Background and Objectives: Procedural training is integral to family medicine residencies. Although accreditation bodies require that family medicine residency programs train residents in procedures relevant to their practices, there are no standards defining the scope of family medicine. We compared the perceived importance of 31 procedures by faculty, residents, and recent graduates of one institution.
Methods: An online survey was sent to current residents and faculty of a large academic family medicine residency, as well as community practitioners who had graduated from that residency within the past 5 years. The survey asked participants to rate how important 31 procedures are for family medicine practices.
Results: The overall response rate was 37%. Most respondents provided outpatient care, and few provided or intended to provide obstetric care. Dermatologic and musculoskeletal procedures were rated as having high importance by all groups, whereas obstetric and inpatient procedures received lower ratings. Residents ascribed higher importance than faculty or recent graduates for nearly all procedures.
Conclusions: Most residents, faculty, and community practitioners provided outpatient care and rated dermatologic and musculoskeletal procedures as important. Inpatient and obstetric care are less common career paths, and related procedures were rated as less important. Resident physicians ascribed greater importance than community practitioners for many procedures, which may be due misperceptions of their future practice needs or imposed requirements for graduation.
Decisions regarding which procedures to emphasize in family medicine training present an ongoing challenge. The Accreditation Council for Graduate Medical Education mandates that family medicine residents “receive training to perform clinical procedures required for their future practices” without specific guidelines.1 Consensus statements by the Council on Academic Family Medicine and the Society of Teachers for Family Medicine Group on Hospital Medicine and Procedural Training list recommended procedures.2,3 These lists are considered a starting point, as programs currently develop their own procedure requirements.
Procedures performed by family doctors vary by geography, demography, and setting. Rural providers may perform more procedures than doctors in urban settings.4-6 Men may perform more procedures than women,5,6 except for gynecologic procedures.7 A national survey revealed that the most common procedures performed by family doctors are skin procedures (73.4%), musculoskeletal injections (64.2%), spirometry (34.3%), and endometrial sampling (30.0%).8 The scope of family practice is decreasing as well. A recent survey revealed that less than 50% of chief residents plan to practice obstetrics.5 Surveys of graduates from the University of Missouri Family and Community Medicine (MUFCM) residency program reveal that the number of graduates practicing obstetrics, inpatient medicine, critical care, or emergency medicine has decreased.5,9
MUFCM recently revised its procedure curriculum, accounting for residents’ goals and likely needs. We conducted a survey to document practice patterns and determine the most important procedures according to residents, faculty, and community practitioners.
The MUFCM residency is a 12/12/12 program. Residents see patients at one of four sites—two rural clinics, one suburban clinic, and one federally qualified health center. Faculty have continuity clinics at these same locations and two additional suburban clinic sites. MUFCM residents rotate on mandatory family medicine inpatient and obstetric services. They are required to perform joint injections, laceration repairs, skin biopsies, circumcisions, vaginal deliveries, and one toenail removal. Faculty may see patients and supervise residents in clinic, on adult or pediatric inpatient services, or obstetric services.
We developed an online Qualtrics survey to assess perceptions of the importance of 31 outpatient, inpatient, pediatric, and obstetric instrument-assisted procedures. Prior to distribution, a faculty panel verified face validity. Respondents rated procedures’ importance as: 1=do not do (faculty and community practitioner only) or not important, 2=somewhat important, and 3=very important or a necessity. We also collected information regarding demographics, practice location, and setting.
The survey was emailed to all current MUFCM residents and faculty, as well as physicians who graduated from MUFCM residency within 5 years and are now employed elsewhere (hereafter, “recent graduates”). One reminder email was sent to all participants. Responses were anonymous, participation was voluntary, and no incentives were offered.
Survey data were downloaded and imported into SAS for Windows 9.4 (SAS Institute, Cary, NC). We calculated mean responses for each category. Because data were ranked, we used the Kruskal-Wallis test to determine whether responses were from the same distribution. Posthoc tests were performed between groups when the initial test was statistically significant and were adjusted by the Bonferroni correction to account for multiple tests. This study was exempted by the University of Missouri Health Sciences Institutional Review Board.
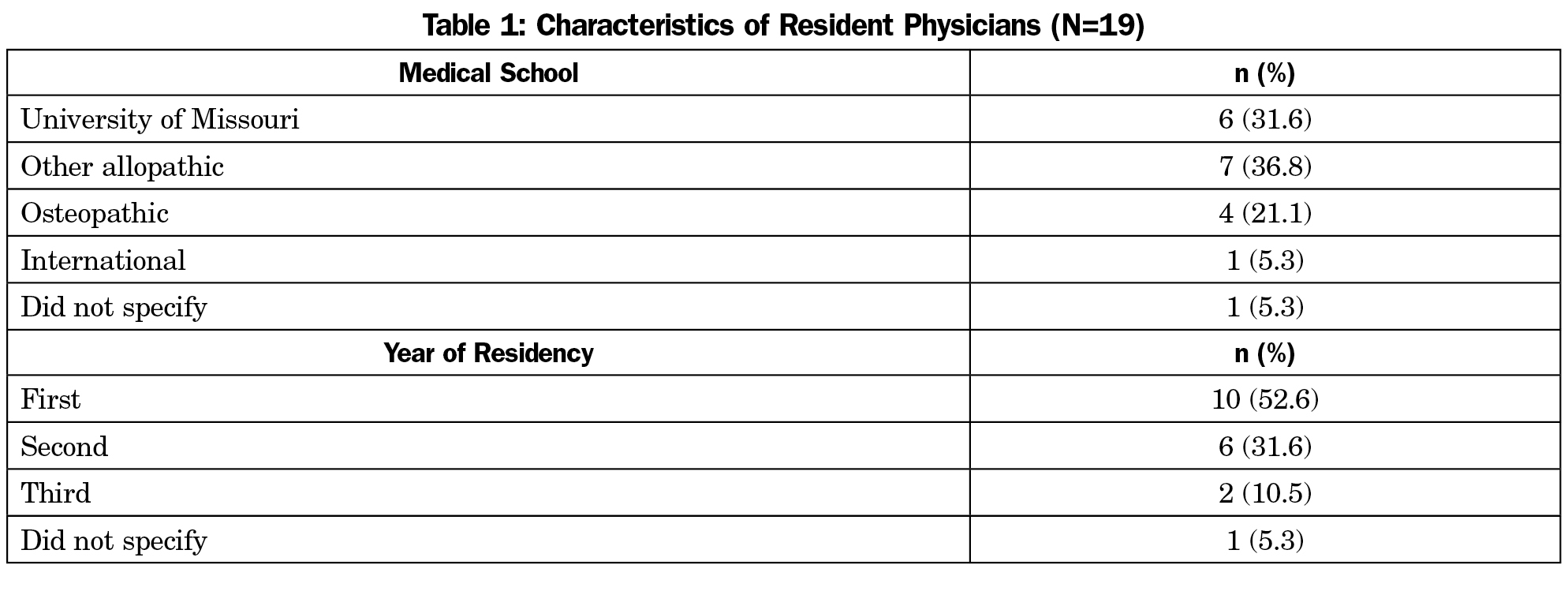
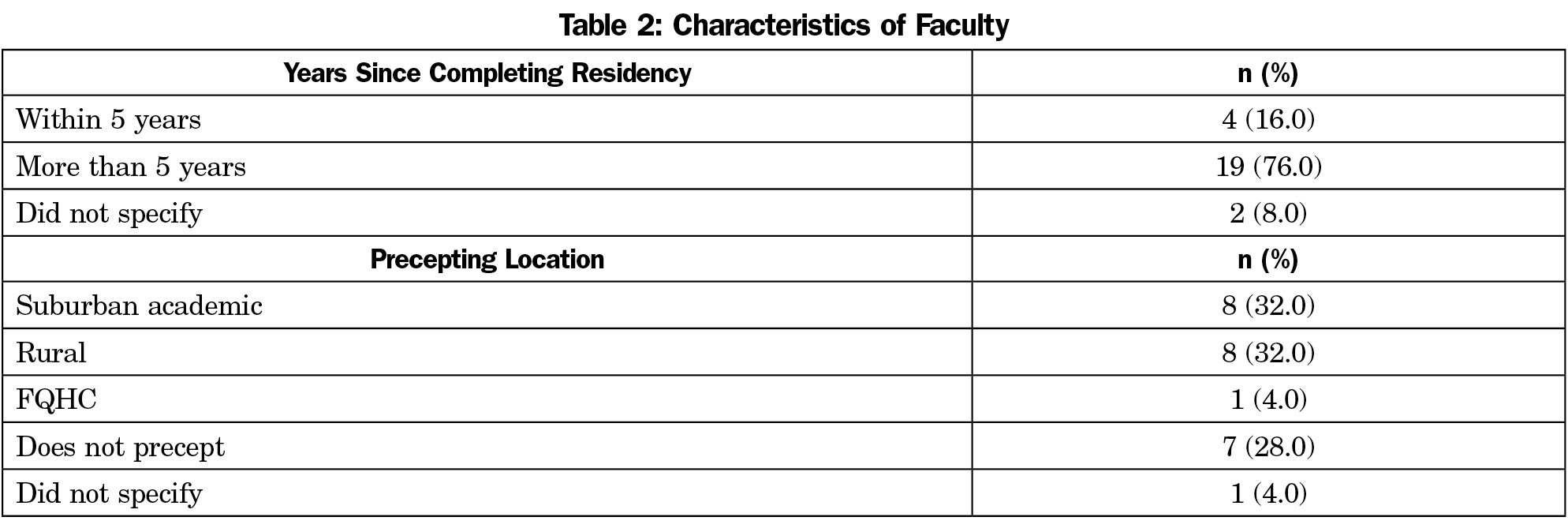
The overall response rate was 37%. Nineteen of 36 residents (53%) responded to the survey (Table 1). Over half of residents who responded were in their first year. Approximately one-third of residents attended medical school at the University of Missouri, and one-third attended another allopathic program. Twenty-five of 89 faculty (29%) and 19 of 47 recent graduates (40%) responded. Most faculty completed residency more than five years ago (Table 2).
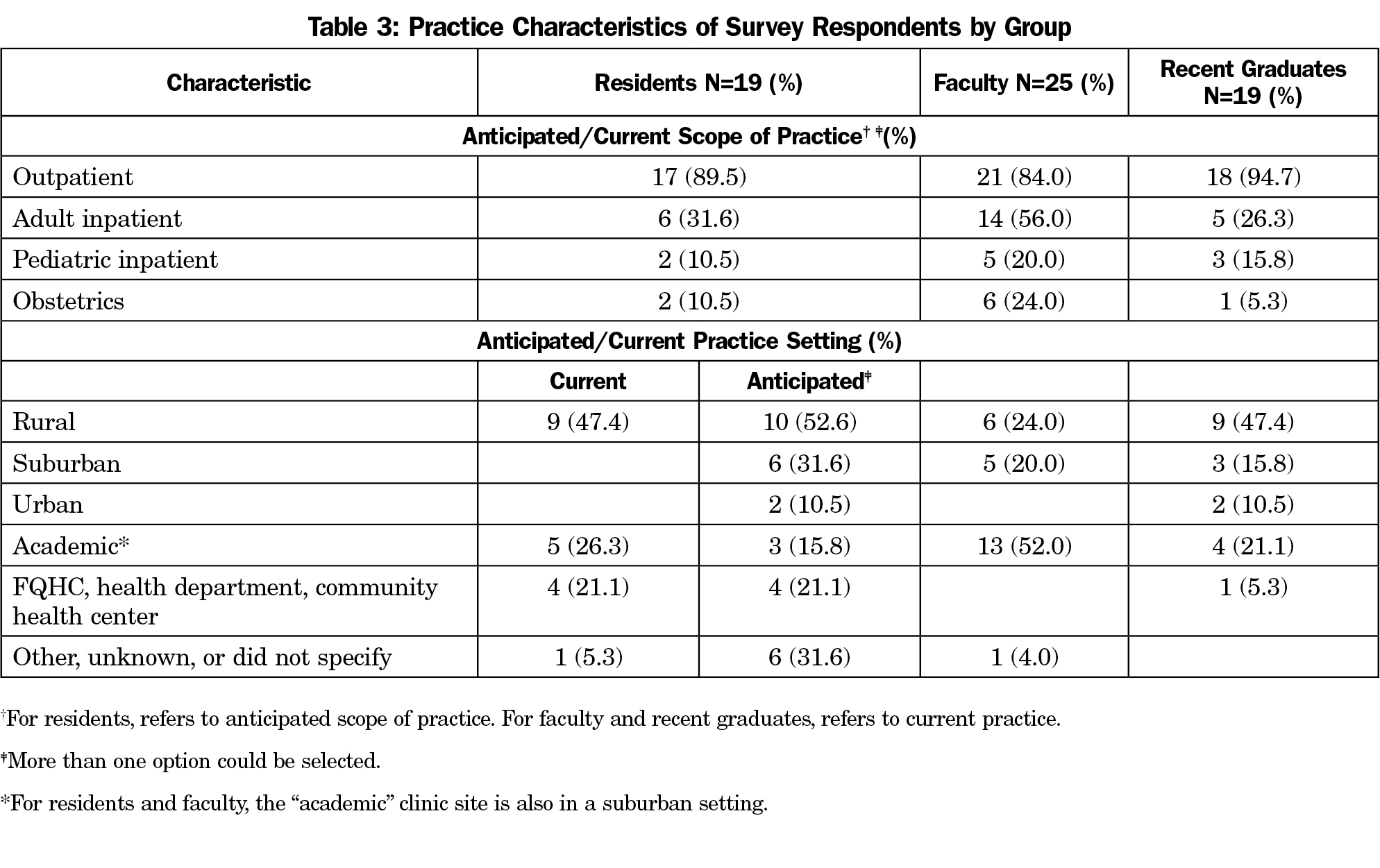
Half of residents and recent graduates practiced in a rural location (Table 3). Most residents anticipated practicing in rural locations. Most faculty practiced in a suburban setting. Nevertheless, all three groups reported higher percentages of rural practice compared to national averages.10 In all three cohorts, most respondents practiced or anticipated practicing outpatient medicine. Fewer practiced or anticipated practicing adult inpatient medicine. Obstetrics and pediatric inpatient medicine were the least frequently endorsed.
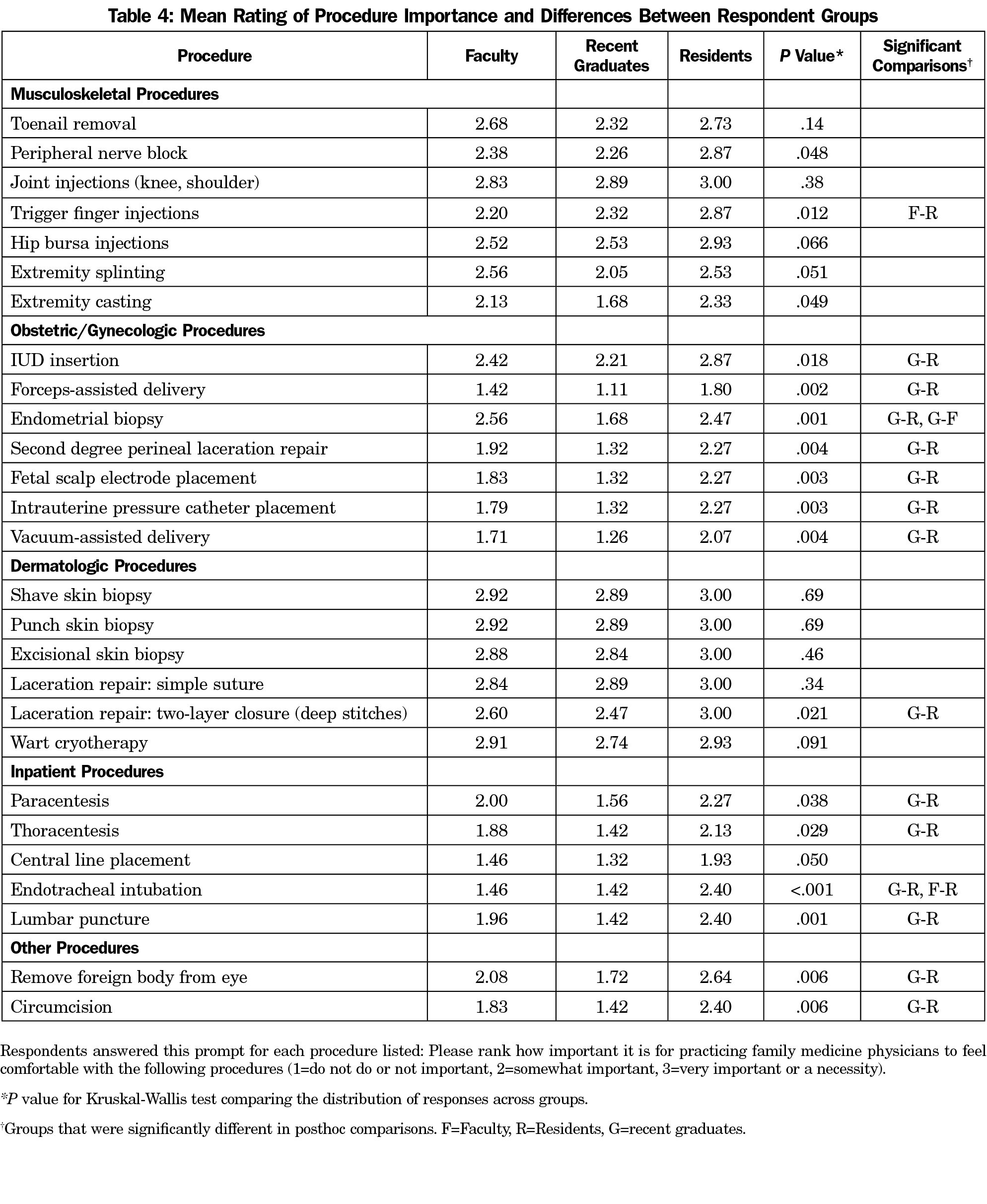
All cohorts rated musculoskeletal and dermatologic procedures as highly important (Table 4). Obstetric and inpatient procedures were rated as less important, especially among recent graduates. Residents ascribed higher importance than faculty or recent graduates for all procedures except extremity splinting and endometrial biopsy. Statistically significant differences between ratings of procedure importance were seen for every obstetric and gynecologic procedure, with residents ascribing highest importance and recent graduates ascribing lowest importance. Similar findings were seen for all inpatient procedures listed except for central line placement, for which all groups assigned low importance.
Our study shows that residents consistently rated procedures, especially inpatient and OB procedures, as more important than recent graduates. Although not statistically significant, resident physicians also consistently rated procedures as more important compared to faculty. Residents may be unaware of factors that may shape their future practice. All residents, but not all faculty, serve on inpatient and obstetric services, which may influence residents’ perceptions.
All groups rated outpatient dermatologic and musculoskeletal procedures as highly important and obstetric and inpatient procedures as less important. Office-based procedures appear to have higher priority. Recent graduates may be influenced by local demography, cost of supplies, financial reimbursement, competition with specialists, or may feel limited by their residency training. Faculty may limit procedures due to time constraints or competing professional obligations. Residents may be influenced by faculty role models.
The scope of family practice, including procedural practice, appears to be narrowing. A 2014 national survey of newly-certifying and recertifying family physicians showed that new graduates anticipate providing a broader scope of practice than current practitioners.11 Despite early ambitions to provide full-scope care, scope of practice—including inpatient, obstetrics, and procedures—narrows soon after residency. Further study is needed to determine how competition with subspecialists, physician reimbursement, or residency training influence the scope of family medicine practice.
The study is limited by the number of respondents. Few third-year residents responded, and first-year residents may have less understanding of their future practice needs. Different faculty practice locations may influence the procedures done in their private clinics. Furthermore, our survey was distributed to physicians currently or previously employed by one institution and may not generalize to other programs.
Nevertheless, it is notable that we found differences regarding procedure importance between current residents and recent graduates of the same institution. This study is unique in that it surveys learners, faculty, and recent graduates to begin to determine the types of procedures valuable for family medicine. As accreditation bodies reassess procedural training, they may consider whether residencies should encourage full-scope practice or focus on common practice trends. For individual programs, it may be worthwhile to consider practice patterns of graduates as a starting point. More investigation is recommended to make procedure training more relevant.
Acknowledgments
Presented at the University of Missouri, Department of Family and Community Medicine, June 14th, 2017.
References
- Accreditation Council for Graduate Medical Education. ACGME Program requirements for graduate medical education in family medicine. Effective July 1, 2017. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/120_family_medicine_2017-07-01.pdf?ver=2017-06-30-083354-350. Accessed October 11, 2017.
- Association of Family Medicine Residency Directors. CAFM consensus statement for procedural training in family medicine residency. https://afmrd.socious.com/page/procedures. Accessed March 29, 2017.
- Kelly BF, Sicilia JM, Forman S, Ellert W, Nothnagle M. Advanced procedural training in family medicine: a group consensus statement. Fam Med. 2009;41(6):398-404.
- Goertzen J. Learning procedural skills in family medicine residency: comparison of rural and urban programs. Can Fam Physician. 2006;52:622-623.
- Sharp LK, Wang R, Lipsky MS. Perception of competency to perform procedures and future practice intent: a national survey of family practice residents. Acad Med. 2003;78(9):926-932. https://doi.org/10.1097/00001888-200309000-00019.
- Tucker W, Diaz V, Carek PJ, Geesey ME. Influence of residency training on procedures performed by South Carolina family medicine graduates. Fam Med. 2007;39(10):724-729.
- MacKenzie MS, Berkowitz J. Do procedural skills workshops during family practice residency work? Can Fam Physician. 2010;56(8):e296-e301.
-
American Academy of Family Physicians. Table 14: Clinical procedures performed by physicians at their practice. https://www.aafp.org/about/the-aafp/family-medicine-facts/table-12(rev).html. Accessed October 11, 2017.
- Ringdahl E, Delzell JE Jr, Kruse RL. Changing practice patterns of family medicine graduates: a comparison of alumni surveys from 1998 to 2004. J Am Board Fam Med. 2006;19(4):404-412. https://doi.org/10.3122/jabfm.19.4.404.
-
American Academy of Family Physicians. Table 2: Demographic characteristics of AAFP members. https://www.aafp.org/about/the-aafp/family-medicine-facts/table-2.html. Accessed December 19, 2017.
- Coutinho AJ, Cochrane A, Stelter K, Phillips RL, Jr., Peterson LE. Comparison of intended scope of practice for family medicine residents with reported scope of practice among practicing family physicians. JAMA. 2015;314(22):2364-2372. https://doi.org/10.1001/jama.2015.13734.



There are no comments for this article.