Background and Objectives: Despite widespread patient use, herbal and dietary supplement education is not required in US-accredited medical schools. Thus, physicians are unprepared to address supplement use with patients. Our objectives were to assess perceived adequacy of medical education on supplements, determine resident perspectives on appropriate placement of curricula in their longitudinal medical education, and evaluate the effects of an innovative workshop on family medicine resident knowledge about supplements and intentions to address this topic with patients.
Methods: Family medicine residents (N=65) participated in an hour-long workshop covering basic concepts about herbal and dietary supplements, including regulations, literature review techniques, and risk/benefit analysis. The participants completed pre/postworkshop surveys to assess need for increased education and evaluate efficacy of the workshop.
Results: Most participants (91.9%) thought they should have received more education than provided on supplements and perceived greater need for curricula in undergraduate medical education than in graduate medical education. Only 47.6% received required education on supplements, significantly less than the 72.6% who thought this education should be required (P<0.05). The workshop increased the proportion of residents planning to address patients’ supplement use, increased the frequency residents intend to ask about supplements, and improved resident perceptions of the efficacy of some supplements when used with physician guidance.
Conclusions: Residents perceived a lack of adequate medical education on the use of herbal and dietary supplements. Results showed a brief workshop increased resident intentions to discuss supplement use with patients. Further education on supplement use may be warranted.
Dietary supplements, including vitamins, minerals, and herbals, are the most widely used component of complementary and alternative medicine (CAM) among US adults, surpassing chiropractic, yoga, meditation, and special diets.1,2 Over half of US adults report use of supplements with 18%-39% reporting use specifically of herbals (nonvitamin, nonmineral supplements) to self-treat a wide range of conditions.1-3 While vitamins and minerals often fall under the umbrella of nutrition—a subject required in 94% of US medical schools—herbal medicine does not.4 Given widespread patient use, medical education on supplements, with a particular focus on herbals, warrants specific attention.
By failing to discuss supplements, physicians risk prescribing medications that adversely interact with supplements, failing to recognize patient symptoms possibly attributable to supplements, and missing opportunities to use supplements beneficially.5-9 While some supplements have been shown in clinical trials to be effective, others have little evidence, pose significant risks to patients, or carry risks for drug interactions.5-9 As providers and managers of full-spectrum patient care, these discussions are of particular importance to family physicians.
The Society of Teachers of Family Medicine has endorsed residency training in CAM since 1999.10 Consequently, the proportion of family medicine residencies (FMRs) including curricula on CAM has increased from 28% in 1995 to 44% in 2013, and 89% of CAM courses include training on supplements.11-12 Despite increasing graduate medical education (GME) on supplements, the proportion of patients discussing supplements with their physician has remained low. Sixty-three percent to 72% of patients using supplements in 2008, up to 80% in 2017 report that they do not discuss them with their physician.5,6 This is surprising, as CAM curricular guidelines include the “ability to inquire into patients’ use of CAM in a nonthreatening, nonjudgmental manner,” yet these data suggest that current medical education on CAM does not improve discussions about supplements.11
The paucity of these discussions might be partly explained by deficient undergraduate medical student education (MSE) on supplements as opposed to insufficient GME on supplements. Currently, Liaison Committee on Medical Education- (LCME) accredited medical schools are not required to include any instruction on CAM.13 While a large body of literature describes the implications of and suggests solutions to limited CAM exposure in MSE, few examine the need for expanded education on supplements specifically, or incorporate evidence-based analysis of therapies.7,8,14,15 Not only do the data warrant education specifically on supplements, medical students consistently rank supplements among the top CAM therapies they would like to learn about.1,2,7
The National Academy of Medicine (formerly the Institute of Medicine) recommended as early as 2005 that health professional schools provide enough instruction on CAM to competently advise patients, though no specific guidelines were provided.16 Although GME on CAM has expanded in FMRs and improved resident knowledge in programs incorporating this training, other surveys show that only 5% of FM residents feel comfortable advising patients on CAM.10-12,17 Less improvement has been made at the MSE level, with consequent reports that medical students are not comfortable counseling patients about CAM.7,15,16 These data suggest that the US medical education system has done a poor job incorporating National Academy of Medicine recommendations.
Objectives and Hypotheses
In this study, we assessed perceived adequacy of medical education on supplements among residents at Colorado FMRs and sampled resident perspectives on appropriate placement of supplement curricula in GME vs MSE. Due to previously reported medical student and resident discomfort advising patients about CAM, we hypothesized that residents perceive MSE and GME on supplements as inadequate; however, we hypothesized that residents would identify a greater need for supplement education in MSE, given recent GME expansion of supplement education without corresponding expansions in MSE. 7,10-12,15-18 Based on principles from the theory of reasoned action (TRA), a well-established theory of human motivation and behavior, we hypothesized that both perceived faculty norms and resident attitudes would influence resident intentions and behavior.19 Finally, we evaluated perceived utility of an innovative workshop in improving resident knowledge about supplements and intentions to address supplements with patients, hypothesizing that our curriculum would improve confidence about supplements and increase the proportion of residents intending to address supplements with patients.
Design and Recruitment
This study was a pre/post, single-group design. Immediately before and after participating in a 1-hour workshop about supplements, 65 FM residents completed self-report surveys about (1) perceived need for MSE/GME on supplements, and (2) supplement use attitudes, norms, intentions, and past behavior (reflecting key constructs from the TRA). The postsurvey also included measures of perceived workshop utility. The study was approved by the Colorado Multiple Institutional Review Board with exempt status.
A total of 65 residents from six Colorado FMR programs were recruited to the study. Emails offering the experimental workshop were sent to FMR program directors and the workshop was delivered at FMRs electing to participate. FM residents in participating programs who were on clinical rotations that allotted time for didactics were required to participate in the workshop, which was incorporated into their series of regular didactic sessions. Although attendance was required, participation in the research project through completion of pre/postsurveys was voluntary. Residents were given a postcard consent form preworkshop and paper surveys pre/postworkshop. Response rate among residents attending the workshop was 100%, despite the option not to participate. Eligible participants were in a Colorado FMR program and present at the didactic session.
Educational Intervention
The workshop was designed to incorporate the core competencies outlined by the Academic Consortium for Integrative Medicine and Health that apply to supplements: potential for adverse effects, research evidence for efficacy, reputable resources for information, and current regulations.20 We engaged residents in the process of researching supplements with reputable sources in response to patient cases and provided guidance for counseling patients about safety, efficacy, and regulations. Residents worked in small groups of two to three, with one facilitator per session of eight to thirteen residents and evaluated two cases. Subsequent discussions referred back to the cases. This skill-oriented and case-based design is distinct in that it prompts participants to incorporate evidence-based medicine and critical thinking into discussions of supplements, something which only 8.2% of medical schools include in existing curricula.15 Curricular content is described in Table 1.
Measures
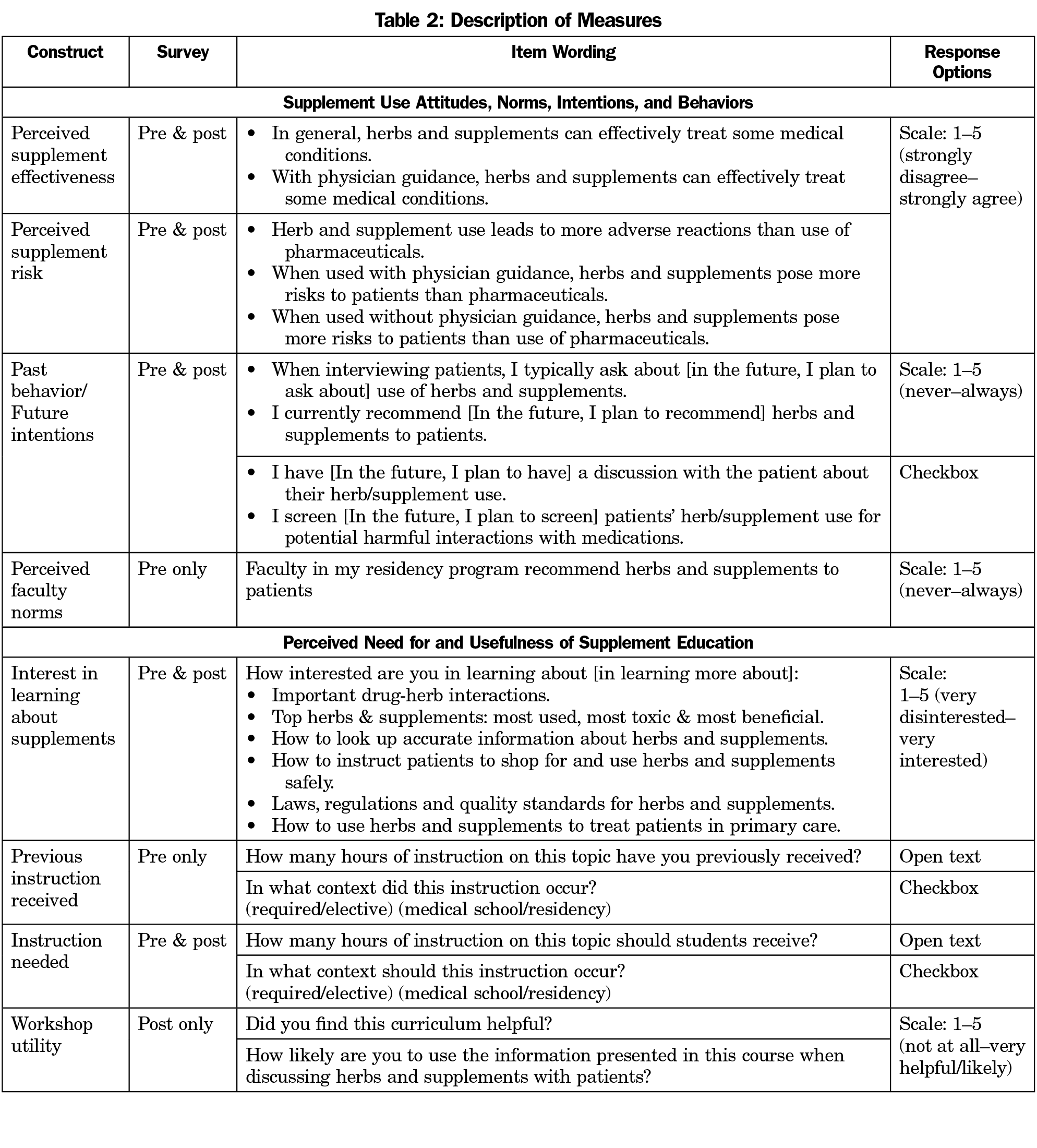
Outcomes measures are described in Table 2, selected to allow evaluation of effects of the workshop on TRA motivational constructs relevant to supplement use, and perceived need for and utility of the workshop itself. Composite variables (averages of Likert-type scale items) were created where internal consistency (Cronbach α) among items reflecting a given construct was greater than .70. Continuous scale items were otherwise analyzed individually. In the presurvey, participants reported perceived effectiveness of supplements (two items; Cronbach α=.80–pre and post) and perceived risk of supplements (three items analyzed separately, “attitudes towards supplement use”); residency faculty behaviors recommending supplements to patients (one item, “perceived norms for supplement use”); “past behavior” discussing supplements with patients (two Likert-type scale items, two checkbox items—coded “yes” if either box checked “yes”). We assessed perceived need for MSE/GME supplement education with items assessing interest in learning about supplements (six items, Cronbach α=.91 pre, .90 post), and by comparing participants’ actual amount (open text coded as 0 hours, 0 to 5 hours, 6 to 10 hours, more than 10 hours, or “other” for nonnumerical responses) and context (GME vs MSE, required vs elective) for previous supplement education, and perceived amount and context in which students should receive such education. We manually coded for each participant whether or not they felt they should have received more instruction than they actually received. In the postsurvey, participants repeated items assessing attitudes, interest, and education students should receive, and also reported future intentions to discuss supplements with patients (two items) and perceived workshop utility (two items). This was a pilot study and no relevant measures previously existed; measures were practical and had face validity for this evaluation.
Analysis
We used descriptive statistics to assess participants’ attitudes toward supplements, intentions to address supplements with patients, perceived need for MSE and GME on supplements, and perceptions of workshop utility. We used McNemar’s test to evaluate differences in proportions and dependent samples t-test and Fisher’s exact test to examine changes in attitudes and intentions pre/postworkshop. Analyses were conducted using SAS Version 9.4.
Sample Characteristics
The sample included 65 FM residents with a mean of 1.75 years in residency. This consisted of 34% of the population of Colorado FM residents (8-13 residents from each of the 6 participating programs). Demographic data (eg, age, gender, race/ethnicity) on participants were not collected.
Although 100% of didactic session participants filled out surveys, 6.2% were filled out incompletely and 4.6% filled out only one survey (pre or post) due to arriving late or leaving early. Missing data were handled via listwise deletion.
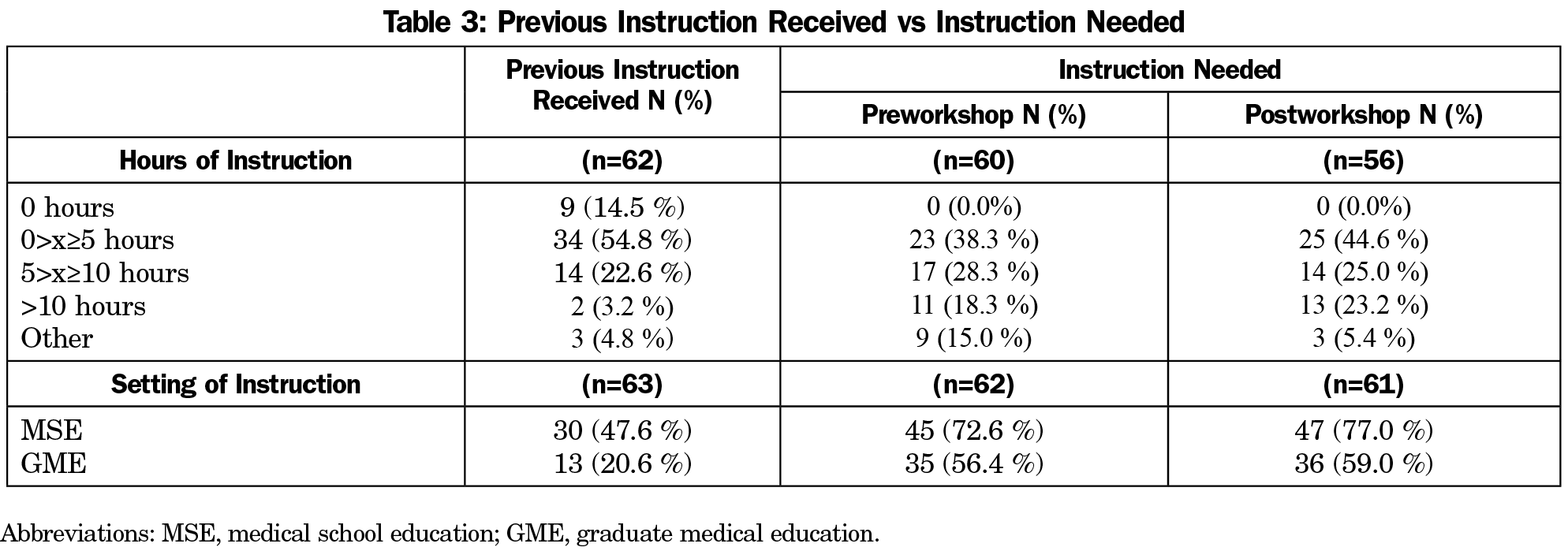
Perceived Need for Supplement Education
Comparing individual resident hours and setting of instruction received vs needed, 57 out of 62 residents (91.9%) responded that they should have received more education. On the presurvey, residents reported having received significantly less education on supplements than they believe they should have received (Table 3). At the MSE level, 47.6% of respondents received required classes on supplements, whereas 72.6% of respondents said students should have received required classes (McNemar test: P=.0002). At the GME level, 20.6% of respondents received required classes, whereas 56.4% of respondents said residents should receive required classes (McNemar test: P<.0001). A greater proportion of residents believe this instruction should be received at the MSE level than at the GME level, both preworkshop (72.6% MSE, 56.4% GME, McNemar test: P=.03) and postworkshop (77.0% MSE, 59.0% GME, McNemar test: P=.02).
Relationships Among Perceived Norms, Attitudes, Past Behavior, and Intentions
On the presurvey, residents whose faculty recommend supplements (perceived faculty norms) were more likely to report that they themselves recommend supplements to patients (past resident behavior; r=0.48, P<0.0001); preworkshop attitudes (perceived effectiveness and risk) were not associated with past resident behavior (Ps=ns). Conversely, postworkshop, resident intentions to recommend supplements in the future were not associated with faculty norms reported preworkshop (r=.07, P=ns), but were positively associated with postworkshop perceived effectiveness (r=.54, P<.001), and negatively associated with postworkshop perceived risk of adverse reactions relative to pharmaceuticals (r=-.31, P=.01) and risk relative to pharmaceuticals when used with physician guidance (r=-.32, P=.01).
Changes in Attitudes and Intentions to Address Supplements Following Workshop
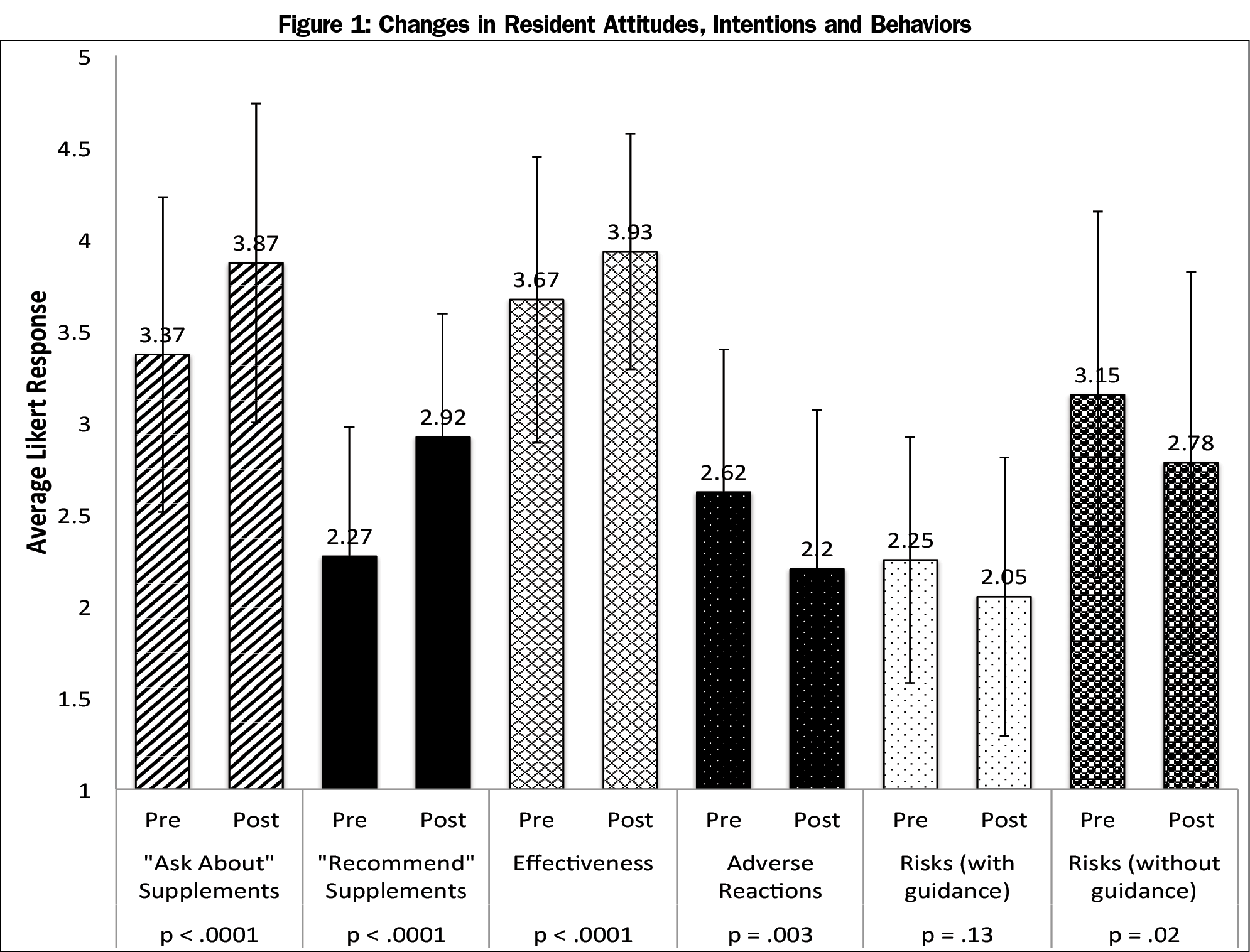
Preworkshop, 33 out of 65 respondents (50.8%) indicated they would address supplements during clinical encounters (Figure 1). Postworkshop, 55 out of 65 (84.6% of respondents) indicated they intended to address supplements during future clinical encounters (pre/post difference: P=.006, Fisher exact test, two-sided).
A dependent samples t-test showed that, postworkshop, respondents intended to ask patients about supplements more frequently (Mchange=0.52, SDchange=0.77, 95% CI: 0.32, 0.72, t(59)=5.20, P<.0001). Similarly, respondents planned to recommend some supplements more frequently postworkshop (Mchange=0.67, SDchange=0.77, 95% CI: 0.47, 0.87, t(59)=6.67, P<.0001).
A dependent samples t-test showed respondents exhibited increased perceptions of effectiveness of some supplements pre/postworkshop (Mchange=0.26, SDchange=0.46, 95% CI: 0.14, 0.38, t(60)=4.38, P< 0.0001). Similarly, respondents showed lower perceptions of risks of supplements pre/postworkshop, including beliefs that supplements have adverse reactions (Mchange=-0.43, SDchange=1.07, 95% CI: -0.70, -0.15, t(60)=-3.11, P=0.003), beliefs that supplements pose more risks than pharmaceuticals, both with physician guidance (Mchange=-0.20, SDchange=1.00, 95% CI: -0.45, 0.06, t(60)=-1.54, P=0.13) and without physician guidance (Mchange=-0.37, SDchange=1.18, 95% CI: -0.67, -0.06, t(60)=-2.41, P=0.02).
Workshop Utility
Overall, participants indicated that they were likely to use the information presented and that they found the workshop helpful. Mean response to how helpful residents found the workshop was 4.41 (SD=0.69), and mean response to how likely residents were to use the information presented was 4.38 (SD=0.58).
Results supported our hypotheses that FM residents perceive past MSE and GME as inadequate and that our curriculum improves their attitudes about supplements and increases the proportion of residents intending to address supplements with patients. Furthermore, results indicate that a larger proportion of residents perceive a need for expanded supplement education in MSE than in GME, although a majority believe supplement education should be expanded at both levels.
Almost all residents believed they should have received more education on supplements than provided in medical school. Inadequacy of current MSE was further supported by the significantly smaller proportion of residents who received required instruction on supplements in medical school than the proportion believing this instruction should be required. Although this same trend was observed at the GME level, this discordance could be explained by residents’ only partial completion of residency training at the time that their opinions were sampled.
These findings are not surprising given the paucity of current MSE on supplements. Although 50.8% of medical schools offer courses in CAM, only 69.9% of these courses include information on supplements, providing a median of 2 hours of instruction on this topic during an average 20-hour course.15 A majority of these courses are offered electively, with only 29% provided in a required setting.15 Thus, 35.5% of US medical schools (69.9% of 50.8%) provide a median of 2 hours of coursework on supplements and only 10.3% of schools (29% of 35.5%) provide this education in a required setting.15 Regarding GME, evaluation of the Integrative Medicine in Residency (IMR) online course shows that only 8.6% of content hours are devoted to supplements (16/186 total hours).18
In accordance with predictions from the TRA, findings in this study illustrated that perceived faculty norms and resident attitudes influence residents’ intended behavior. Prior to the workshop, resident behavior was correlated with perceived faculty norms. Following the workshop, resident intended behavior was correlated with attitudes about supplements, and was no longer correlated with the perceived faculty norms reported preworkshop. Lack of correlation between preworkshop attitudes and resident behavior was surprising and might be attributable to insufficient prior instruction on supplements to adequately inform attitudes, such that residents emulated faculty behaviors without a deeper understanding of the reasons for those behaviors. Postworkshop, however, resident attitudes about supplements correlated strongly with intended behavior, supporting our hypothesis that changing resident attitudes can evoke corresponding changes in intended behavior.
Our results further supported our hypotheses that our workshop improves resident attitudes about supplements and increases the proportion of residents intending to address this topic with patients. These results align with prior studies that observed associations between increased CAM education, improved attitudes towards CAM therapies, and intentions to apply the curricular content taught to medical practice.10,26,27
Similar to the postsurvey administered in this study, the more extensive IMR course used an exit survey to sample FM residents’ intent to utilize content learned.10 Ratings on a 5-point scale after the IMR course (4.2) were nearly identical to postworkshop ratings (4.38) in our study with respect to intent to apply content learned/address supplements with patients.10 The high ratings for our workshop were also comparable to high ratings of dietary supplement curricula at the MSE level. Following a month-long, fourth-year elective course at Pennsylvania State University College of Medicine, students highly rated their preparedness to discuss supplements postcourse while participants in our workshop demonstrated increased intent to address supplements with patients pre/postworkshop.7
Although pre/post ratings between our workshop and these courses were comparable, both the IMR and the fourth-year elective differed substantially from our workshop with respect to duration. Completion time for the IMR course was 186 total hours (16 hours on supplements) vs 4 weeks for the fourth-year elective vs 1 hour for our workshop.7,18 These differences in course duration may offer an opportunity for programs to improve participants’ competence discussing supplements with patients without adding substantial course time to medical students’ and residents’ already packed schedules. This answers concerns expressed at both the MSE and GME level that one of the top barriers to integrating CAM content into the curriculum is finding time for it.12,20
Limitations
This study was limited by lack of a comparison group due to pre/post single-group design. It is not clear that the changes in attitudes or intentions were attributable to the educational content itself. Simply having contact with an educator perceived to support CAM may have influenced participants, particularly since faculty influence was noted to affect attitudes. Results are limited by self-report surveys, which may have been subject to demand characteristics, such that participants may have responded as they believed the investigator wanted them to respond. The sample was limited by size, selection bias, and the geographical boundaries of Colorado. Although Colorado residents come from schools across the country, they may share characteristics attracting them to Colorado, making findings potentially less applicable to programs in other states. Additionally, the sample consisted of only 34% of Colorado FM residents and demographic data were not collected to evaluate how well this sample represents the population.
Next Steps
Further research could evaluate the efficacy of this workshop when incorporated into required MSE, since a larger proportion of residents identified a need for increased supplement education in MSE than in GME. The workshop could also be expanded and evaluated in FMR programs in other states and in residency programs in other specialties.
Results suggest FM residents perceive a lack of adequate curricula on dietary supplements, believe curricula is most needed at the MSE level, and exhibit increased intentions to discuss supplements with patients following our workshop. Enhancing curricula to include content on supplements, such as engaging patients in shared decision making around supplement use, may be warranted. Further work is needed to examine the extent to which additional education, beyond this brief workshop, has an effect on physician knowledge and behavior, and patient-centered outcomes.
Acknowledgments
The authors thank Monika Nuffer, PharmD, for her assistance with the educational content of the workshop, the International Congress on Integrative Medicine and Health, for providing financial support to attend their conference, and the Medical Student Council at the University of Colorado School of Medicine, for providing financial support for conference attendance.
Financial support for this project was provided by the Department of Family Medicine, University of Colorado School of Medicine.
Presentations: Conference on Meditation hosted by the Cuban Society of Neurosciences and the OM Meditation Association, April 6-9, 2017, Havana, Cuba.
Society of Teachers of Family Medicine Conference on Medical Student Education, February 9-12, 2017, Anaheim, CA.
Society of General Internal Medicine Mountain West Regional Conference, October 7, 2016, Phoenix, AZ.
International Congress on Integrative Medicine and Health (poster presentation), May 20, 2016, Las Vegas, NV.
References
- Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: united States, 2002–2012. In: National health statistics reports; no 79. Hyattsville, MD: National Center for Health Statistics; 2015.
- Peregoy JA, Clarke TC, Jones JI, Stussman BJ, Nahin RL. Regional Variation in Use of Complementary Health Approaches by U.S. Adults. In: National health statistics reports; no 146. Hyattsville, MD: National Center for Health Statistics; 2015.
- Kantor ED, Rehm CD, Du M, White E, Giovannucci EL. Trends in dietary supplement use among US adults from 1999-2012. JAMA. 2016;316(14):1464-1474. https://doi.org/10.1001/jama.2016.14403
- Adams KM, Kohlmeier M, Zeisel SH. Nutrition education in U.S. medical schools: latest update of a national survey. Acad Med. 2010;85(9):1537-1542. https://doi.org/10.1097/ACM.0b013e3181eab71b
- Patel SJ, Kemper KJ, Kitzmiller JP. Physician perspectives on education, training, and implementation of complementary and alternative medicine. Adv Med Educ Pract. 2017;8:499-503. https://doi.org/10.2147/AMEP.S138572
- Chao MT, Wade C, Kronenberg F. Disclosure of complementary and alternative medicine to conventional medical providers: variation by race/ethnicity and type of CAM. J Natl Med Assoc. 2008;100(11):1341-1349. https://doi.org/10.1016/S0027-9684(15)31514-5
- Karpa K. Development and implementation of an herbal and natural product elective in undergraduate medical education. BMC Complement Altern Med. 2012;12(1):57. https://doi.org/10.1186/1472-6882-12-57
- Kemper KJ, Amata-Kynvi A, Sanghavi D, et al. Randomized trial of an internet curriculum on herbs and other dietary supplements for health care professionals. Acad Med. 2002;77(9):882-889. https://doi.org/10.1097/00001888-200209000-00014
- McCune JS, Hatfield AJ, Blackburn AA, Leith PO, Livingston RB, Ellis GK. Potential of chemotherapy-herb interactions in adult cancer patients. Support Care Cancer. 2004;12(6):454-462. https://doi.org/10.1007/s00520-004-0598-1
- Lebensohn P, Kligler B, Brooks AJ, et al. Integrative medicine in residency: feasibility and effectiveness of an online program. Fam Med. 2017;49(7):514-521.
- Kligler B, Gordon A, Stuart M, Sierpina V. Suggested curriculum guidelines on complementary and alternative medicine: recommendations of the Society of Teachers of Family Medicine Group on Alternative Medicine. Fam Med. 2000;32(1):30-33.
- Gardiner P, Filippelli AC, Lebensohn P, Bonakdar R. Family medicine residency program directors attitudes and knowledge of family medicine CAM competencies. Explore (NY). 2013;9(5):299-307. https://doi.org/10.1016/j.explore.2013.06.002
- Liaison Committee on Medical Education. Functions and Structure of a Medical School. In: Standards for Accreditation of Medical Education Programs Leading to the M.D. Degree. 2015.
- Gaster B, Unterborn JN, Scott RB, Schneeweiss R. What should students learn about complementary and alternative medicine? Acad Med. 2007;82(10):934-938. https://doi.org/10.1097/ACM.0b013e318149eb56
- Brokaw JJ, Tunnicliff G, Raess BU, Saxon DW. The teaching of complementary and alternative medicine in U.S. medical schools: a survey of course directors. Acad Med. 2002;77(9):876-881. https://doi.org/10.1097/00001888-200209000-00013
- Institute of Medicine Committee on the Use of Complementary and Alternative Medicine. Complementary and Alternative Medicine in the United States. Washington, DC: National Academies Press; 2005.
- Prajapati SH, Kahn RF, Stecker T, Pulley L. Curriculum planning: a needs assessment for complementary and alternative medicine education in residency. Fam Med. 2007;39(3):190-194.
- Lebensohn P, Kligler B, Dodds S, et al. Integrative medicine in residency education: developing competency through online curriculum training. J Grad Med Educ. 2012;4(1):76-82. https://doi.org/10.4300/JGME-04-01-30
- Ajzen I, Fishbein M. Questions raised by a reasoned action approach: comment on Ogden (2003). Health Psychol. 2004;23(4):431-434. https://doi.org/10.1037/0278-6133.23.4.431
- Kligler B, Maizes V, Schachter S, et al; Education Working Group, Consortium of Academic Health Centers for Integrative Medicine. Core competencies in integrative medicine for medical school curricula: a proposal. Acad Med. 2004;79(6):521-531. https://doi.org/10.1097/00001888-200406000-00006
- U.S. Food and Drug Administration. Dietary Supplements. U.S. Department of Health and Human Services Website. September 17, 2015. http://www.fda.gov/Food/DietarySupplements/. Accessed October 3, 2015.
- Natural Medicines Comprehensive Database. Stockton, CA: Therapeutic Research Faculty. http://naturaldatabase.therapeuticresearch.com/home.aspx. Accessed 2014-2016.
- Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA. 1998;279(15):1200-1205. https://doi.org/10.1001/jama.279.15.1200
- Mowry JB, Spyker DA, Cantilena LR Jr, McMillan N, Ford M. 2013 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 31st Annual Report. Clin Toxicol (Phila). 2014;52(10):1032-1283. https://doi.org/10.3109/15563650.2014.987397
- Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. In: National health statistics report; no. 12. Hyattsville, MD: National Center for Health Statistics; 2008.
- Schneider CD, Meek PM, Bell IR. Development and validation of IMAQ. BMC Med Educ. 2003;3(1):5. https://doi.org/10.1186/1472-6920-3-5
- Lie D, Boker J. Development and validation of the CAM Health Belief Questionnaire (CHBQ) and CAM use and attitudes amongst medical students. BMC Med Educ. 2004;4(1):2. https://doi.org/10.1186/1472-6920-4-2




There are no comments for this article.