thinking about work (27.09+15.66 vs 16.56+12.96, P<0.02; 9.95+8.45 vs 5.80+6.65, P<0.01). Similarly, program directors who reported moderate to great deal of being overwhelmed by personal responsibilities had higher levels of emotional exhaustion and depersonalization (34.38+14.49 vs 19.89+14.22; P<0.01; 13.20+8.85 vs 7.05+7.25, P<0.01). The presence of considerable or severe financial stress was also significantly correlated with higher levels of emotional exhaustion and depersonalization (32.85+15.84 vs 23.04+15.39, P<0.01; 13.50+10.00 vs 8.25+7.84; P=0.02). The number of children and the number of vacation days taken during the past year were not significantly correlated with the level of emotional exhaustion or depersonalization.
In contrast, the level of resiliency reported was directly correlated with having a moderate to great amount of personal time (4.10+0.67 vs 3.77+0.69, P<0.01), healthy work-life balance (4.12+0.67 vs 3.78+0.69, P<0.01), and ability to stop thinking about work (4.24+0.63 vs 3.77+0.68, P<0.01), and indirectly correlated with the feeling of being overwhelmed by personal responsibilities (4.03+0.66 vs 3.58+0.69, P<0.01) and the presence of considerable or severe financial stress (3.95+0.69 vs 3.50+0.74, P=0.01). As with symptoms of burnout, resiliency was not correlated with the number of children or number of vacation days taken in the past year.
The rate of the characteristics of burnout among family medicine residency program directors appears to be comparable to or lower than other groups previously studied. In board certified family physicians using the Mini Z burnout survey, the burnout rate was found to be 24.5%, with female sex and age significantly associated with burnout.16 The rate of emotional exhaustion and depersonalization in family medicine residency program directors compares favorably to rates noted among medical students (37.4% and 27.9%, respectively), internal medicine residents (45.8% and 28.9%, respectively), practicing physicians (37.9% and 29.4%, respectively), clerkship directors (46.2% and 41.3%, respectively), and medical school deans (40.4% and 23.6%).2, 17-20
A survey of internal medicine program directors reported similar results, as 27.0% reported emotional exhaustion and 10.4 % reported depersonalization.6 In that study, characteristics of burnout rates were significantly higher among women and directors reporting greater weekly work hours. While depersonalization symptoms affected younger program directors to a greater degree than older program directors, differences in emotional exhaustion and overall burnout did not statistically significantly differ by age. As with the current study, West et al also found that neither emotional exhaustion nor depersonalization had statistically-significant associations with program director tenure. Similar to financial stress, work-home conflicts were common and associated with emotional exhaustion and depersonalization. Also similar to the current study, West et al found that associations with program characteristics such as program size and American Board of Internal Medicine (ABIM) pass rates were not found apart from higher rates of depersonalization among directors of community-based programs.
Overall, few family medicine program and program director demographic characteristics were found to be significantly associated with emotional exhaustion and depersonalization. We did find differences in burnout based upon program director gender or tenure as noted on other studies.6 Similarly, few program and director demographic characteristics were found to be significantly associated with resiliency. Of note, and an area that would require additional study, directors of other program types had lower levels of depersonalization and higher levels of resiliency compared to directors of university-based programs. Based upon these findings, changing general program characteristics or program directors moving to a new program in an attempt to reduce symptoms of burnout and improve attributes of resiliency may not be effective.
In terms of more personal factors, higher levels of personal time, healthy work-life balance, and ability to stop thinking about work were associated with lower levels of emotional exhaustion and depersonalization and higher levels of resiliency. In contrast, the presence of financial stress was significantly related to emotional exhaustion and depersonalization and inversely related to resiliency. Number of children and vacation days taken during the past year were not associated with emotional exhaustion, depersonalization, or resiliency. These findings are similar to a study that noted surgeons placing greater emphasis on finding meaning in work, focusing on what is important in life, maintaining a positive outlook, and embracing a philosophy that stresses work-life balance were less likely to be burned out.19 Based upon these findings, interventions addressing more personal characteristics of residency program directors, especially financial stress, may be more effective in addressing issues associated with burnout and improving attributes of resiliency.
Certain limitations of this study are noted. First, though the questionnaire was distributed to the entire population of program directors, we were not able to obtain a 100% response rate. The effect of nonrespondents upon the results would have been variable and probably would not have altered our findings. In addition, our survey did not include other questions related to burnout present in MBI, though the two questions we did use were consistent with the methods of other studies already cited. Finally, although program directors were asked about specific characteristics associated with burnout and resiliency, some important factors may have been inadvertently omitted from the list.
In conclusion, levels of emotional exhaustion, depersonalization, and resiliency are significantly related to more personal characteristics of family medicine program directors rather than demographic characteristics of the program director or the associated program itself.
References
- Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377-1385. https://doi.org/10.1001/archinternmed.2012.3199.
- Dyrbye LN, Shanafelt TD, Thomas MR, Durning SJ. Brief observation: a national study of burnout among internal medicine clerkship directors. Am J Med. 2009;122(3):310-312.
https://doi.org/10.1016/j.amjmed.2008.11.008.
- Ishak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1(2):236-242.
https://doi.org/10.4300/JGME-D-09-00054.1.
- Lowenstein SR, Fernandez G, Crane LA. Medical school faculty discontent: prevalence and predictors of intent to leave academic careers. BMC Med Educ. 2007;7(1):37.
https://doi.org/10.1186/1472-6920-7-37.
- Shanafelt TD, West CP, Sloan JA, et al. Career fit and burnout among academic faculty. Arch Intern Med. 2009;169(10):990-995.
https://doi.org/10.1001/archinternmed.2009.70.
- West CP, Halvorsen AJ, Swenson SL, McDonald FS. Burnout and distress among internal medicine program directors: results of a national survey. J Gen Intern Med. 2013;28(8):1056-1063.
https://doi.org/10.1007/s11606-013-2349-9.
- Epstein RM, Krasner MS. Physician resilience: what it means, why it matters, and how to promote it. Acad Med. 2013;88(3):301-303.
https://doi.org/10.1097/ACM.0b013e318280cff0.
- Zwack J, Schweitzer J. If every fifth physician is affected by burnout, what about the other four? Resilience strategies of experienced physicians. Acad Med. 2013;88(3):382-389.
https://doi.org/10.1097/ACM.0b013e318281696b.
- Mainous AG III, Seehusen D, Shokar N. CAFM Educational Research Alliance (CERA) 2011 Residency Director survey: background, methods, and respondent characteristics. Fam Med. 2012;44(10):691-693.
- Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996.
- Rafferty JP, Lemkau JP, Purdy RR, Rudisill JR. Validity of the Maslach Burnout Inventory for family practice physicians. J Clin Psychol. 1986;42(3):488-492.
https://doi.org/10.1002/1097-4679(198605)42:33.0.CO;2-S.
- Thomas NK. Resident burnout. JAMA. 2004;292(23):2880-2889.
https://doi.org/10.1001/jama.292.23.2880.
- West CP, Dyrbye LN, Sloan JA, Shanafelt TD. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009;24(12):1318-1321.
https://doi.org/10.1007/s11606-009-1129-z.
- West CP, Dyrbye LN, Satele DV, Sloan JA, Shanafelt TD. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. 2012;27(11):1445-1452. https://doi.org/10.1007/s11606-012-2015-7.
- Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194-200.
https://doi.org/10.1080/10705500802222972.
- Puffer JC, Knight HC, O’Neill TR, et al. Prevalence of burnout in board certified family physicians. J Am Board Fam Med. 2017;30(2):125-126.
https://doi.org/10.3122/jabfm.2017.02.160295.
- Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149(5):334-341.
https://doi.org/10.7326/0003-4819-149-5-200809020-00008.
- West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306(9):952-960.
https://doi.org/10.1001/jama.2011.1247.
- Shanafelt TD, Oreskovich MR, Dyrbye LN, et al. Avoiding burnout: the personal health habits and wellness practices of US surgeons. Ann Surg. 2012;255(4):625-633.
https://doi.org/10.1097/SLA.0b013e31824b2fa0.
- Gabbe SG, Webb LE, Moore DE, Harrell FE Jr, Spickard WA Jr, Powell R Jr. Burnout in medical school deans: an uncommon problem. Acad Med. 2008;83(5):476-482.
https://doi.org/10.1097/ACM.0b013e31816bdb96.



There are no comments for this article.