Background and Objectives: The Warren Alpert Medical School of Brown University (AMS) recently implemented a novel dual degree MD-ScM program in primary care and population medicine (PC-PM) that enrolls up to 24 of its nearly 144 yearly matriculants. The overarching goal of this track is to train medical students to become physician leaders who focus on issues in population medicine within primary care.
Methods: We conducted a baseline assessment of the students enrolled in this parallel track in comparison to our traditional students to identify characteristics of and group differences between students in the PC-PM program and traditional students. Data was collected from first-year students matriculating in the 2015 and 2016 academic years (N=277) using portions of nine validated surveys with an emphasis on caring for the underserved and cultural competence, professionalism, working in interprofessional teams, tolerance of ambiguity, empathy, patient-provider interactions, and patient safety/quality improvement.
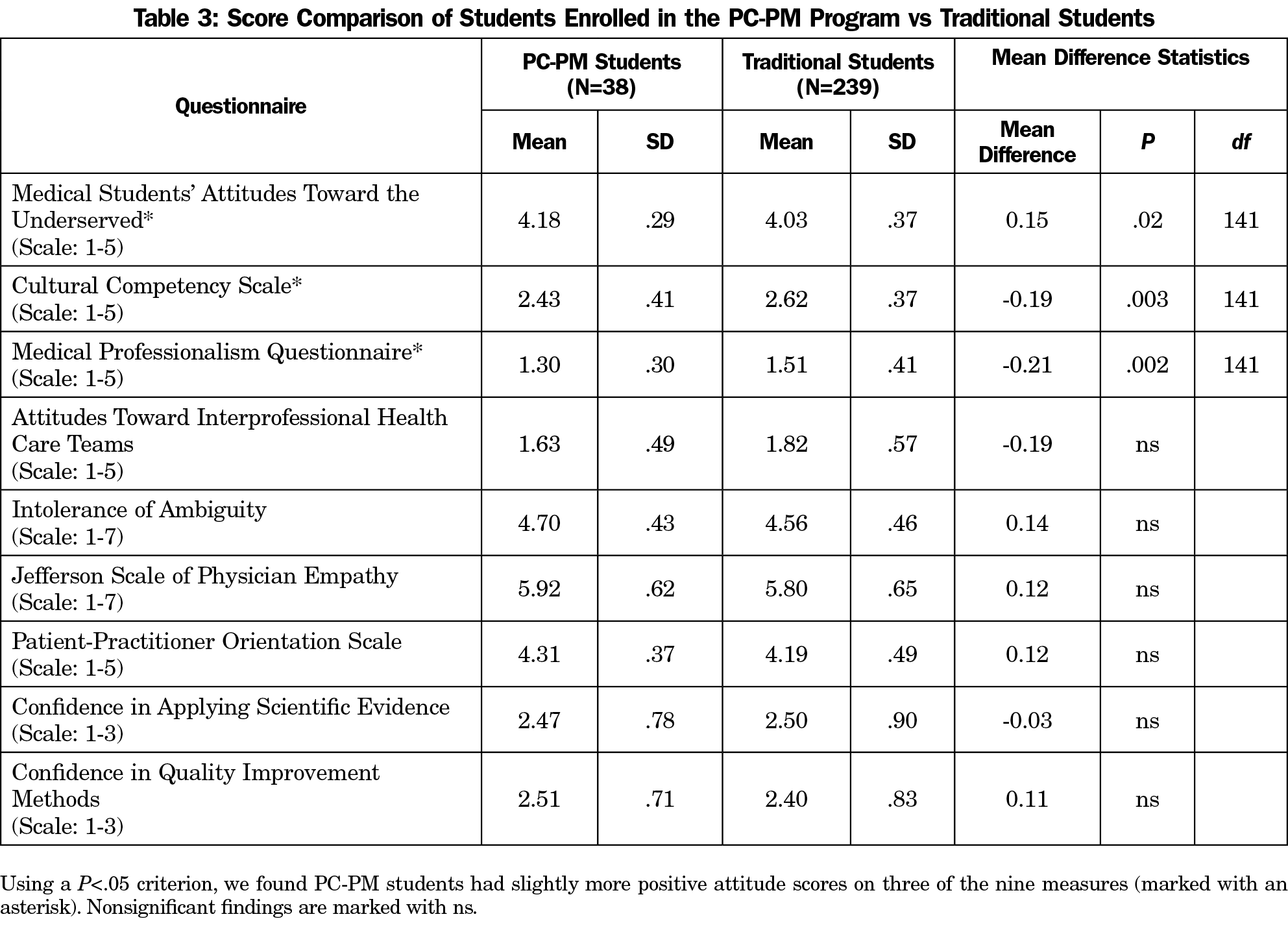
Results: We identified slightly higher significant baseline differences on three scales in which the PC-PM students (n=38) were higher than those in the traditional track students (n=239). These measured cultural competency (t[275]=-3.05, P=.003), professionalism (t[273]=-3.10, P=.002), and attitudes toward working with underserved populations (t[267]=2.31, P=.02).
Conclusions: The higher differences for these three elements may be important to the success of the PC-PM program. We plan to track the growth of the PC-PM students as well as our traditional students through their 4 years of medical school to investigate growth and development throughout the academic career.
Medical education in the United States must continuously evolve to meet the rapidly changing needs of the American health care system. With the advent of the triple aim, health care professionals must strive to improve patient outcomes and patient experience while reducing per capita costs.1 To meet these goals, students must now gain competence in a “third pillar of medical education,” namely health system science, which encompasses knowledge, attitudes, and skills needed to function in the current health care environment, including interdisciplinary teamwork, leadership, and quality improvement.2-5
There will be an estimated primary care physician shortage of 33,000 by the year 2035, and the percentage of US graduates going into primary care continues to decline.6,7 To begin to address these challenges, the Warren Alpert Medical School (AMS) of Brown University developed the dual-degree PC-PM program.8 The goal of the PC-PM program is to increase the number of physicians in primary care by preparing this subset of students for leadership roles in health care ranging from primary care clinical service to research, education, and health policy. This program was founded at AMS due to our institutional history as a primary care medical school and obtaining a grant from the American Medical Association (AMA) as part of the Accelerating Change in Medical Education initiative.8 A separate paper details the vision of the program, including the drive for the program to be innovative, scholarly, evidence-based, unique, and integrated with existing medical education.8
Students who wish to apply for the PC-PM program complete a secondary application geared toward health care reform during the standard medical school application timeline and are interviewed by program administrators to evaluate the fit between the student’s goals and the goals of the program. Up to 24 students annually complete the unique 4-year curriculum that integrates a Master of Science in Population Medicine (ScM) with nine additional courses (integrated when possible) and clinical experiences for the medical degree.
To evaluate differences and to obtain a profile of our class as a whole, we surveyed the 2015 and 2016 matriculating classes of medical students at AMS using portions of nine validated questionnaires to characterize the attitudes, skills, and learning styles of students. The purpose of this study was to identify differences in attitudes between traditional-track students and those enrolled in the PC-PM program at baseline and assess whether any differences remain the same, grow, or narrow over the course of the program, to inform program development and evaluation.
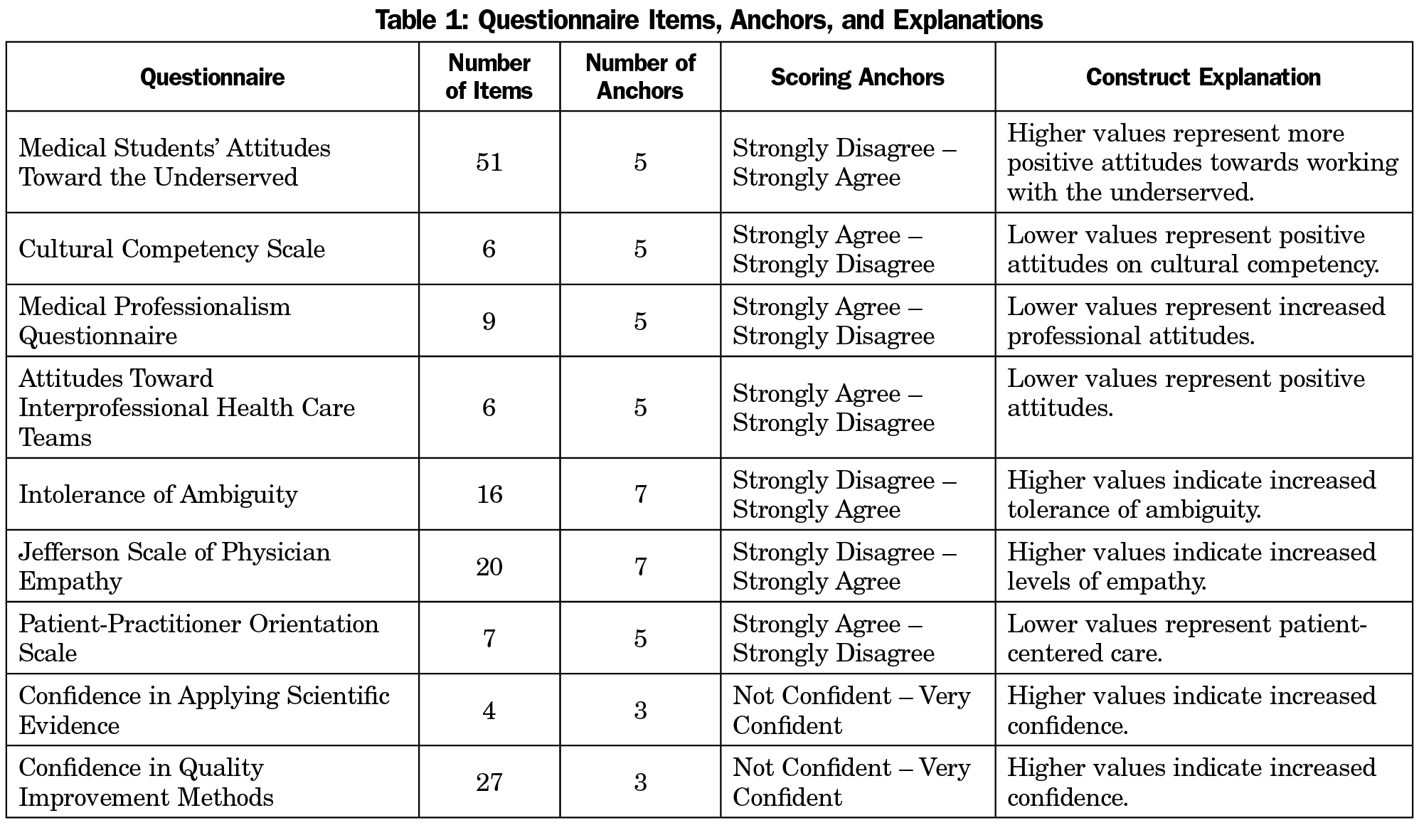
First-year medical students from the 2015 and 2016 entering classes (N=277) completed portions of previously validated questionnaires (described elsewhere) that were chosen as a method to monitor outcomes of the PC-PM program (Table 1): The Medical Students’ Attitudes Toward the Underserved (MSATU),9,10 The Cultural Competency Scale,11 the Medical Professionalism Questionnaire (MPQ),12 Attitudes Toward Health Care Teams Scale,13 Brudner Intolerance of Ambiguity scale,14 Jefferson Scale of Physician Empathy,15 and Patient-Practitioner Orientation Scale (PPOS).16 Since we chose portions of validated surveys, we are not be able to directly compare our results with the same methodological rigor to existing literature. However, our goal was to compare our traditional-track student responses with those of the students in the PC-PM program, thus the methods were adequate for our use. The Brown University Institutional Review Board determined this study did not require review.
Analysis was conducted with the Statistical Package for the Social Sciences (IBM, SPSS, v.24). Mean scores on the MSATU subscales were combined in analyses to control for Type I error. Mean scores on the Cultural Competency Scale, MPQ, Attitudes Toward Interprofessional Health Care Teams, Tolerance of Ambiguity, the Jefferson Scale of Physician Empathy, and the PPOS were included in analyses. Quality improvement items were used to calculate two mean scores to indicate confidence in using scientific evidence and confidence in quality improvement methods. Student scores on each of the scales were delineated by PC-PM program versus traditional-track status to identify baseline differences. Independent sample t-tests were conducted across all variables to contrast traditional-track students versus PC-PM students.
Of first-year students who participated in the survey (N=277), approximately half identified as female (50.5%, n=141) and as white (52.1%, n=146). Students also identified as Asian (23.6%, n=66), black or African-American (7.5%,n=21) and Hispanic/Latino (10.7%, n=30). Approximately half of our students entered our medical school through the standard route (57.1%, n=160), while a third (33.2%, n=93) entered through the Program in Liberal Medical Education (PLME) route. The PLME route is an 8-year program where high school students are accepted to Brown University to complete their Baccalaureate degree, and once finishing and meeting university requirements, are enrolled at AMS.
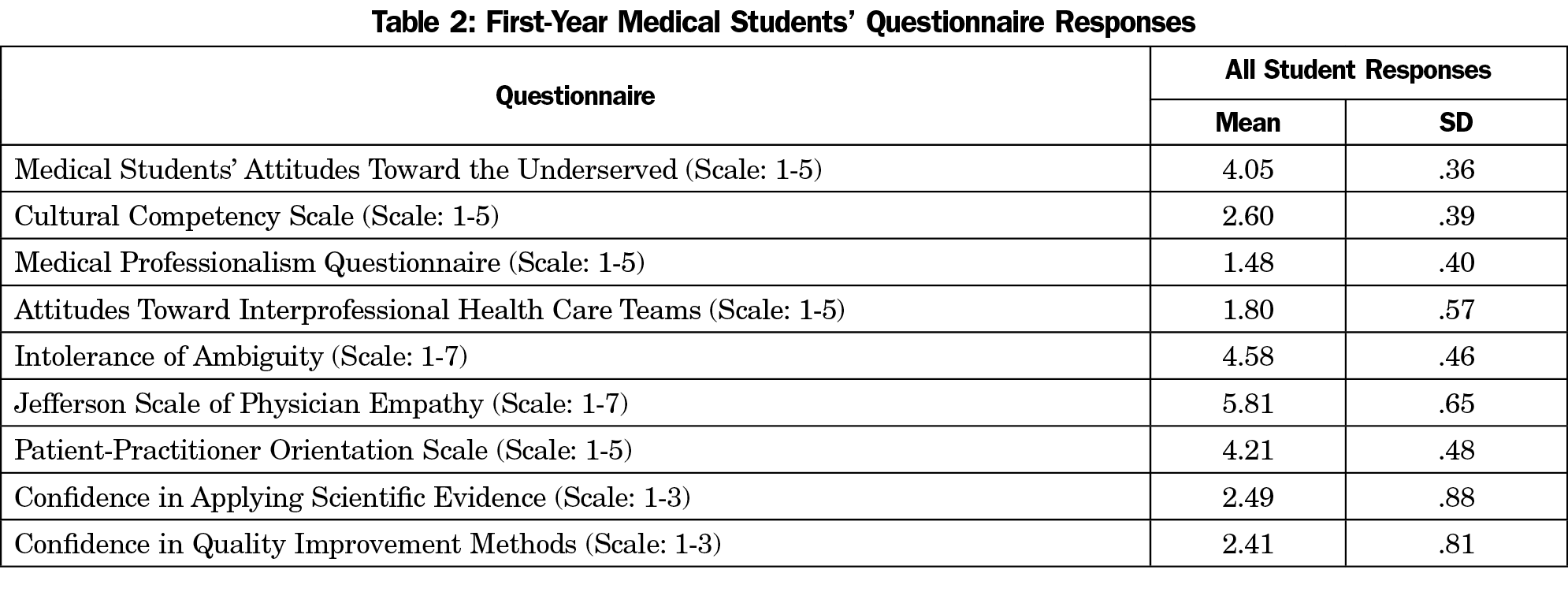
Mean questionnaire scores for all students are shown in Table 2. At baseline, PC-PM students scores differed significantly on three of the nine measures (Table 3).
Results from portions of nine validated questionnaires showed students enrolled in the PC-PM program demonstrated significantly different scores on items from the Cultural Competency Scale, MSATU, and the MPQ. This translates to increased positive attitudes toward cultural competency, higher positive attitudes toward working with underserved populations, and increased professionalism. This is not surprising, given that students enrolled in the program were selected based on an expressed interest in careers in population health and held strong population health-related values, and may bring additional life experiences prior to enrolling in medical school that facilitate increased cultural competence and professionalism. Existing literature on personality factors and specialty choice revealed family practitioners (ie, physicians in primary care) scored higher on a personality measure of abstractedness (eg, creativity) than surgeons and anesthesiologists.17 Research has shown that personality tests completed by first-year medical students can be used to predict entrance to person versus technique-oriented specialization, but that values did not significantly predict type of specialty, though the authors call for more research in this area.18
The implications for increased scores reported by the PC-PM students indicates a need to monitor changes moving forward, to determine whether the scores continue to increase, or remain stable when compared to traditional track students. We also plan to track students as alumni to determine where and in what areas students practice (eg, clinical practice, research, health policy).
We used portions of nine validated surveys to reduce response fatigue, therefore our results cannot be directly compared to existing literature and do not have the same reliability and validity values as the original instrument. Earning the dual degree through completing the thesis is a required portion of the program. It would be interesting to see how the curriculum alone impacts students’ goals and career choices. Additionally, the responses provided here were derived from students at a private medical school in the northeastern United States, limiting generalizability to other institutions.
Acknowledgments
Financial support was provided by the American Medical Association Accelerating Change in Medical Education program.
This paper was at Warren Alpert Medical School of Brown University MedEd Faculty Development Workshop, April, 2017, Providence, RI; the American Medical Association Change In Medical Education Consortium, March, 2017, Phoenix, AZ; and the Society of Teachers in Family Medicine Conference on Medical Student Education, February, 2017, Anaheim, CA.
References
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759-769. https://doi.org/10.1377/hlthaff.27.3.759.
- Varkey P, Peloquin J, Reed D, Lindor K, Harris I. Leadership curriculum in undergraduate medical education: a study of student and faculty perspectives. Med Teach. 2009;31(3):244-250. https://doi.org/10.1080/01421590802144278.
- Boonyasai RT, Windish DM, Chakraborti C, Feldman LS, Rubin HR, Bass EB. Effectiveness of teaching quality improvement to clinicians: a systematic review. JAMA. 2007;298(9):1023-1037. https://doi.org/10.1001/jama.298.9.1023.
- George P, Park YS, Ip J, Gruppuso PA, Adashi EY. The association between premedical curricular and admission requirements and medical school performance and residency placement: A study of two admission routes. Acad Med. 2016;91(3):388-394. https://doi.org/10.1097/ACM.0000000000000922.
- Lown BA, McIntosh S, Gaines ME, McGuinn K, Hatem DS. Integrating compassionate, collaborative care (the “Triple C”) into health professional education to advance the triple aim of health care. Acad Med. 2016;91(3):310-316. https://doi.org/10.1097/ACM.0000000000001077.
- Petterson SM, Liaw WR, Tran C, Bazemore AW. Estimating the residency expansion required to avoid projected primary care physician shortages by 2035. Ann Fam Med. 2015;13(2):107-114. https://doi.org/10.1370/afm.1760..
- Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff (Millwood). 2010;29(5):799-805. https://doi.org/10.1377/hlthaff.2010.0026.
- George P, Tunkel AR, Dollase R, et al. The primary care-population medicine program at the Warren Alpert Medical School of Brown University. R I Med J (2013). 2015;98(9):16-21.
- Crandall SJS, Volk RJ, Loemker V. Medical students’ attitudes toward providing care for the underserved. Are we training socially responsible physicians? JAMA. 1993;269(19):2519-2523. https://doi.org/10.1001/jama.1993.03500190063036.
- Crandall SJS, Volk RJ, Cacy D. A longitudinal investigation of medical student attitudes toward the medically indigent. Teach Learn Med. 1997;9(4):254-260. https://doi.org/10.1207/s15328015tlm0904_2.
- Godkin MA, Savageau JA. The effect of a global multiculturalism track on cultural competence of preclinical medical students. Fam Med. 2001;33(3):178-186.
- Blackall GF, Melnick SA, Shoop GH, et al. Professionalism in medical education: the development and validation of a survey instrument to assess attitudes toward professionalism. Med Teach. 2007;29(2-3):e58-e62. https://doi.org/10.1080/01421590601044984.
- Heinemann GD, Schmitt MH, Farrell MP, Brallier SA. Development of an attitudes toward health care teams scale. Eval Health Prof. 1999;22(1):123-142. https://doi.org/10.1177/01632789922034202.
- Budner S. Intolerance of ambiguity as a personality variable. J Pers. 1962;30(1):29-50. https://doi.org/10.1111/j.1467-6494.1962.tb02303.x.
- Hojat M, Mangione S, Nasca TJ, et al. The Jefferson Scale of Physician Empathy: development and preliminary psychometric data. Educ Psychol Meas. 2001;61(2):349-365. https://doi.org/10.1177/00131640121971158.
- Krupat E, Rosenkranz SL, Yeager CM, Barnard K, Putnam SM, Inui TS. The practice orientations of physicians and patients: the effect of doctor-patient congruence on satisfaction. Patient Educ Couns. 2000;39(1):49-59. https://doi.org/10.1016/S0738-3991(99)00090-7.
- Borges N, Osmon W. Personality and medical specialty choice: technique orientation versus people orientation. J Vocat Behav. 2001;58(1):22-35. https://doi.org/10.1006/jvbe.2000.1761.
- Taber B, Hartung PJ, Borges N. Personality and values as predictors of medical specialty choice. J Vocat Behav. 2011;78(2):202-209. https://doi.org/10.1016/j.jvb.2010.09.006.



There are no comments for this article.