Background and Objectives: Medical students have been training in rural environments for many years. However, there is sparse research demonstrating that training in a rural environment provides an equivalent learning experience to training in an academic medical setting. This study addresses that gap by comparing student performance after training in rural or community environment versus an academic setting while completing the family medicine clerkship.
Methods: Participants in this retrospective cohort study were students who completed an 8-week family medicine third-year clerkship between 2013 and 2016. Half spent the first 4 weeks in a rural or community setting while the other half were in an academic setting. These placements were reversed after midterm exams. Data were collected from both student academic files and from rural rotation tracking systems at two time points: midterm and following the 8-week rotation.
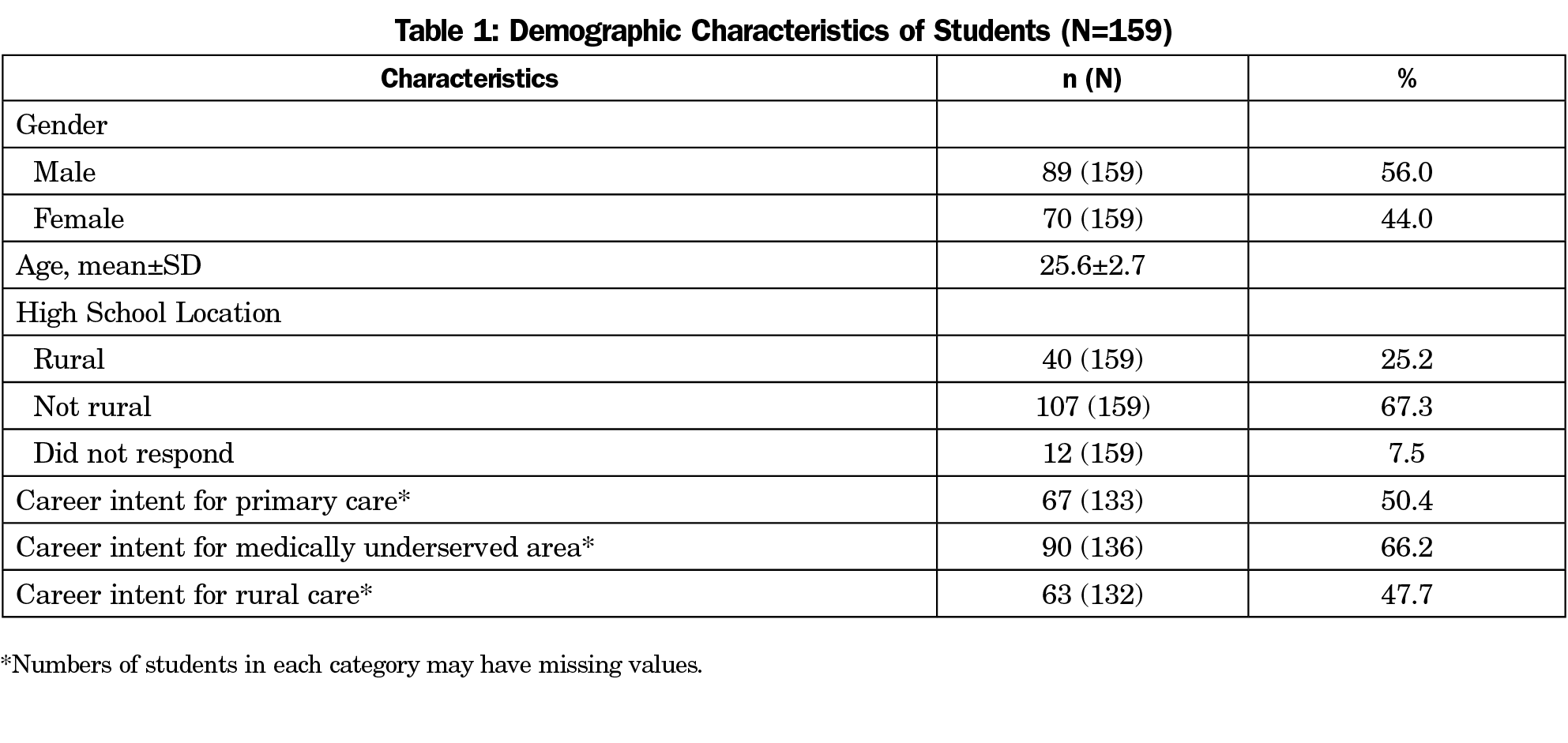
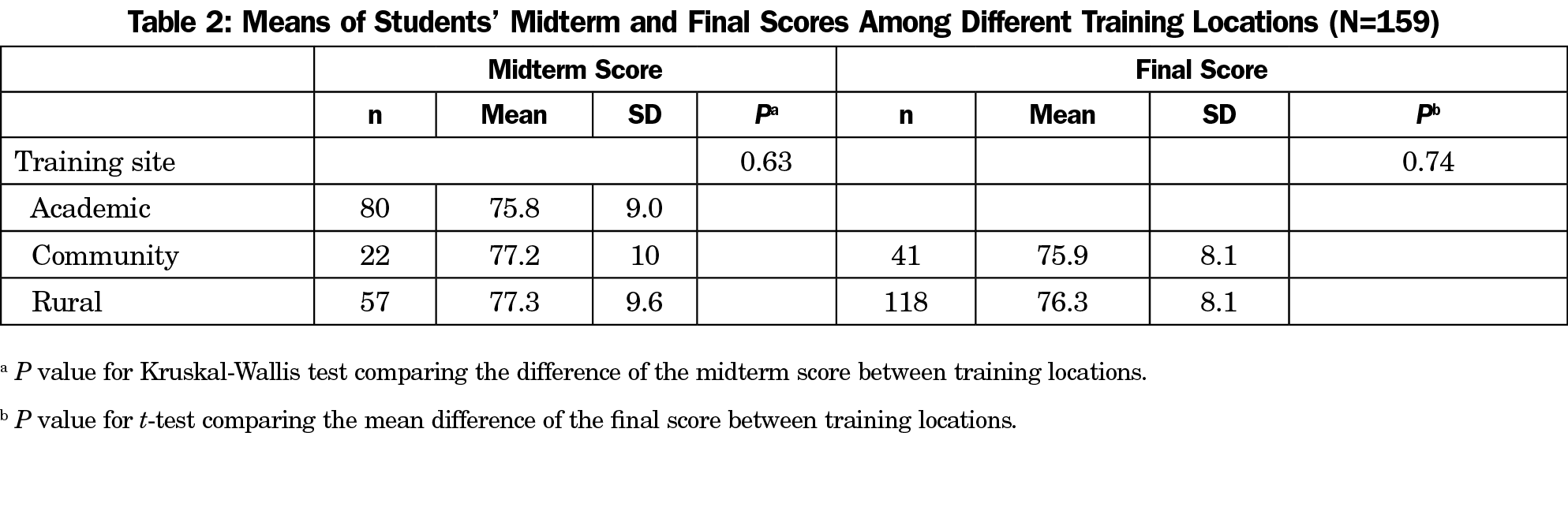
Results: Results from our sample of 159 medical students (89 [56.0%] male and 70 [44.0%] female) revealed no statistically significant differences in students’ midterm (P=.63) and final scores (P=.74) based on training locations.
Conclusions: Study findings suggest that rural and academic clerkships provide equivalent levels of knowledge for family medicine students. This finding has particular relevance for students whose intent is to practice in a rural location. Additional research is needed to identify if these findings are generalizable to other medical schools and locations.
Medical students have been training in rural environments for many years.1 Rural rotations offer a unique setting and population for family medicine practice, and rural rotations are often rated highly by students and preceptors.2 Exposure to rural medicine is believed to increase student interest in future practice in rural locations3 and improve students’ interest in rural medicine.4 This is particularly important since rural areas consistently experience a shortage of primary care physicians.5
Recent work has shown that students who train in the rural environment do not feel that their training in this setting places them at an academic disadvantage.6 In fact, students who participated in longitudinal integrated clerkships in rural settings reported an increased sense of confidence in clinical skills when compared to their urban counterparts6 and demonstrated better patient interaction skills.7 Previous studies have found that training in the rural environment is comparable to training in the academic environment in situations where students self-selected to train in the rural environment.8,9 Students at the University of Minnesota participating in primary care rotations in the rural environment for a total of 9 months were found to have similar scores on National Board of Medical Examiners (NBME) exams, Step One, and Step Two exams when compared to those completing the traditional curriculum.7 This finding was similar to students at the University of Kansas, where scores were equivalent across a 2-month rotation in the rural environment.8
However, there is little research documenting if training in rural environments provides an overall equivalent learning experience to training in an academic medical setting when students did not self-select the nonacademic settings. The primary aim of this study was to compare student exam scores between rural and academic settings for a third-year family medicine clerkship. We hypothesized that student scores will be similar across the rural family medicine environment and the academic family medicine environment. Since some nonacademic clerkships also involved nonrural community settings, we also examined the comparability of these settings to rural and academic environments. A secondary study aim was to evaluate performance when controlling for students’ intent to practice in a rural setting and controlling for the location from which a student hails.
Sample
This retrospective cohort study involved159 third-year medical students completing their family medicine clerkship at the West Virginia University School of Medicine (WVUSOM) Morgantown campus in years 2013 through 2016.
Setting
Rural settings were defined as practices located in an area defined as having a Rural Urban Commuting Area (RUCA) Code10 of four or greater. Community settings are defined as having a RUCA code below four but a training site not under the academic setting. The academic setting was a large tertiary care academic family medicine clinic.
Design
The overall purpose of the 8-week rotation was to provide students with both an academic and a nonacademic (rural or community) clerkship experience. Prior to the start of the 8-week rotation, half of the students were randomly assigned to spend the first 4 weeks training in the rural or community setting and the second 4 weeks training in the academic setting. Community settings were included with rural settings based on the need to have additional rotation sites. The remaining half spent the first 4 weeks training in the academic setting and the second 4 weeks in the rural or community setting.
Data Collection
Data were collected from student academic files and a rotation tracking system. The midterm score is a nationally-developed test on subjects important to family medicine and the final score is the family medicine NBME subject exam. All students completed a survey about intent to practice when they completed their rural or community rotation. This survey was completed after the rural rotation finished. Although the survey was not anonymous, the data was provided deidentified to the authors who worked on the analysis (T.H. and J.X.). Rural locations were converted to Rural-Urban Commuting Area (RUCA) codes. The West Virginia University Institutional Review Board approved this study.
Statistical Analysis
Data were analyzed using SAS (version 9.3. 2012 SAS Institute Inc, Cary, NC). Descriptive analysis was performed for demographic variables to get basic information of the sample. Since student midterm exam scores were not normally distributed, we used nonparametric Kruskall-Wallis test to compare the differences of the students’ midterm score among three different training locations. Examining the midterm scores allowed for group comparisons prior to carry-over effects from the second half of the rotation. We used a t-test to compare students’ final NBME scores between community and rural locations in order to further examine comparability between these two nonacademic settings. Groups analyzed for the final score included one group that completed an academic rotation and a rural rotation, and a second group that completed an academic rotation and a community rotation.
Multiple regression analyses were also conducted on both midterm and final scores to examine the association between training locations and students’ scores after controlling for students’ career intentions and high school locations. All statistical tests were two-sided and a P value of <.05 was considered statistically significant.
This study included a sample of 159 medical students; 89 (56.0%) male and 70 (44.0%) female. See Table 1 for demographic information. The mean student age was 25.6 years (SD=2.7); 74.8% of students were from nonrural areas, and 25.2% were from rural areas. Among these participants, 50.4% reported an intention to practice in primary care, 66.2% in medically underserved areas, and 47.6% in rural settings (Table 1).
Prior to the midterm score, 50.3% of participants were trained in an academic setting, and 13.8% and 35.9% were trained in community and rural settings, respectively. Prior to the final score, 100% of the students completed an academic portion of the family medicine rotation, 25.8% completed a community rotation, and 74.2% completed a rural rotation. The results of the Kruskal-Wallis test shown in Table 2 indicate that there were no statistically significant differences in students’ midterm (P=.63) among academic, rural, and community settings. The t-test results revealed that there was no significant difference in final exam scores between students who received an academic 4-week experience plus a rural 4-week experience, and those who received an academic 4-week plus a 4-week community experience (P=.74). The multiple regression analysis also showed that there was no association between training locations and students’ midterm and final scores after controlling for students’ career intents and their high school locations.
This study shows no statistical difference in training among rural, community, and academic settings within this family medicine clerkship. This randomized study adds to the literature demonstrating that training in rural settings can be an acceptable alternative to training in the academic environment. Previous studies have reviewed student performance on training in rural environments in relation to their peers who have trained in academic settings, when students self-selected rural training. Although the length time of training in the rural environment has varied, students have shown no statistically significant difference in academic performance.6,7,9 Utilizing the results of this study along with previous studies, educators can have confidence that training in the rural setting provides similar outcomes to those of an academic training experience. Replication of these findings is important to provide an evidence base for rural training in medical education.
Rural areas have sustained a continued shortage of primary care physicians.5 Utilizing student rotations, we are able to increase medical student interest in practice in the rural environment.3,5 This study also showed that scores have no statistical difference when controlling for the intention of a student to practice in the rural setting. It also revealed that students from rural hometowns were shown to perform at a similar level on their rotations compared to students who were not from a rural area.
This study is limited in generalizability since it was conducted at a single medical school during the family medicine clerkship. Another limitation is that the students had all completed both a nonacademic rotation and an academic rotation before the final NBME exam, making the analysis unclear as to the specific effects of the nonacademic rotation on the NBME exam results.
Rurality of a rotation, student rural upbringing, or a student’s intent to practice in a rural location does not change the student’s performance while on the family medicine clerkship rotation. More research is needed to identify if these findings are generalizable to other medical schools and locations.
Acknowledgments
Funding: Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number 5U54GM104942-03. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors acknowledge West Virginia University Institute for Community and Rural Health, who assisted with data collection on student demographics and rural rotations.
Previous Presentation: Haggerty T, Xiang J, Hanks H, Unger K. The impact of training in a rural environment for third year medical students on a family medicine rotation: findings from a retrospective cohort study. Poster presented at: North American Primary Care Research Group Annual Meeting. Montreal, QC. November 2017.
References
- Chen F, Fordyce M, Andes S, Hart LG. Which medical schools produce rural physicians? A 15-year update. Acad Med. 2010;85(4):594-598. https://doi.org/10.1097/ACM.0b013e3181d280e9
- Barrett FA, Lipsky MS, Lutfiyya MN. The impact of rural training experiences on medical students: a critical review. Acad Med. 2011;86(2):259-263. https://doi.org/10.1097/ACM.0b013e3182046387
- Isaac V, Watts L, Forster L, McLachlan CS. The influence of rural clinical school experiences on medical students’ levels of interest in rural careers. Hum Resour Health. 2014;12(1):48. https://doi.org/10.1186/1478-4491-12-48
- Roseamelia C, Greenwald JL, Bush T, Pratte M, Wilcox J, Morley CP. A qualitative study of medical students in a rural track: views on eventual rural practice. Fam Med. 2014;46(4):259-266.
- Rosenblatt RA. Commentary: do medical schools have a responsibility to train physicians to meet the needs of the public? The case of persistent rural physician shortages. Acad Med. 2010;85(4):572-574. https://doi.org/10.1097/ACM.0b013e3181d306b8
- Caygill R, Peardon M, Waite C, Wright J. Comparing a longitudinal integrated clerkship with traditional hospital-based rotations in a rural setting. Med Teach. 2017;39(5):520-526. https://doi.org/10.1080/0142159X.2017.1297893
- Zink T, Power DV, Olson K, Harris IB, Brooks KD. Qualitative differences between traditional and rural-longitudinal medical student OSCE performance. Fam Med. 2010;42(10):707-711.
- Maxfield H, Kennedy M, Delzell JE, Paolo AM. Performance of third-year medical students on a rural family medicine clerkship. Fam Med. 46(7):536-538.
- Zink T, Power D V, Finstad D, Brooks KD. Is there equivalency between students in a longitudinal, rural clerkship and a traditional urban-based program? Fam Med. 42(10):702-706. http://www.ncbi.nlm.nih.gov/pubmed/21061201. Accessed November 6, 2018.
- United States Department of Agriculture Economic Research Service. Rural-Urban Commuting Area Codes. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx. Accessed November 6, 2018.



There are no comments for this article.