Background and Objectives: Numerous organizations are calling for the expansion of graduate medical education (GME) positions nationally. Developing new residency programs and expanding existing programs can only happen if financial resources are available to pay for the expenses of training beyond what can be generated in direct clinical income by the residents and faculty in the program. The goal of this study was to evaluate trended data regarding the finances of family medicine residency programs to identify what financial resources are needed to sustain graduate medical education programs.
Methods: A group of family medicine residency programs have shared their financial data since 2002 through a biennial survey of program revenues, expenses, and staffing. Data sets over 12 years were collected and analyzed, and results compared to analyze trends.
Results: Overall expenses increased 70.4% during this period. Centers for Medicare and Medicaid Services (CMS) GME revenue per resident increased by 15.7% for those programs receiving these monies. Overall, total revenue per resident, including clinical revenues, state funding, and any other revenue stream, increased 44.5% from 2006 to 2016. The median cost per resident among these programs, excluding federal GME funds, is currently $179,353; this amount has increased over the 12 years by 93.7%.
Conclusions: For this study group of family medicine programs, data suggests a cost per resident per year, excluding federal and state GME funding streams, of about $180,000. This excess expense compared to revenue must be met by other agencies, whether from CMS, the Health Resources and Services Administration (HRSA), state expenditures or other sources, through stable long-term commitments to these funding mechanisms to ensure program viability for these essential family medicine programs in the future.
Workforce analyses have projected the need for more physicians, particularly primary care physicians, in the coming years.1-3 Addressing this projected shortage of providers will require creating new primary care residency training positions4 and as such, the American Medical Association, Association of American Medical Colleges, and numerous other organizations are calling for the expansion of graduate medical education positions nationally.5,6 New medical schools are developing in many regions, and many existing medical schools are expanding to meet the demand for all specialties in the future. All of these new students will need residency positions in which to train, and a particular need for primary care physicians—whose training is more costly than specialty training because of clinical revenue differences7—as well as for redistribution of physicians from urban to rural locations, is fueling interest in many states to help finance the start-up phase for new residency programs.
Developing new programs and expanding existing residency programs can only happen if two necessary conditions are met. First, resources required for training in the particular specialty must be present in the community (patient population, faculty in that specialty, teachers from other specialties, clinic and hospital facilities with needed capacity), and second, financial revenue streams must be present to pay for the expenses of training beyond what can be generated in direct clinical income by the residents and faculty in the program.
Understanding the sources of revenue and the amount of money potentially available from each source to offset the expenses of residency programs is essential to everyone involved in developing and sustaining these programs. In particular, leadership and boards of local clinics and hospitals need to understand what may be “asked” of them for financial support. State legislatures are starting to provide payment streams to assist state programs and need to know how much money is needed. Nationally, both the Centers for Medicare and Medicaid Services (CMS)—which provides Medicare and Medicaid Graduate Medical Education (GME) funding—and the Health Resources and Services Administration (HRSA)—which provides GME funding for the Teaching Health Center (THC) program—are being examined for their critical roles and amounts of payments for graduate medical education.7,8 Future budget planning and regulatory decisions by these organizations are essential to the ongoing financing of residency programs, but data to guide those decisions are limited.9
Published data examining the expenses and overall costs of residency programs have struggled with how to account for the variability in the sizes and structures of these programs, complicated further by regional variations in practice revenues, wage indices, local cost of living, wealth of community, organizational size and structure, and other variables.3,6,7 In particular, primary care training is difficult to normalize given the differences in program structures between those that are based in community clinics, hospitals, and academic medical centers. A recent article examining the costs of the THC programs provided a cost per resident estimate,8 but this is not an ideal benchmark for other, non-THC programs due to accreditation differences and practice structure and reimbursement differences.
The goal of this paper is to provide trended data that has comprehensively tracked the finances and operations of a network of family medicine residency programs who represent a wide range of program structures, specifically to compare the cost per resident for established Accreditation Council for Graduate Medical Education (ACGME)-accredited core family medicine programs more typically financed by CMS rather than the THC program. Our objectives are to identify trends and questions regarding program financing to elucidate important considerations in the ongoing national discussion about what is needed to support graduate medical education programs, and how this might be accomplished.
This study was considered exempt from IRB review under University of Washington Human Subjects Research guidelines.
The University of Washington Family Medicine Residency Network (“the Network”), currently consists of 30 family medicine residency programs in Washington, Wyoming, Alaska, Montana, and Idaho all of which are affiliated with the University of Washington, but are independently sponsored by their clinics, local hospital systems, universities, or consortia, and thus financially independent of one another except where sponsorship is mutual. Program structure varies significantly; the number of residents per year ranges from 6 to 15 (median: 8), and the number of faculty from 4 to 12 (median: 6).
The Network was established in 1977, with collaborative relationships among all programs in supporting sharing of best practices, data, and resources. As part of this, Network programs have shared their financial data since 2002 through a biennial survey of program revenues, expenses, staffing, and productivity data. Each survey was conducted in a defined time frame, at a similar time of year, and analysis of the data across multiple elements was done using a standardized approach for each biennial data set. Results of prior data analyses have been published.7–9
The current data set was similarly collected and analyzed, and results compared against previous data sets from 2006, 2008, 2010, and 2012. All 18 established core programs reported data sets. Several programs in the Network were excluded from this analysis because their financial models are significantly different from ACGME-accredited established core family medicine programs, including programs that had not yet graduated their first class of residents, osteopathic programs that had not yet been accredited by the ACGME under the Single Accreditation System, and Rural Training Tracks which are all smaller and affiliated with a core program. Median values for all data elements were analyzed rather than mean values, given some significant outliers in individual data elements.
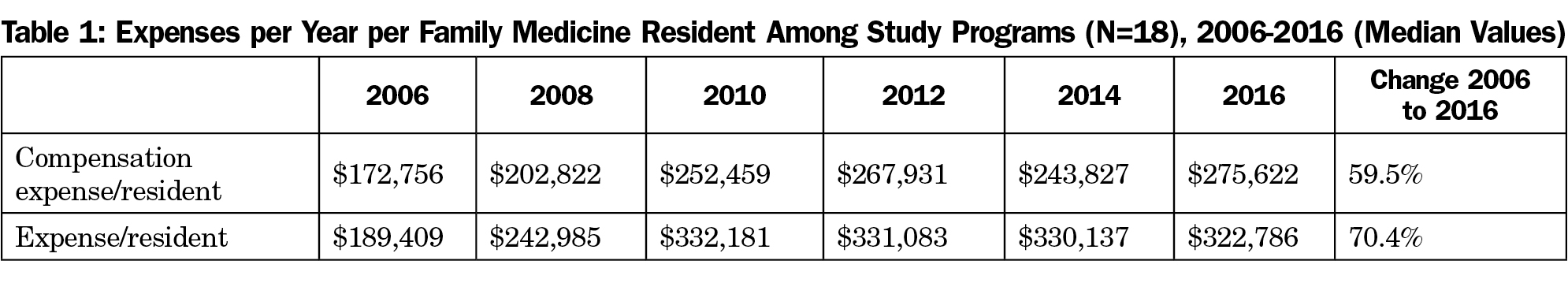
Expenses (Table 1)
Expenses for the residency program were defined as all expenses attributable to the operations of a family medicine program, including the expenses of the family medicine clinic where the core program resident and faculty practices were based.
Compensation expense per resident included the salary and benefits for the resident, and apportioned compensation expenses for faculty teaching and administration and program staff support. For all programs, this expense comprised the majority (median=82.8%) of the overall budget of the residency program, not including the operations of the clinics and hospitals where the residents train. This expense increased 59.5% between 2006 and 2016.
Overall expenses increased 70.4% during this period, reflecting additional increased costs for other infrastructure supports.
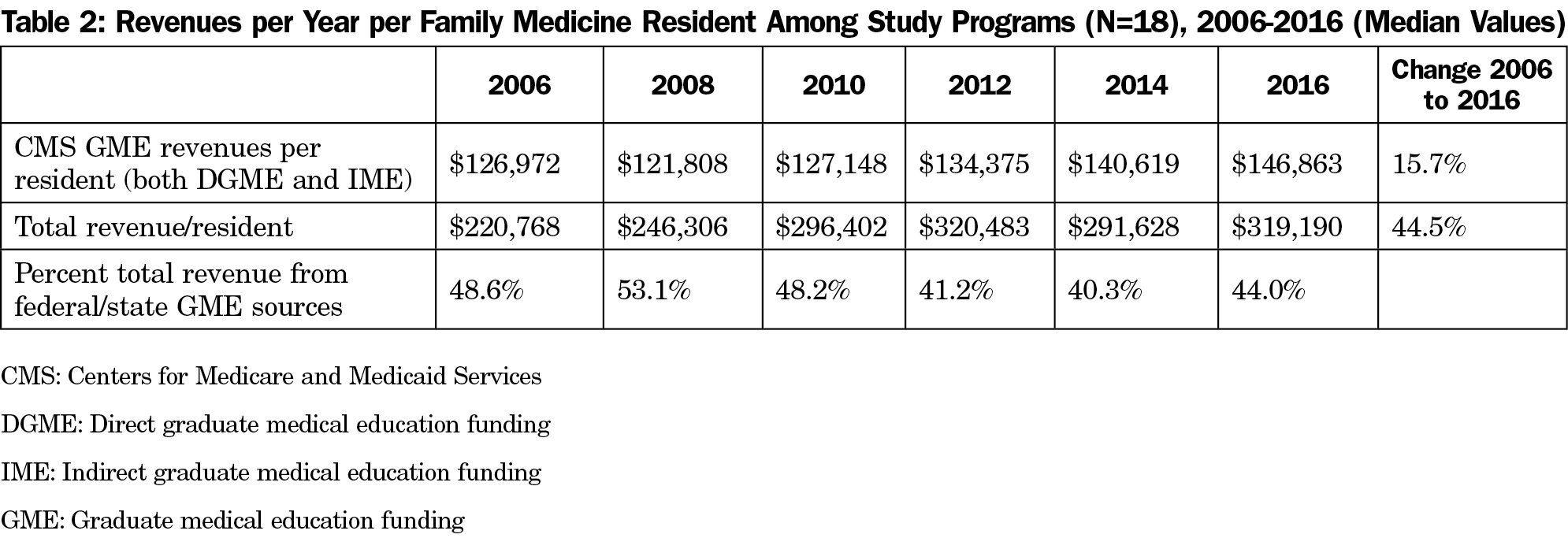
Revenues (Table 2)
CMS Direct Graduate Medical Education (DGME) revenue per resident increased by 15.7% over the period 2006 to 2016 for those programs receiving these monies. Of note, three programs in the Network have historically received minimal or no money from CMS DGME sources since the establishment of caps on the number of residents who could receive DGME funding in 1996.10
Medicaid GME revenues were reported to have been paid to hospitals where residents are training in three of the five states in which the Network programs are based; one state (Wyoming) has never funded Medicaid GME, and one state (Alaska) had recently stopped this funding.11 However, few programs were able to discover what the actual Medicaid GME payment was to their institution (only 5 of 16 programs that should be receiving this reported an amount), and none reported that these payments were directly part of their program’s budget. These revenues were not included in this analysis.
Clinical revenues, which comprise on average 39.3% of total program revenues, continue to be based on fee-for-service volumes for the majority of Network programs. The penetration of managed care remains limited, and reimbursements related to advanced practice models and quality measures was still limited at the time of the most recent survey. The median payer mix for Medicare and Medicaid patients for these programs was 63% of visits, a recent increase from a prior stable value of 57%. Practices in the Network based in federally qualified health centers, compared to those residency practices that were in traditional fee-for-service clinics, received a median reimbursement per clinic visit that was 30.6% higher.
State funding excluding Medicaid GME monies varied widely over these years, not only between states but within an individual state, depending on state budget allocations. Overall state funding contributed a median of 5.1% of total program revenues.
Overall, total revenue per resident, including clinical revenues, state funding, and any other revenue stream, increased 44.5% from 2006 to 2016. The percent of total revenue from federal and state sources decreased slightly from 2006 but remained stable over the most recent years between 40.3% and 44.0%.
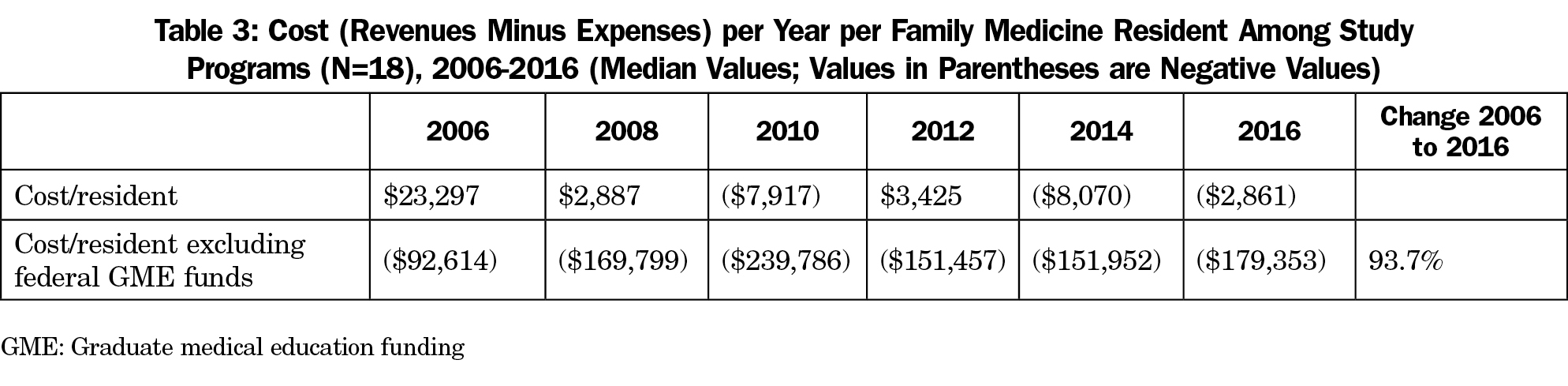
Cost per Resident (Table 3)
The median cost per resident, including both Medicare and Medicaid GME revenues, came close to breakeven throughout these years, but with wide variability both between programs, and within the same program from year to year. Ultimately, programs must come close to breaking even for ongoing support of the programs, as the sponsoring institutions are mandated by the ACGME to assure that programs will have the resources they need to operate and adequately train residents.12
However, the median cost per resident among these programs, excluding federal GME funds, is currently $179,353. This amount has increased over the 12 years by 93.7%, reflecting the increasing cost relative to patient and other non-GME revenues of residency training in primary care and specifically family medicine.
Understanding the financing of residency programs is essential to policy decision-making at all levels: federal, state, and local. Although there is significant variability in individual program expenses and revenues and different program sizes and structures among these programs, the standardized methodology and biennial tracking of the same group of programs over 12 years suggests significant trends that have applicability to broad policy discussions. The current analysis underscores many concepts that are key to understanding why expenses relative to revenues may vary greatly between program structures, and the importance of identifying stable revenue streams, including the critical need for ongoing state and federal funding for training.
The median expense relative to revenues generated locally by the program itself, excluding payments by federal GME funding streams, is $179,353 per resident per year. This is 13.8% higher than the $157,602 recently reported for residencies in the HRSA THC program, and 23.6% higher than the $144,999 reported for existing THC programs that had expanded.4 There are several explanations for this difference. First, most of the THC programs are based in federally qualified ealth centers (FQHC) that get enhanced patient care reimbursements for Medicare and Medicaid patients, whereas most of the residency practices in this study see similar populations, but only a few are designated FQHCs that receive these enhanced reimbursements. Second, many of the THC programs are accredited by the American Osteopathic Association (AOA) and not by the ACGME. Our experience in collaborating with AOA programs in the Washington, Wyoming, Alaska, Montana, and Idaho region has shown that the expenses of AOA family medicine programs have been notably less than those of ACGME programs because of fewer faculty, administrative, and facility requirements. Third, the THC analysis looked primarily at new or expanding programs rather than the “steady state” of established programs, and those costs have significant differences. However, the article focusing on the cost per resident in a THC program came to the same conclusion that we do: ultimately, the cost of residency training, particularly in primary care specialties with large outpatient overhead costs and limited patient care revenues, must be supported by federal GME expenditures, whether through Medicare GME, Medicaid GME, HRSA/THC, or other large funding sources to ensure the future of developing primary care workforce in the future.
Expense per resident has less variability across Network programs than revenue per resident, emphasizing the importance of identifying adequate revenue sources that are stable over time. This includes both appropriate patient care revenues for primary care services provided, as well as state and federal funding sources.
Among the study programs, federal and state revenue streams vary widely and have a major impact; programs with less federal and state funding streams are less financially viable, and subsequently struggle more with program resource allocation and faculty recruitment and retention. Importantly, the establishment of the original resident caps for CMS DGME and IME payments in 1996 codified imbalances in payments among programs depending upon their insights into quantifying the expenses of residency training at that time; these historical imbalances magnify over time as inflation percentage increases have occurred.
Many states and communities are considering starting new residency training programs as a way to address the current or impending physician workforce shortage. The data reported here is for mature programs that have all 3 years of family medicine residents in place, as it is at this point of maturity—when resident productivity is highest and the full amount of CMS GME funding is in place—that the long-term viability of programs is determined. Short-term residency funding and grants can help with program start-up expenses, but tend to underestimate the ability of programs to remain financially stable over the long-term. In considering short-term solutions it is important to acknowledge the long life cycle of a class of residents, with 1 year of recruitment, followed by a number of years of training (three for family medicine, longer for psychiatry and surgical programs). This long start-up period for new programs does raise the question about the possibility of expanding existing programs when possible as a less expensive and faster method of increasing workforce.15
There are limitations to the generalizability of this specific data set. All of these programs are located in the Pacific Northwest. There are known regional variations in many elements of program finances: CMS GME revenues, particularly the per resident amount; state Medicaid financing of GME, where some states make significant contributions and others make none; and payments for patient care services, including baseline payment rates, regional insurance carrier rates, Medicaid and Medicare payment rates, payer mix, the penetration of managed care plans, the presence of advanced practice models, and others. There are known variations within the Network programs that can affect program finances as well, including where programs have expanded over their CMS cap, which would decrease the CMS revenue per resident. However, the underlying expense categories and requirements, and the revenue streams available and their variation over time, reflect universal factors that apply to all primary care training programs.
Current University of Washington Family Medicine Residency Network benchmarking data suggests a cost per resident per year, excluding federal and state GME funding streams, of about $180,000. This amount is significantly more than that noted by the recent paper specific to THC program funding.4 This excess expense compared to revenue must be met by other agencies, whether from CMS, HRSA, state expenditures, or direct local hospital support, through stable long-term commitments to these funding mechanisms to ensure program viability for these essential family medicine programs in the future.
Acknowledgments
Special acknowledgment to Jani McKay, MBA, PHR, CPHR, of MJ McKay Corporation, who conducted the most recent family medicine program surveys and analyzed and compiled the results.
References
- US Department of Health and Human Services Health Resources and Services Administration, National Center for Health Workforce. Projecting the Supply and Demand for Primary Care Practitioners Through 2020; 2013. https://bhw.hrsa.gov/sites/default/files/bhw/nchwa/primarycarebrief.pdf. Accessed October, 2017.
- Dall T, West T, Chakrabarti R, Iacobucci W. The Complexities of Physician Supply and Demand: Projections from 2013 to 2025.; 2017. https://aamc-black.global.ssl.fastly.net/production/media/filer_public/a5/c3/a5c3d565-14ec-48fb-974b-99fafaeecb00/aamc_projections_update_2017.pdf. Accessed October, 2017.
- Petterson SM, Liaw WR, Phillips RL Jr, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010-2025. Ann Fam Med. 2012;10(6):503-509.
https://doi.org/10.1370/afm.1431.
- Petterson SM, Liaw WR, Tran C, Bazemore AW. Estimating the residency expansion required to avoid projected primary care physician shortages by 2035. Ann Fam Med. 2015;13(2):107-114.
https://doi.org/10.1370/afm.1760.
- AMA Builds on Efforts to Expand Funding for Graduate Medical Education [press release] https://www.ama-assn.org/ama-builds-efforts-expand-funding-graduate-medical-education. Chicago: American Medical Association; June 15, 2016. Accessed March 23, 2017.
- AAMC Commends Introduction of GME Expansion Legislation [press release] https://www.aamc.org/newsroom/newsreleases/431072/20150430_2.html. Washington, DC: Association of American Medical Colleges; April 30, 2015.
- Wynn BO, Smalley R, Cordasco KM. Does It Cost More to Train Residents or to Replace Them? A Look at the Costs and Benefits of Operating Graduate Medical Education Programs. Santa Monica, CA: Rand Corporation; 2013. http://www.rand.org/content/dam/rand/pubs/research_reports/RR300/RR324/RAND_RR324.pdf. Accessed March 23, 2017.
- Regenstein M, Nocella K, Jewers MM, Mullan F. The Cost of Residency Training in Teaching Health Centers. N Engl J Med. 2016;375(7):612-614.
https://doi.org/10.1056/NEJMp1607866.
- Carney PA, Waller E, Green LA, et al. Financing Residency Training Redesign. J Grad Med Educ. 2014;6(4):686-693.
https://doi.org/10.4300/JGME-D-14-00002.1.
- Lesko S, Hughes L, Fitch W, Pauwels J. Ten-year trends in family medicine residency productivity and staffing: impact of electronic health records, resident duty hours, and the medical home. Fam Med. 2012;44(2):83-89.
- Lesko S, Fitch W, Pauwels J. Ten-year trends in the financing of family medicine training programs: considerations for planning and policy. Fam Med. 2011;43(8):543-550.
- Pauwels J, Oliveira A. Three-year trends in the costs of residency training in family medicine. Fam Med. 2006;38(6):408-415.
- Pauwels J, Oliveira A, Stevens N. Benchmarking the costs of residency training in family practice. Fam Med. 2003;35(5):330-336. http://www.stfm.org/Portals/49/Documents/FMPDF/FamilyMedicineVol35Issue5Pauwels330.pdf. Accessed March 23, 2017.
- Centers for Medicare & Medicaid Services. Direct Graduate Medical Education. 2017-01-31. https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/dgme.html. Published 2017. Accessed March 23, 2017.
- Ashkin EA, Newton WP, Toomey B, Lingley R, Page CP. Cost of Incremental Expansion of an Existing Family Medicine Residency Program. Fam Med. 2017;49(7):544-547.