Background and Objectives: Behavioral health integration (BHI) in primary care settings is critical to mental health care in the United States. Family medicine resident experience in BHI in family medicine residency (FMR) continuity clinics is essential preparation for practice. We surveyed FMR program directors to characterize the status of BHI in FMR training.
Methods: Using the Council of Academic Family Medicine Educational Research Alliance (CERA) 2017 survey, FMR program directors (n=478, 261 respondents, 54.6% response rate) were queried regarding the stage of BHI within the residency family medicine center (FMC), integration activities at the FMC, and the professions of the BH faculty. BHI was characterized by Substance Abuse and Mental Health Services Agency (SAMHSA) designations within FMRs, and chi-square or ANOVA with Tukey honest significant difference (HSD) post hoc testing was used to assess differences in reported BHI attributes.
Results: Program directors reported a high level of BHI in their FMCs (44.1% full integration, 33.7% colocated). Higher levels of BHI were associated with increased use of warm handoffs, same day consultation, shared health records, and the use of behavioral health (BH) professionals for both mental health and medical issues. Family physicians, psychiatrists, and psychologists were most likely to be training residents in BHI.
Conclusions: Almost half of FMR programs have colocated BH care or fully integrated BH as defined by SAMHSA. Highly integrated FMRs use a diversity of behavioral professionals and activities. Residencies currently at the collaboration stage could increase BH provider types and BHI practices to better prepare residents for practice. Residencies with full BHI may consider focusing on supporting BHI-trained residents transitioning into practice, or disseminating the model in the general primary care community.
Primary care has been the principal mental health system for decades, delivering up to 80% of psychiatric care in the United States.1 Family medicine has embraced this central role of providing quality behavioral health (BH) care. The Accreditation Council on Graduate Medical Education requires significant behavioral training during family medicine residency (FMR),2 and FMR graduates deliver more BH care than other primary care specialties.3
Despite this, BH care in primary care clinics has been limited in quality and reach.4,5 Integration of behavioral health professionals into primary care settings is a major organizational strategy that addresses gaps in mental health care.6 Behavioral health integration (BHI) has been found to improve patient satisfaction,7 reduce costs,8 and improve social function for patients with depression.9 In 2013, SAMSHA described six levels of BHI grouped into three broad categories: collaboration, colocation, and integration. Collaboration is characterized by physically distant primary care and behavioral providers with varying communication. Colocation describes physical proximity with diverse care structures. Full integration is intentional team care with warm handoffs, shared records, and multidisciplinary care coordination.10
FMRs are integrating BHI into their continuity clinics and curriculum, but research on BHI curricula and penetration is sparse.11 BHI training in family medicine residencies (FMRs) increases resident knowledge and confidence,12 and residents identify working with interdisciplinary behavioral providers as a strength of a BH rotation.13 Educators have proposed model BHI curricula for medical and psychiatry residents.14 After one pilot program, 97% of residents reported an intention to practice integrated care after graduation.15 Assessment of the current state of BHI in FMRs across the country will better inform curriculum. We surveyed program directors about BHI in the family medicine centers (FMCs) where residents provide continuity care, including the degree of integration, training activities, and type of educators involved in residency-based BHI curricula. We aimed to characterize the degree of BHI and its relationship to BH activities and teachers in FMRs.
Measures
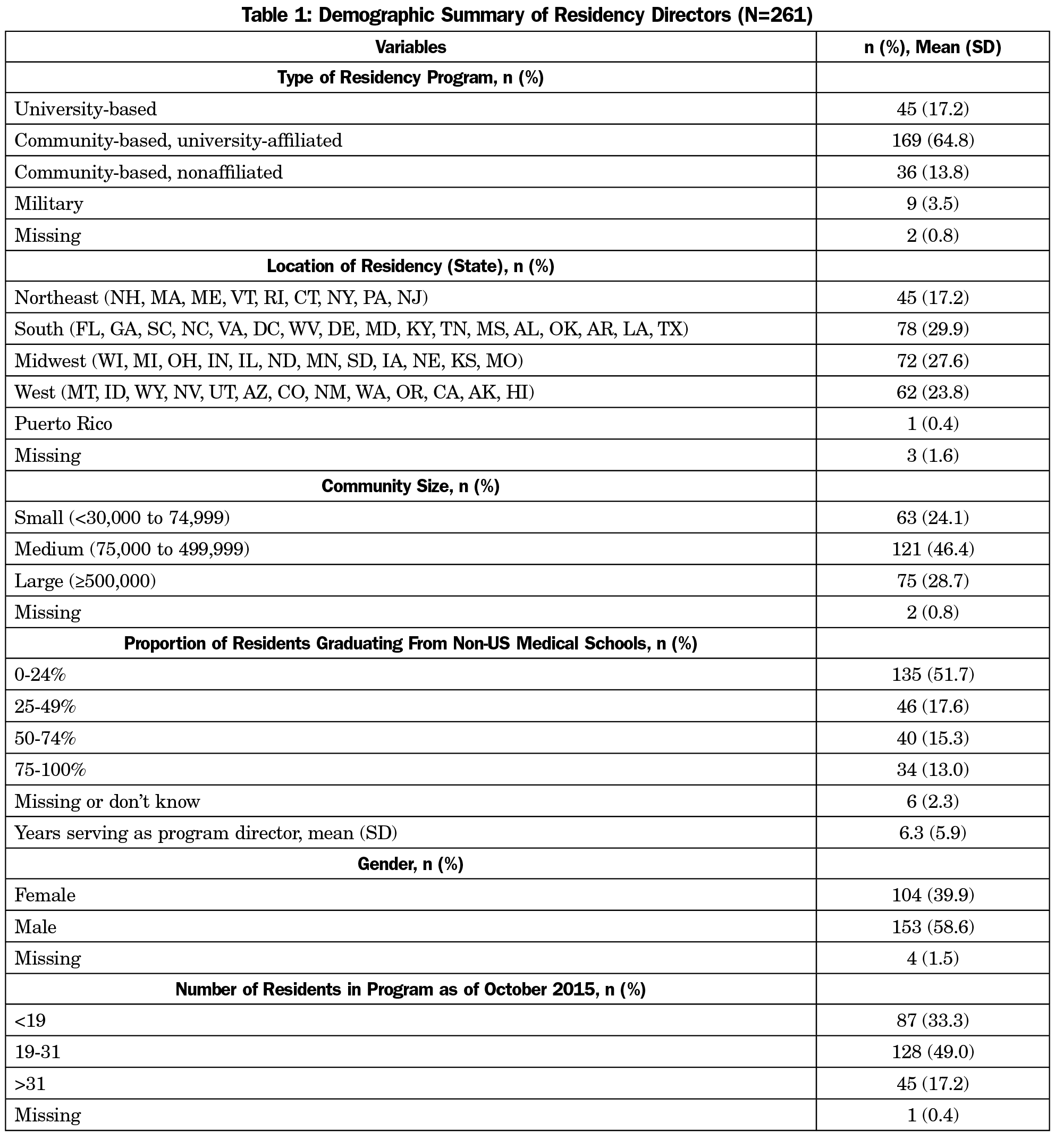
FMR program directors were emailed a link to the 2017 CERA survey.16,17 A total of 261 of 478 (45%) of program director members of the Council of Academic Family Medicine contacted completed the survey. Table 1 details the demographic questions including residency type, region, community size, residency size, and program director characteristics.
Participants selected one of six multiple-choice descriptions of BHI at the residency’s FMC which were then compressed into a three-tiered model following the SAMHSA framework. Minimal coordination and basic collaboration at a distance were grouped as collaboration. Basic collaboration onsite and close collaboration onsite with some systemic integration were grouped as colocation. Close collaboration approaching an integrated practice and full collaboration in a transformed/merged practice were grouped as full integration.10 Respondents indicated which BH activities occurred in the FMC and which types of professional providers taught BH to residents. This CERA study was approved by the American Academy of Family Physicians Institutional Review Board.
Analysis
Characteristics of program directors and BHI questions were summarized using one-way frequencies and means. Associations between the reported degree of BHI offered (collaboration vs colocated vs full integration) and characteristics of BHI offered at sites were assessed using chi-square tests for categorical variables and one-way ANOVA with Tukey honest significant difference (HSD) post hoc comparisons for continuous variables. If cell sizes less than five were present for categorical variable comparisons, Fisher exact tests were used. All analyses were conducted at an alpha=0.05 level using SAS v9.4 (SAS Institute, Cary, NC).
Table 1 describes the demographics of the program directors and FMRs. FMRs most often were community-based with a university affiliation, in a medium-size community, with 19 to 31 residents. FMRs from the Northeast were the smallest proportion of the sample.
Table 2 demonstrates that most FMRs reported either colocated (33.7%) or fully integrated BH care (44.1%). About 90% of FMCs had more than one type of BH faculty. Family physicians and psychiatrists most frequently taught BH skills, while licensed counselors and marriage and family therapists were least utilized. There was no significant difference in the degree of integration by program type, geographic region, community size, or program size (results not shown).
Table 3 demonstrates that the use of all individual BHI activities in FMRs was positively associated (all P<.003) with increased degree of BHI. Average number of different BH activities also increased with degree of collaboration (P<.0001). A greater proportion of both fully integrated (75.7%) and colocated (71.6%) programs used psychologists to teach BH compared to collaborative programs (43.8%) but no other differences in types of professionals were found. The mean number of BH educator types was similar for colocated and fully integrated programs (3.3 and 3.6, respectively) with both significantly higher when compared to collaborative programs (mean=2.6).
Most FMR program directors in this study report colocated or fully integrated BH care in their FMCs, and most FMRs provide residents with training from at least three different types of BH professionals. This high level of integration was seen across all program types and regions. This high penetration of BHI into FMR education was simultaneously surprising and reassuring to the authors.
The 12.3% of programs in the collaboration phase notably lack warm handoffs, same-day consultation, and shared electronic health records. Those residencies differ from more integrated residencies in the absence of psychologists, social workers, licensed counselors or marriage or medical family therapists. Inclusion of these processes and personnel would advance their BHI.
Programs were generally low in psychiatry exposure and population health. Previous work indicated that family medicine residents perceive a lack of pharmacology and family systems education during residency.13 The diversity of BH teachers indicated in this study may be better targeted to fill those gaps.
Residencies with full BHI may consider using a similar interprofessional model to provide health care in other areas, or focusing on supporting BHI-trained residents with the transition into practice.
This study was limited by the sample size and self-report design. Objective assessment of BHI within FMR clinics would add validity to the initial characterization described here.
This study demonstrates that the concept and practice of BHI in FMRs is now well established. Maximization of each of these elements of BHI can improve patient care in the FMR clinic, and better prepare family medicine residents to enter a practice that provides behavioral health care in the primary care setting.
Acknowledgments
The authors wish to thank Kent Bream and Mario DeMarco from the University of Pennsylvania’s Department of Family Medicine and Community Health for their contributions to the conceptual development of the survey and conceptual models driving analyses, and Ian Bennett as our CERA mentor.
Funding: This project was supported by the Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (HHS) under grant T0BHP30018 (Drs Jacobs and Brieler) and UH1HP29964 (Drs Betancourt and Cronholm) for Primary Care Training and Enhancement. This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the US Government.
References
- Regier DA, Goldberg ID, Taube CA. The de facto US mental health services system: a public health perspective. Arch Gen Psychiatry. 1978;35(6):685-693. https://doi.org/10.1001/archpsyc.1978.01770300027002.
- Accreditation Council for Graduate Medical Education. ACGME program requirements in family medicine. http://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/120_family_medicine_2017-07-01.pdf?ver=2017-06-30-083354-350Accessed8/17/17.
- Brieler JA, Scherrer JF, Salas J. Differences in prescribing patterns for anxiety and depression between General Internal Medicine and Family Medicine. J Affect Disord. 2015;172:153-158. https://doi.org/10.1016/j.jad.2014.09.056.
- Stein MB, Sherbourne CD, Craske MG, et al. Quality of care for primary care patients with anxiety disorders. Am J Psychiatry. 2004;161(12):2230-2237. https://doi.org/10.1176/appi.ajp.161.12.2230.
- Bradford DW, Kim MM, Braxton LE, Marx CE, Butterfield M, Elbogen EB. Access to medical care among persons with psychotic and major affective disorders. Psychiatr Serv. 2008;59(8):847-852. https://doi.org/10.1176/ps.2008.59.8.847.
- American Psychiatric Association. Dissemination of integrated care within adult primary care settings. 2016. https://www.integration.samhsa.gov/integrated-care-models/APA-APM-Dissemination-Integrated-Care-Report.pdf Accessed November 29, 2017.
- Solberg LI, Crain AL, Maciosek MV, et al. A stepped-wedge evaluation of an initiative to spread the collaborative care model for depression in primary care. Ann Fam Med. 2015;13(5):412-420. https://doi.org/10.1370/afm.1842.
- Fisher L, Dickinson WP. Psychology and primary care: new collaborations for providing effective care for adults with chronic health conditions. Am Psychol. 2014;69(4):355-363. https://doi.org/10.1037/a0036101.
- Woltmann E, Grogan-Kaylor A, Perron B, Georges H, Kilbourne AM, Bauer MS. Comparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: systematic review and meta-analysis. Am J Psychiatry. 2012;169(8):790-804. https://doi.org/10.1176/appi.ajp.2012.11111616.
- Heath B, Wise Romero P, and Reynolds K. A review and proposed standard framework for levels of integrated healthcare. Washington, DC: SAMHSA-HRSA Center for Integrated Health Solutions. March 2013. https://www.integration.samhsa.gov/integrated-care-models/A_Standard_Framework_for_Levels_of_Integrated_Healthcare.pdf. Accessed November 25, 2017.
- Blount FA, Miller BF. Addressing the workforce crisis in integrated primary care. J Clin Psychol Med Settings. 2009;16(1):113-119. https://doi.org/10.1007/s10880-008-9142-7.
- Hemming P, Hewitt A, Gallo JJ, Kessler R, Levine RB. Residents’ confidence providing primary care with behavioral health integration. Fam Med. 2017;49(5):361-368.
- Zubatsky M, Brieler J, Jacobs C. Training experiences of family medicine residents on beavioral health rotations. Fam Med. 2017;49(8):635-639.
- Smith RC, Laird-Fick H, D’Mello D, et al. Addressing mental health issues in primary care: an initial curriculum for medical residents. Patient Educ Couns. 2014;94(1):33-42. https://doi.org/10.1016/j.pec.2013.09.010.
- Hill JM. Behavioral health integration: transforming patient care, medical resident education, and physician effectiveness. Int J Psychiatry Med. 2015;50(1):36-49. https://doi.org/10.1177/0091217415592357.
- US Census Bureau. Census Regions and Divisions of the United States. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf. Accessed August 28, 2017.
- Mainous AG III, Seehusen D, Shokar N. CAFM Educational Research Alliance (CERA) 2011 Residency Director survey: background, methods, and respondent characteristics. Fam Med. 2012;44(10):691-693.





There are no comments for this article.