Background and Objectives: Pharmacist inclusion in patient-centered medical home (PCMH) teams has been shown to benefit both patients and practices. However, pharmacists’ inclusion on these teams is not widespread, partly because the work they do is not well known. The Successful Collaborative Relationships to Improve PatienT care (SCRIPT) project was started in August 2009 to understand the clinical and economic impact of pharmacists providing direct patient care. The objective of this study was to describe the work of pharmacists practicing as integrated members of the patient care team within PCMHs through retrospective analysis of their patient care documentation over a 4-year time frame. Two pharmacists were placed into four suburban medical home practices in Pittsburgh, Pennsylvania to perform comprehensive medication management (CMM). These pharmacists documented their CMM encounters in an electronic health record and a database for reporting purposes.
Methods: This study is a retrospective, descriptive analysis of pharmacist-documented CMM encounters from February 2010 through February 2014. Pharmacists’ work—including patient demographics, disease states, and medication therapy problems—was recorded in a Microsoft Access database and tabulated.
Results: The pharmacists conducted 11,206 CMM encounters with 3,777 unique patients during the study period. The pharmacists identified 9,375 medication therapy problems (MTPs) and performed 14,092 interventions. Pharmacists most commonly worked with patients with diabetes, hypertension, pain, and hyperlipidemia. Physician and patient acceptance of the pharmacists’ work was high.
Conclusions: Pharmacists working in family medicine offices contribute to patient care through identification and resolution of MTPs and also by collaborating with PCMH teams.
Pharmacists’ inclusion on patient-centered medical home (PCMH) teams has been shown to improve patient care outcomes in several small-scale studies but has yet to be widely implemented in practice.1,2 Pharmacists practicing in a PCMH provide comprehensive medication management (CMM), defined as the standard of care that ensures each patient’s medications are assessed for appropriateness, effectiveness, safety, and adherence given specific factors like demographics, comorbidities, and other medications.3,4 Working collaboratively with other health care providers, CMM enables a pharmacist to optimize medications for patients in a safe and cost-effective way. Elements of CMM enhance care coordination and decrease cost compared to traditional primary care practice.5-10 Additionally, pharmacist-provided patient care leading to therapeutic and safety outcomes is well described and when compared to standard care, improves HbA1C, blood pressure, lipid profiles, and reduces adverse drug events.5,6,11 Furthermore, PCMH team members recognize pharmacists’ value through evidence-based practice, patient interviewing skills, and drug information knowledge while forming professional, collaborative relationships.12-14
An interprofessional team utilizing the unique skill sets of each member is the hallmark of the PCMH and is critical to achieving positive patient outcomes.15,16 The PCMH model expands patients’ access to primary care, improves chronic disease state outcomes, and increases rates of screening for certain health problems.17-19 PCMHs have also been shown to decrease overall health care costs and reduce patient utilization of acute care services.17,18,20 One study found PCMHs decreased emergency department utilization by 23% and decreased medication related costs by 11%.21
Results from longitudinal, sustained pharmacist contribution to patient care within a PCMH are lacking. While the benefits of pharmacist integration into the PCMH model have been well documented, few studies report the longitudinal work of pharmacists that achieved the reported outcomes. Such information is critical to the development of a sustainable, replicable, and scalable model of embedded pharmacists in PCMHs.7,22 Understanding the work and types of interventions pharmacists make in primary care can allow medical directors, health plans, and policy makers to seek their addition to PCMHs. We describe the work of two pharmacists integrated into four nonacademic family medicine practices dedicated to the medical home over a 4-year period.
The objective of this study was to describe the work of pharmacists practicing as integrated members of PCMHs through retrospective analysis of their patient care documentation over a 4-year time frame. We specifically aimed to describe (1) the pharmacists’ volume of patients and encounters, (2) the volume and types of work performed by the pharmacists overall and for the most common disease states, and (3) the volume and types of activities the pharmacists performed to ensure continuity of care for patients.
Practice Setting
The SCRIPT (Successful Collaborative Relationships to Improve PatienT care) project began in 2009 as a partnership between University of Pittsburgh Medical Center (UPMC) St Margaret, UPMC Health Plan, and the University of Pittsburgh School of Pharmacy. The primary goal of SCRIPT was to understand the impact of pharmacists providing patient care as integral members of the PCMH.23 Two pharmacists with experience in providing direct patient care were integrated into four nonacademic, suburban UPMC family physician offices in the greater Pittsburgh area. Each pharmacist divided their time between two practices. The pharmacists joined interprofessional patient care teams comprised of physicians, medical assistants, nurses, nurse practitioners, and office managers. These teams care for approximately 37,000 patients between the four practice sites. Twenty-one physicians average 30 patient visits per day. Additional details of these practice sites have been previously reported.23
While each pharmacist’s time was divided between two practices, patient care and team coordination was not dependent on the pharmacist’s location. Pharmacists routinely responded to patient and PCMH team inquiries through the electronic health record (EHR) and phone conversations, even while not at their physical location. Pharmacists primarily rotated between the practices as a means to see patients face-to-face. Approximately 25% of the pharmacists’ time was spent providing face-to-face services. Phone outreach and follow-up accounted for 20% of the time.23 Consultation with the prescribers and PCMH staff accounted for 15% of the time. The remaining 40% of time was a combination of population health (writing of policies and clinical protocols), chart review to identify patient needs, and documentation.23
Pharmacist Workflow
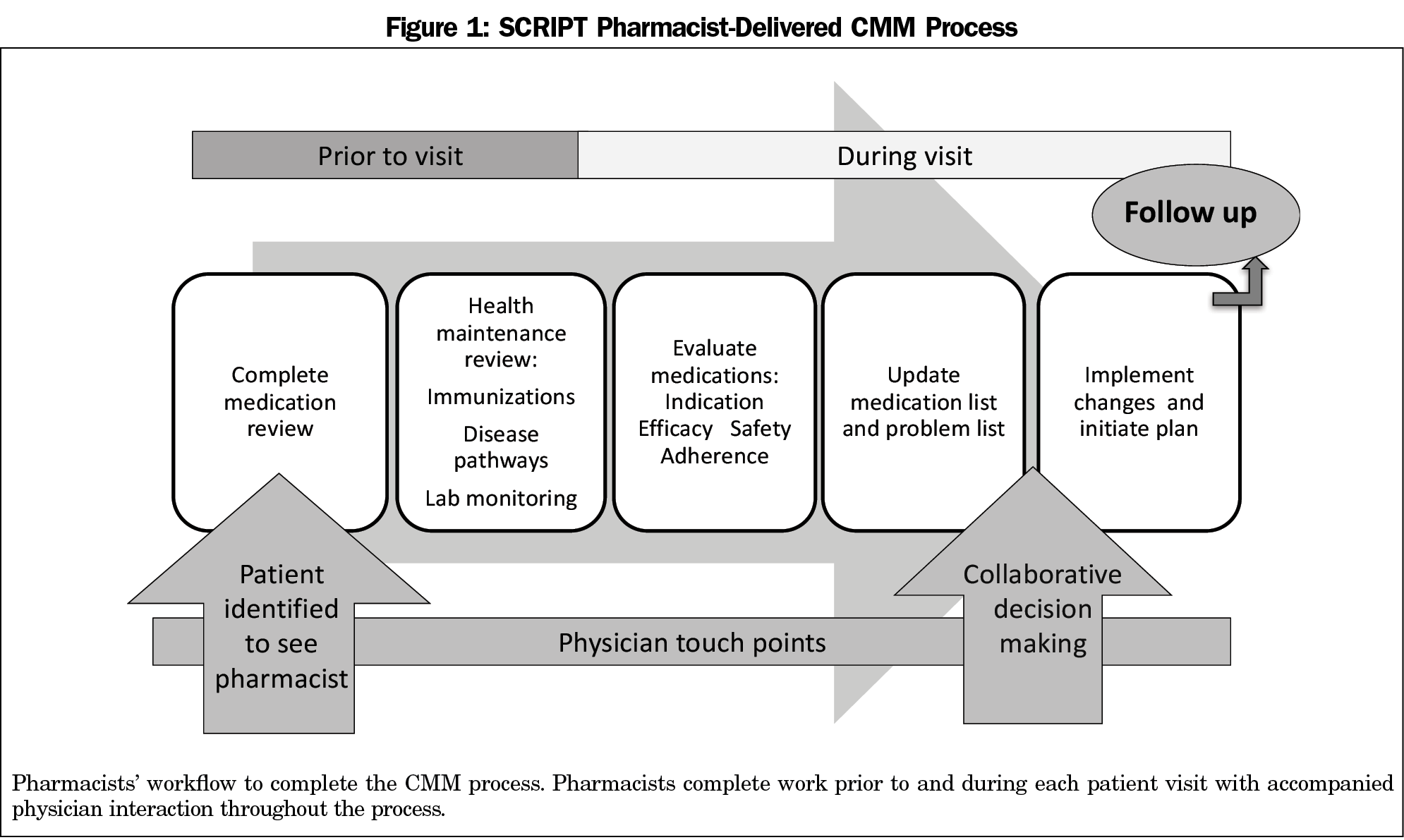
The SCRIPT pharmacists collaborated with prescribers and staff to deliver coordinated, comprehensive patient care. Figure 1 depicts the pharmacist workflow. Patients requiring CMM were identified through a variety of mechanisms including pharmacists’ review of daily schedules, physician referral, staff referral, patient self-referral, health-system generated reports including hospital/emergency room discharges, or payer-generated reports. Eligibility for pharmacist involvement with the patient was purposely open-ended so pharmacists could assess and respond to the needs of their patients and practice while the study investigators could uncover where their care was most needed. Prior to patient contact, each pharmacist reviewed the individual patient’s medications and required health maintenance activities to create a framework for the encounter.
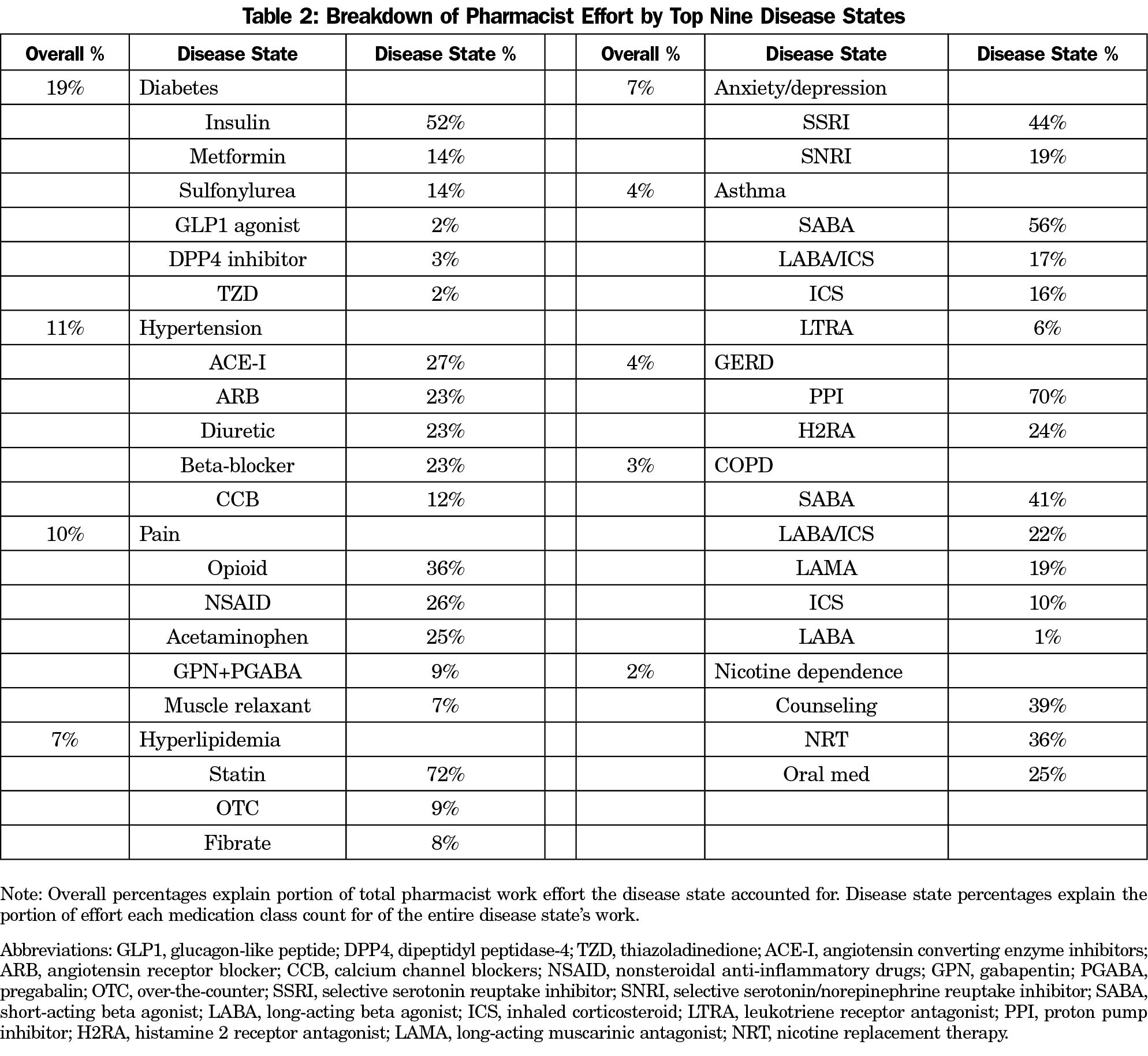
The pharmacists provided patient care through various means, most frequently beginning with a face-to-face visit, followed by telephone or face-to-face follow-up, and electronic messaging with physicians in anticipation of their visits with the patient. Patients can have scheduled appointments with the pharmacist or see the pharmacist before, during, or after their appointment with a physician. This flexibility is intentional to optimize office workflow and minimize patient wait times. During encounters, pharmacists provided CMM, which includes detailed medication evaluation to identify, prevent, and solve medication therapy problems (MTPs). Table 1 outlines the components of CMM.3,4 Pharmacists reviewed each medication individually to ensure therapy is safe, indicated, and optimized to achieve clinical and patient goals. The pharmacist then engages in collaborative decision making with the physician and patient to resolve any MTPs.
After an encounter is completed, the pharmacists document in the patient’s EHR. These notes outline the visit and include a medication review, MTPs identified, and interventions discussed with the physician, nurse, and patient. The pharmacists also document in an internally developed database. This Microsoft Access database was developed to collect discrete data related to the pharmacists’ work that the practices’ EHR could not yet capture. In this database, a profile with demographics, medications, and medical problem list is maintained for each patient. For each patient encounter, the pharmacists documented the MTP(s) identified, the medication(s) associated with the MTP(s), and interventions performed to resolve the MTP(s).
Data Collection and Statistical Analysis
This study was a retrospective, descriptive analysis of pharmacist-documented MTPs and interventions from patient encounters occurring at the four family medicine SCRIPT practices from February 2010 through February 2014. Data extracted from the internally developed database included patient demographics, medications, health conditions, MTPs identified by the pharmacists, interventions performed by the pharmacists, and continuity of care activities documented by the pharmacists.
All MTPs in the data set were first categorized into one of the seven recognized MTP categories including: (1) nonadherence, (2) adverse effect, (3) dose too low, (4) dose too high, (5) needs additional drug therapy, (6) unnecessary drug therapy, and (7) needs different drug therapy.4,24 The volume of each MTP and associated interventions was tabulated for the entire data set. Disease states associated with each encounter were also extrapolated from the Microsoft Access database.
All data were analyzed using descriptive statistics. Analyses were carried out using Stata (Version 13.1; StataCorp LP, College Station,
Texas). This study was approved by the University of Pittsburgh Institutional Review Board.
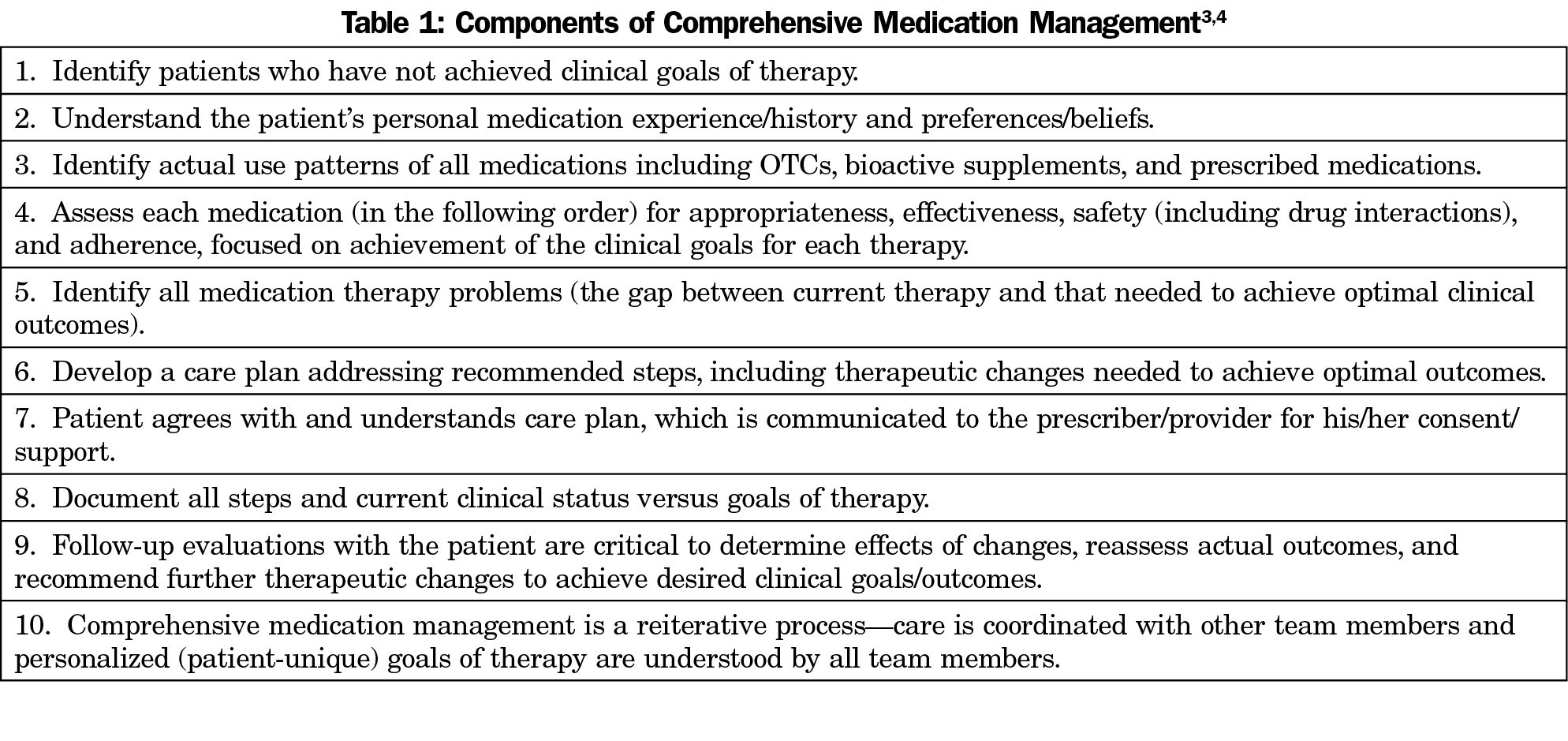
A total of 3,777 patients received care from pharmacists between February 2010 through February 2014. The mean age of these patients was 57.3 years +/-19.6 SD. Approximately 61% were female. Patient encounters totaled 11,206 over the 4-year span and included 9,375 total MTPs. The medications and conditions most frequently encountered by the pharmacists are listed in Table 2. The top nine disease states accounted for 67% of the pharmacists’ efforts. These conditions included diabetes (19%), hypertension (11%), pain (10%), hyperlipidemia (7%), anxiety/depression (7%), asthma (4%), GERD (4%), COPD (3%) and nicotine dependence (2%).
Identification of MTPs
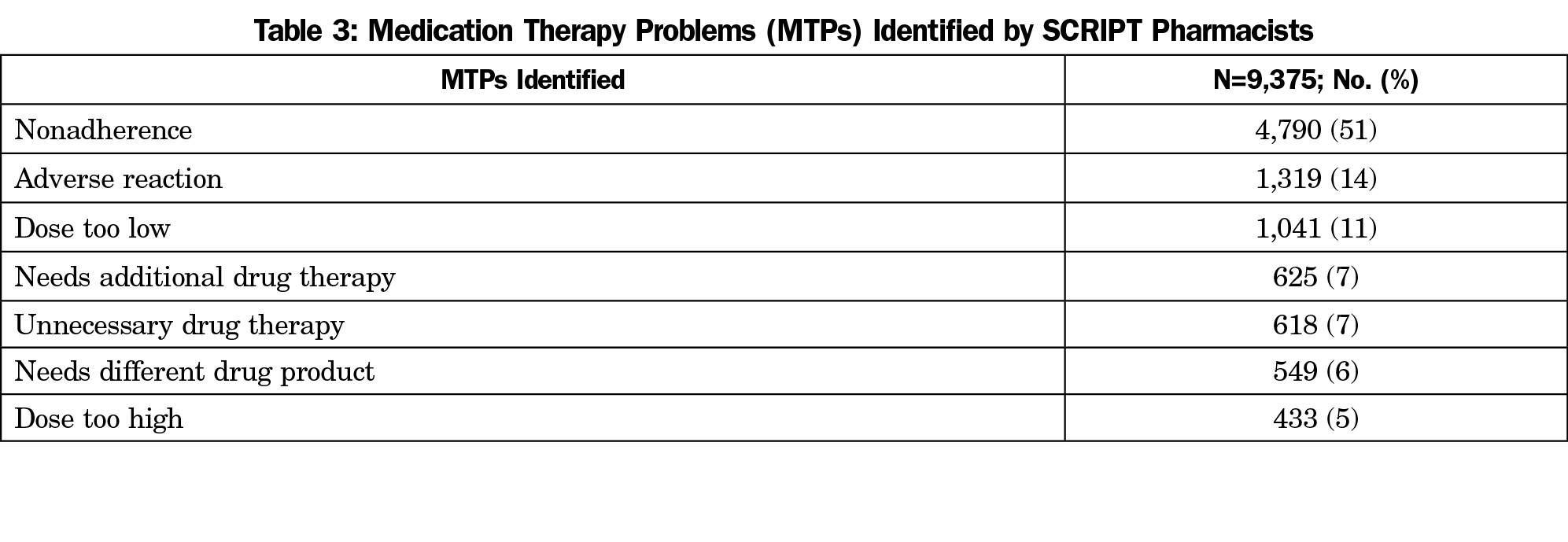
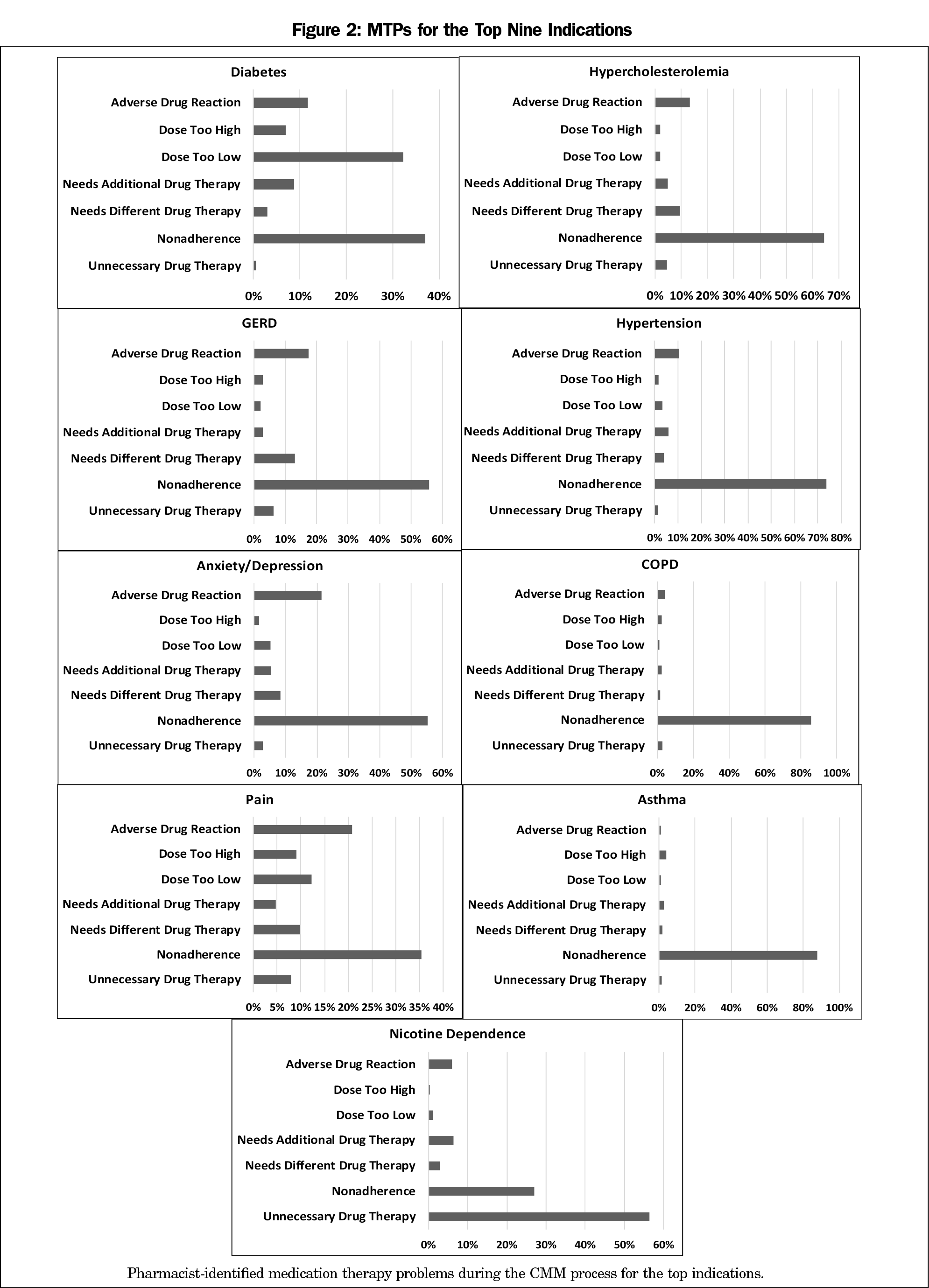
Table 3 summarizes the quantities and frequencies of MTPs for the entire data set. Nonadherence was the most common MTP identified for the entire data set (51%). Common reasons for nonadherence documented by the pharmacists were cost, misunderstood directions, patient preference not to take medication, forgetfulness, unable to administer the medication, and product unavailability or expiration. The second most common MTPs identified for top nine disease states varied. These included dose too low for diabetes; adverse drug reactions for hypertension, hypercholesterolemia, anxiety/depression, pain, COPD and GERD, and dose too high for asthma. Figure 2 shows a breakdown of the MTPs per top indication. For diabetes, the most common disease state, the most frequent MTPs identified were nonadherence, dose too low, adverse drug reaction, and needs additional therapy.
Resolution of MTPs
Through CMM encounters, pharmacists resolved MTPs by several means and recorded 14,092 interventions. The pharmacists performed an average of 1.5 interventions per MTP identified, indicating that it sometimes took more than one step to resolve a problem. Education was the most frequent intervention, accounting for 57% of all interventions. Pharmacists provided education on medications, lifestyle changes, and devices including glucometers, insulin pens, and inhalers. Pharmacists adjusted medication regimens to account for 23% of all interventions. Reasons for medication changes included optimization of medication therapy or for formulary reasons.
Pharmacists provided various interventions for the top indications. After education, the second most common interventions varied for the top nine indications. These included changes in medication regimen for hypertension, hyperlipidemia, and asthma, and addition of a medication for nicotine dependence. The most frequent interventions made for patients with diabetes included providing patient education, addressing adherence, titration of medications, and assessing for optimized medication regimens.
Pharmacist interventions were accepted at a high rate by both physicians and patients. Physicians accepted 98% and patients accepted 90% of all interventions.
Continuity of Care
Continuity of patient care is an important aspect of the pharmacists’ impact. This includes coordination of care and medication therapy monitoring. Medication lists were updated a total of 4,700 times for an average of 1.2 times per patient. Physician interaction occurred 7,145 times and included face-to-face communication for the majority of first encounters. No MTPs were identified for 4,653 encounters (41%) provided by SCRIPT pharmacists.
The results of our study describe the work of pharmacists integrated as members of patient care teams within PCMHs. The longitudinal work provided by the pharmacists was comprehensive, including 149 different disease states during 11,206 encounters. The pharmacists provided comprehensive medication management (CMM) across multiple practice sites in the same geographic area. Our pharmacists were embedded as integral members of the care teams in each PCMH working very closely with physicians, who accepted their interventions 98% of the time. Conversely, a study of contracted pharmacists working outside of the patient care team yielded a lower rate of acceptance.10 Our acceptance rates mirror a previous study of PCMH pharmacists, but those pharmacists focused their effort on only one chronic condition.25 Additionally, our results are sustained over a longitudinal, 4-year period; previous studies have been less than 1 year.10,25
The pharmacists cared for patients of all ages, highlighting the potential for full-spectrum family practices. However, the patient panel cared for by the pharmacists predominantly included middle-aged or older adults. These patients represent a segment that have an increased medication burden, suggesting pharmacists may be best employed to care for older adults. In our study, diabetes was the most encountered chronic condition and required the most effort of the pharmacists. Diabetes requires multiple medications to effectively treat the condition, with extensive monitoring and therapeutic adjustments aligning it very closely with the pharmacists’ skill sets. The other top indications also require multiple medications, making it unsurprising this is where the pharmacists were most utilized. The breadth of disease states (149) also implies that importance of a generalist mindset on the part of the pharmacist is a critical aspect of the care provided.
Medication therapy problems (MTPs) were identified and resolved by our pharmacists during patient care encounters. Nonadherence was the most commonly identified MTP. Nonadherence to medication regimens accounts for up to $289 billion in US health care costs annually, and can lead to death and hospitalizations.26 Pharmacists are trained to use a specialized skill set to improve adherence rates, which is unique from other members of the PCMH.27-29 Secondary MTPs that pertained to the specific indications were identified and resolved by modifying existing medications, starting new medications, or stopping medications to achieve clinical goals.
Our study was set in four medical home practices with two pharmacists. Before recording patient encounters in the Microsoft Access database and periodically during the study period, the pharmacists met to ensure data would be entered correctly. However, each pharmacist may have made assumptions on how to best categorize the data entry into the database. Additionally, pharmacists were required to document their work in multiple places including the study database, a health system database, and in the EHR. This likely led to underreporting of work due to misplaced documentation and lack of time. Lastly, the build and functionality of the Microsoft Access database also impacted report generation. Embedding software that allows pharmacists to document and tally their interventions directly into the EHR can improve future studies.
Our results are reported at a time of advancement of the PCMH and pharmacists’ roles in patient care. Quality metrics continue to be established, with the bar being raised higher every year.30-32 These require a team-based approach, utilizing the unique skill sets of various health care team members. There is also a national effort to deploy an integrated documentation system called the Pharmacist eCare Plan, which allows pharmacists to consistently document their patient care and securely message partnering physicians and prescribers through their EHR for further continuity of care.33 This documentation will aid in a standardized process for pharmacists to document CMM work.
While numerous examples outline the impact pharmacists can have on targeted disease states and cost reduction, their incorporation in PCMH teams is not widely implemented.11, 34-40 Our previous study outlines successful implementation of the pharmacist in the PCMH,23 and this study provides the long-term impact through a descriptive analysis. The pharmacist integration into the PCMH provides a complementary skill to effectively identify, prevent, and solve MTPs. Medications account for 80% of treatment plans, and thus are critical to effectiveness and quality of patient care.4 Overall, our study is directly applicable to family medicine practices as pharmacists’ contributions to patient care are sustained over time, encouraging the development of trust between team members and with their patients. Family physicians and pharmacists should work collaboratively with directors, health plans, and policy makers to develop sustainable models for routine inclusion of this team member in PCMHs.
Our study shows sustained results to support pharmacist involvement in primary care practices by utilizing CMM. Pharmacists’ unique knowledge and skill set allows for identification, prevention, and solving of MTPs to support quality patient care within a PCMH team. Further expansion of pharmacists in PCMH teams is warranted.
Acknowledgments
AcknowleDgments: The authors acknowledge Eric Foley for his development of the Microsoft Access database and data retrieval.
Presentations:
1. Castelli G. Successful Collaborative Relationships to Improve PatienT care (SCRIPT): evaluation of pharmacists’ interventions in family medicine offices [Poster]. Society of Teachers of Family Medicine Annual Spring Conference. San Antonio, TX. May 4, 2014.
2. Castelli G. The SCRIPT Project: evaluation of clinical pharmacist work in non-academic family medicine practices [Poster]. North American Primary Care Research Group. Colorado Springs, CO. November 14, 2016.
References
- Choe HM, Farris KB, Stevenson JG, et al. Patient-centered medical home: developing, expanding, and sustaining a role for pharmacists. Am J Health Syst Pharm. 2012;69(12):1063-1071. https://doi.org/10.2146/ajhp110470
- Smith M, Bates DW, Bodenheimer T, Cleary PD. Why pharmacists belong in the medical home. Health Aff (Millwood). 2010;29(5):906-913. https://doi.org/10.1377/hlthaff.2010.0209
- Patient-Centered Primary Care Collaborative (PCPCC). The Patient-Centered Medical Home: Integrating Comprehensive Medication Management to Optimize Patient Outcomes Resource Guide, 2nd ed. Washington, DC: PCPCC, 2012. Available from www.pcpcc.org/sites/default/files/media/medmanagement.pdf. Accessed May 1, 2018.
- American College of Clinical Pharmacy. Comprehensive Medication Management in Team-Based Care. 2017. Available from https://www.accp.com/docs/positions/misc/CMM%20Brief.pdf. Accessed November 3, 2017.
- Nkansah N, Mostovetsky O, Yu C, et al. Effect of outpatient pharmacists’ non-dispensing roles on patient outcomes and prescribing patterns. Cochrane Database Syst Rev. 2010;(7):CD000336.
- Giberson S, Yoder S, Lee MP. Improving patient and health system outcomes through advanced pharmacy Practice. A report to the U.S. Surgeon General. Office of the Chief Pharmacist. U.S. Public Health Service. December 2011.
- Nigro SC, Garwood CL, Berlie H, et al. Clinical pharmacists as key members of the patient-centered medical home: an opinion statement of the Ambulatory Care Practice and Research Network of the American College of Clinical Pharmacy. Pharmacotherapy. 2014;34(1):96-108. https://doi.org/10.1002/phar.1357
- Isetts BJ, Schondelmeyer SW, Artz MB, et al. Clinical and economic outcomes of medication therapy management services: the Minnesota experience. J Am Pharm Assoc (2003). 2008 Mar-Apr;48(2):203-11; 3 p following 211.
- Romanelli RJ, Leahy A, Jukes T, Ishisaka DY. Pharmacist-led medication management program within a patient-centered medical home. Am J Health Syst Pharm. 2015;72(6):453-459. https://doi.org/10.2146/ajhp140487
- Smith M, Giuliano MR, Starkowski MP. In Connecticut: improving patient medication management in primary care. Health Aff (Millwood). 2011;30(4):646-654. https://doi.org/10.1377/hlthaff.2011.0002
- Chisholm-Burns MA, Kim Lee J, Spivey CA, et al. US pharmacists’ effect as team members on patient care: systematic review and meta-analyses. Med Care. 2010;48(10):923-933. https://doi.org/10.1097/MLR.0b013e3181e57962
- Snyder ME, Zillich AJ, Primack BA, et al. Exploring successful community pharmacist-physician collaborative working relationships using mixed methods. Res Social Adm Pharm. 2010;6(4):307-323. https://doi.org/10.1016/j.sapharm.2009.11.008
- McDonough RP, Doucette RP. Dynamics of Pharmaceutical Care. J Am Pharm Assoc. 2001;41(5):682-692. https://doi.org/10.1016/S1086-5802(16)31315-8
- Maracle HL, Oliveira DR, Brummel A. Primary care providers’ experiences with pharmaceutical care-based medication therapy management services. Innov Pharm. 2012;1(72):1-12.
- Doherty RB, Crowley RA; Health and Public Policy Committee of the American College of Physicians. Principles supporting dynamic clinical care teams: an American College of Physicians position paper. Ann Intern Med. 2013;159(9):620-626. https://doi.org/10.7326/0003-4819-159-9-201311050-00710
- Pub L No. 1111-148, 124 Stat 119. The Patient Protection and Affordable Care Act (2010).
- Nielson M, Langner B, Zema C, Hacker T, Grundy P. Benefits of implementing the primary care patient centered medical home: review of cost and quality results 2012. Patient-Centered Primary Care Collaborative. Sept 2012.
- Nielson M, Gibson A, Buelt L, Grundy P, Grumbach K. The patient-centered medical home’s impact on cost and quality. Patient-Centered Primary Care Collaborative. Jan 2015.
- Phillips RL Jr, Bronnikov S, Petterson S, et al. Case study of a primary care-based accountable care system approach to medical home transformation. J Ambul Care Manage. 2011;34(1):67-77. https://doi.org/10.1097/JAC.0b013e3181ffc342
- Friedberg MW, Rosenthal MB, Werner RM, Volpp KG, Schneider EC. Effects of a Medical Home and Shared Savings Intervention on Quality and Utilization of Care. JAMA Intern Med. 2015;175(8):1362-1368. https://doi.org/10.1001/jamainternmed.2015.2047
- Steiner BD, Denham AC, Ashkin E, Newton WP, Wroth T, Dobson LA Jr. Community care of North Carolina: improving care through community health networks. Ann Fam Med. 2008;6(4):361-367. https://doi.org/10.1370/afm.866
- Isetts BJ. Pharmaceutical care, MTM, & payment: the past, present, & future. Ann Pharmacother. 2012;46(4):S47-S56. https://doi.org/10.1345/aph.1Q806
- Kozminski M, Busby R, McGivney MS, Klatt PM, Hackett SR, Merenstein JH. Pharmacist integration into the medical home: qualitative analysis. J Am Pharm Assoc (2003). 2011 Mar-Apr;51(2):173-83.
- Strand LM, Morley PC, Cipolle RJ, Ramsey R, Lamsam GD. Drug-related problems: their structure and function. DICP. 1990;24(11):1093-1097. https://doi.org/10.1177/106002809002401114
- Carter BL, Ardery G, Dawson JD, et al. Physician and pharmacist collaboration to improve blood pressure control. Arch Intern Med. 2009;169(21):1996-2002. https://doi.org/10.1001/archinternmed.2009.358
- Viswanathan M, Golin CE, Jones CD, et al. Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann Intern Med. 2012;157(11):785-795. https://doi.org/10.7326/0003-4819-157-11-201212040-00538
- Bosworth HB, Granger BB, Mendys P, et al. Medication adherence: a call for action. Am Heart J. 2011;162(3):412-424. https://doi.org/10.1016/j.ahj.2011.06.007
- Desborough JA, Sach T, Bhattacharya D, Holland RC, Wright DJ. A cost-consequences analysis of an adherence focused pharmacist-led medication review service. Int J Pharm Pract. 2012;20(1):41-49. https://doi.org/10.1111/j.2042-7174.2011.00161.x
- Carter BL, Foppe van Mil JW. Comparative effectiveness research: evaluating pharmacist interventions and strategies to improve medication adherence. Am J Hypertens. 2010;23(9):949-955. https://doi.org/10.1038/ajh.2010.136
- National Committee for Quality Assurance. HEDIS 2016. 2015. Available at: http://www.ncqa.org/hedis-quality-measurement/hedis-measures/hedis-2016. Accessed March 8, 2018.
- Centers for Medicare and Medicaid Services. Medicare Access and CHIP Reauthorization Act (MACRA). Available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html. Accessed May 11, 2018.
- Pharmacy Quality Alliance. PQA measures used by CMS in the Star Ratings.http://pqaalliance.org/measures/cms.asp. Accessed May 7, 2018.
- National Council for Prescription Drug Programs. Pharmacist eCare Plan. Guidance on the Use of the HL7 CDA Consolidated templates for Clinical Notes R2.1 Care Plan. Available at https://www.ncpdp.org/NCPDP/media/pdf/Pharmacist-eCare-Plan.pdf. Accessed May 1, 2018.
- Chisholm-Burns MA, Graff Zivin JS, Lee JK, et al. Economic effects of pharmacists on health outcomes in the United States: A systematic review. Am J Health Syst Pharm. 2010;67(19):1624-1634. https://doi.org/10.2146/ajhp100077
- Kislan MM, Bernstein AT, Fearrington LR, Ives TJ. Advanced Practice Pharmacists: a retrospective evaluation of the efficacy and cost of ClinicaL Pharmacist PractitionErs managing ambulatory Medicare patients in North Carolina (APPLE-NC). BMC Health Serv Res. 2016;16(1):607. https://doi.org/10.1186/s12913-016-1851-2
- Tan ECK, Stewart K. Elliott RA, George J. Pharmacist services provided in general practice clinics: a systematic review and meta-analysis. Res Soc Adm Pharm. 2014;10(4):608e622.
- Santschi V, Rodondi N, Bugnon O, Burnier M. Impact of electronic monitoring of drug adherence on blood pressure control in primary care: a cluster 12- month randomised controlled study. Eur J Intern Med. 2008;19:427e434.
- Houle SKD, Chatterley T, Tsuyuki RT. Multidisciplinary approaches to the management of high blood pressure. Curr Opin Cardiol. 2014;29(4):344e353. https://doi.org/10.1097/HCO.0000000000000071
- Greer N, Bolduc J, Geurkink E, et al. Pharmacist-led chronic disease management: a systematic review of effectiveness and harms compared with usual care. Ann Intern Med. 2016;165(1):30. https://doi.org/10.7326/M15-3058
- Wubben DP, Vivian EM. Effects of pharmacist outpatient interventions on adults with diabetes mellitus: a systematic review. Pharmacotherapy. 2008;28(4):421e436. https://doi.org/10.1592/phco.28.4.421



There are no comments for this article.