Background and Objectives: The Advanced Life Support in Obstetrics (ALSO) course is widely utilized in the United States as an evidence-based program that bridges knowledge gaps and improves skills via hands-on training, group learning, and memorization of standardized mnemonics in a team-based approach to patient care. This reduces communication barriers among maternity care providers, ultimately decreasing potential negative outcomes. A needs assessment identified that Serbian providers would benefit from structured learning and hands-on simulation approaches in obstetrics from a structured training like the ALSO course. The objective of this study was to explore the changes in clinicians’ knowledge and preferred scenario responses in managing obstetrics cases before and after participation in the ALSO course.
Methods: The ALSO training lasted 2 days and included lecture sessions, interactive workshops, a written knowledge test, and a simulated skills test. Participants completed an additional 20-item questionnaire assessing their knowledge and preferred scenario responses two weeks pre- and immediately post-ALSO training. Using a paired t test we assessed changes between pre- and posttest knowledge and preferred scenario response scores.
Results: Twenty-seven participants provided complete data. For the entire sample, the pretest mean number of correct items on the knowledge and preferred scenario response assessment was 10.8 and the posttest mean number correct was 15.2, representing an increase of 4.4 correct answers (P<.001).
Conclusions: The current results suggest that the ALSO course can successfully increase knowledge and preferred scenario responses in Serbian providers and may be a viable approach to improving birth outcomes.
When unpredictable obstetric emergencies rapidly emerge, successful management involves well-coordinated, multidisciplinary teamwork to avoid detrimental outcomes. Preparation for such emergencies requires sustainable teaching courses and simulation training in a safe, nonclinical environment1; the American Academy of Family Physicians (AAFP) recognizes the Advanced Life Support in Obstetrics (ALSO) as an evidence-based program using an approach in obstetric emergencies.2 Global outreach to improve health care around the world is needed. Courses like ALSO can provide a platform for best practices for a learner to develop knowledge and skills necessary to effectively manage perinatal emergencies.3,4
On previous visits and needs assessments, a new style of a team approach with structured learning and hands-on simulation in emergency obstetrics would benefit clinician education. Serbian obstetrics and gynecology resident physicians are usually observers and do not have hands-on experience with emergency obstetric scenarios. In partnership with our academic family medicine residency and Kybele (a humanitarian organization working to improve international childbirth safety), we assembled a team of ALSO-certified instructors and providers to travel to teach the ALSO course in Novi Sad, Serbia. The purpose of this study was to assess if participants with no prior exposure to ALSO, and English as a second language, would gain knowledge and simulated clinical skills to empower management of obstetric emergencies through content-focused pre/postquestions and the ALSO course.
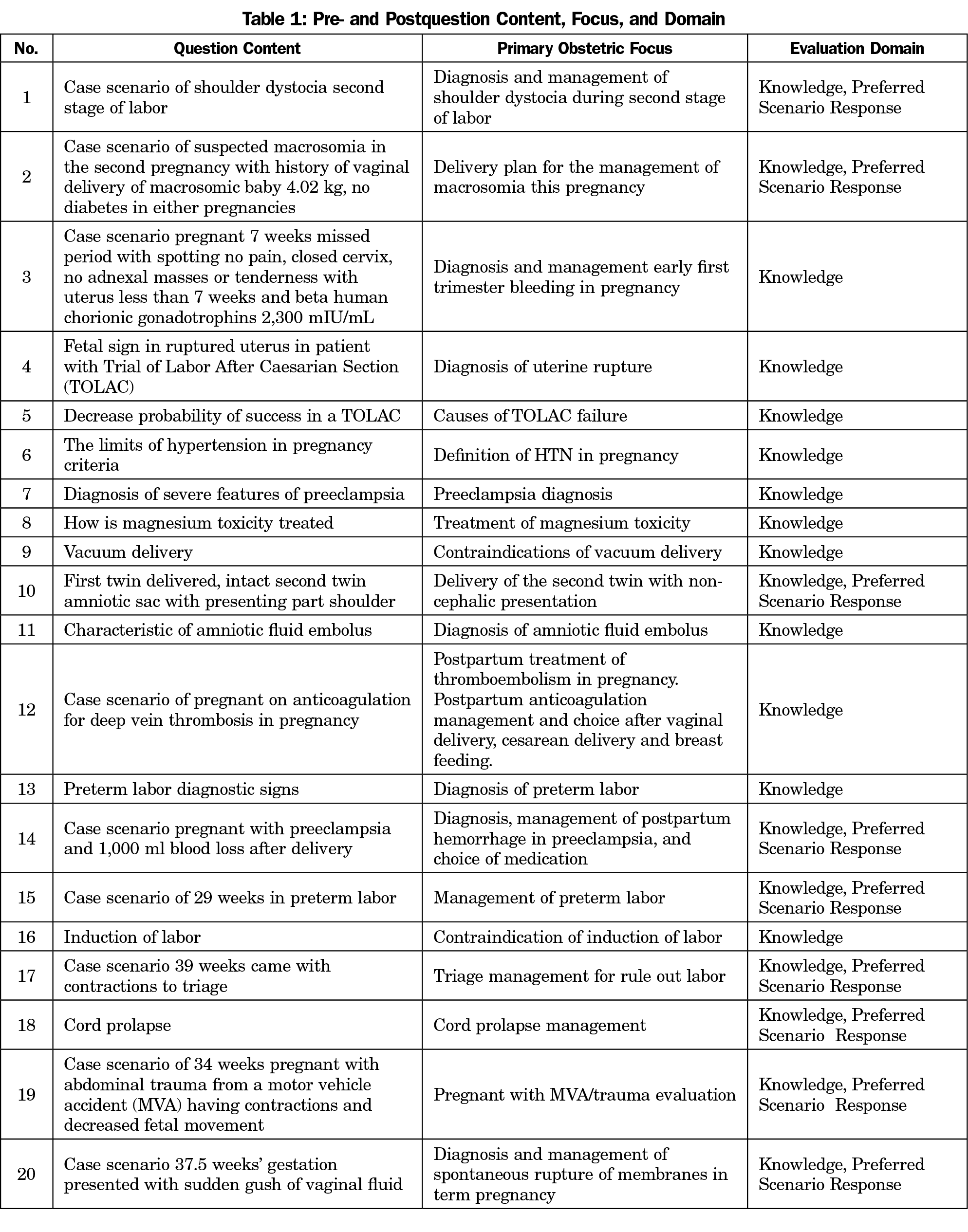
AAFP provided permission to use ALSO course materials for this project. The Institutional Review Board at the lead author’s practice approved the protocol. All participants completed informed consent. Kolb’s Experiential Learning Theory provided the framework for the learning process of adult development that included a pre and posttest assessment with simulation.5 The participants were from Novi Sad and neighboring cities representing multiple disciplines with the majority from obstetrics (faculty, residents). A 20-item questionnaire was developed (Table 1), drawing from existing questionnaires and expert input to assess provider knowledge and preferred scenario responses using a Likert-type response format. The questionnaire was administered 2 weeks prior to, and again immediately following ALSO training. The training lasted 2 days and included lecture sessions, interactive workshops, a written knowledge test, and a simulated skills test. On day two, participants underwent the standard ALSO evaluation process with a written test and a mega-delivery for simulation of clinical skills. Differences in pre- and postscores on the written knowledge test were assessed with a paired t-test in Stata 14 (Stata Corp, College Station, TX). We set significance at P<.05.
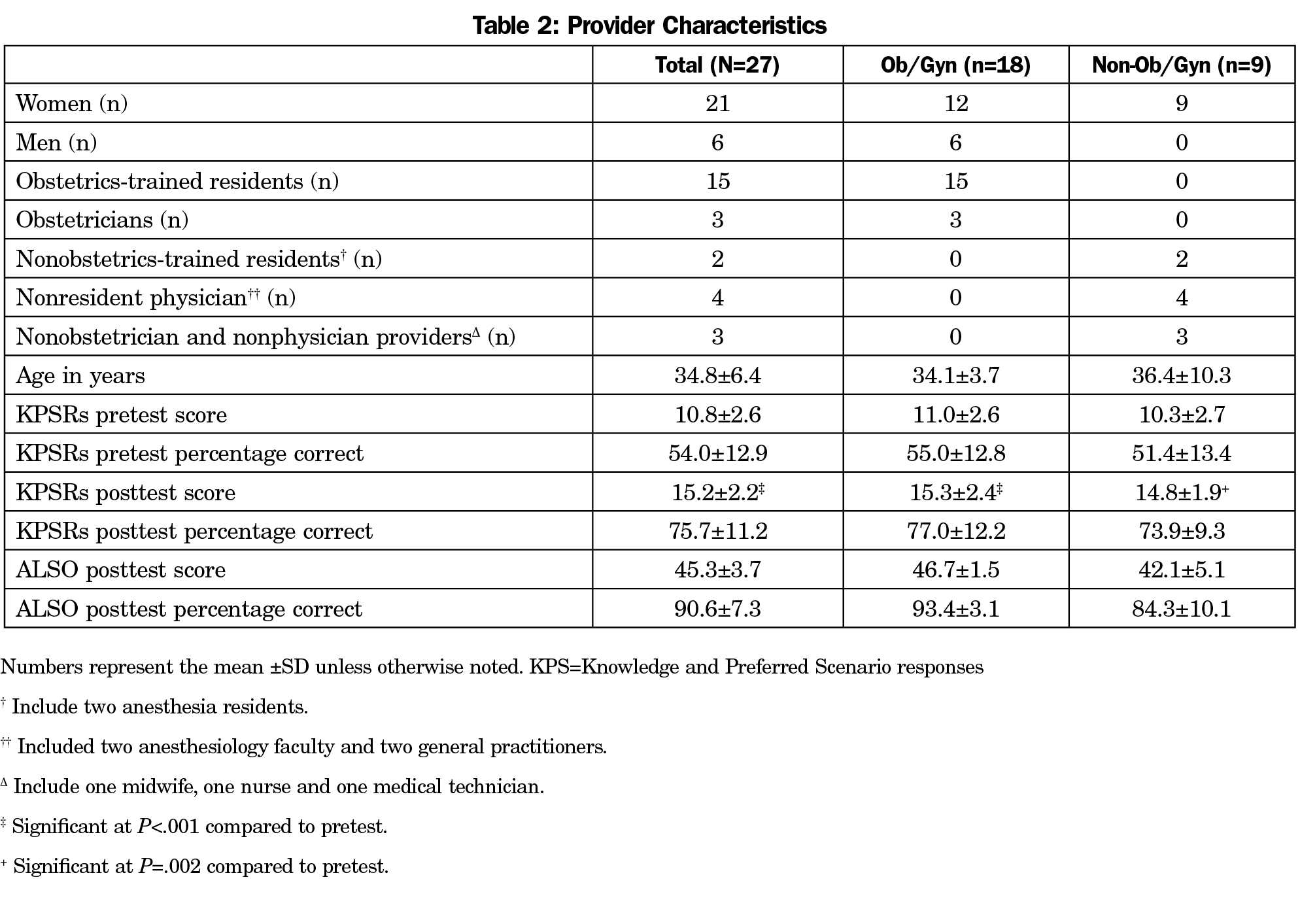
Thirty-five participants attended the ALSO course, with 27 completing pre- and posttest questionnaires. Participants were primarily female (n=21), early career (aged 34.8.±6.4 years), and were primarily from Novi Sad (n=15) and surrounding areas (Table 2). Participants were comprised of obstetrics-trained residents (n=15), obstetricians (n=3), nonobstetrics-trained residents (n=2), nonresident physicians (n=4), a nonobstetrician and nonphysician providers (n=3). Participants were lost to follow-up due to being scheduled for call (n=1) or conflicting travel plans (n=7). With the exception of living outside of the city, participants who could not complete the posttest were not different from those completing all measurements. Results of the paired t test indicated a significant increase in the average number of correct responses from pretest (10.8±2.6) to posttest (15.2±2.2), representing an increase of 4.4±2.62 (t [26]=8.71, P<.001).
The current study using a content-focused pre/posttesting design with the ALSO course in a lower middle-income country is a practical option to train medical professionals caring for pregnant patients. Performance on the content-focused 20 questions showed statistical improvement in participant knowledge and preferred scenario responses. All participants who completed the course passed both the case scenario (hands-on simulation) and written components of the ALSO course. The results of the present study have some limitations. First, the ALSO course did not have an official pretest, so we had to create a questionnaire that has not been validated. Second, the absence of a comparison or control group may affect internal validity. Fortunately, the design of the study allowed for assessment of pretest questions 2 weeks prior to delivery of the ALSO course, minimizing testing effects such that testing effects are improvements seen in test scores, due to being given a test multiple times in a short timeframe rather than actual improvements in knowledge. Third, a small sample size limits ability to examine group differences in response to the training. However it is a strength that the sample was relatively diverse regarding training and specialization.
Empowering clinicians to recognize and adequately react in certain obstetric conditions would considerably enhance their current training.6 Specifically, the ALSO training prepares clinicians in a simulated working environment, especially in those rare, but potentially fatal situations where correct decisions must be made.7 Challenges to self-sustaining international programs include an unsupportive institution and financial incentive. Clear institutional level commitment may help in overcoming barriers and assuring sustainability of these courses by covering maintenance costs, identifying course leaders, and overcoming staff resistance to participation mainly caused by time constraints and fear of being evaluated in front of others.8 More formal monitoring of the management of pre- and postobstetric emergencies in Serbia could help further capture the impact of the educational intervention and the return on the investment of resources that may result.
ALSO is a standardized approach to teaching skills in obstetrics that can be taught abroad to providers that have English as a second language. If a team approach in obstetrics is desired, our findings support the value of using ALSO training in Eastern European countries such as Serbia. Our findings inform precourse planning for provider education and provide evidence of the usefulness of teaching knowledge, simulated clinical skills, and teamwork in this region of the world. Gaining information about clinician understanding of ALSO concepts before and after formal instruction could inform areas to concentrate training for these countries.
Acknowledgments
The authors acknowledge the Advanced Life Support in Obstetrics (ALSO) program and the Department of Family and Community Medicine obstetric faculty and residents
Disclaimer: A funding collaboration exists between Kybele Organization (www.kybeleworldwide.org), The Office of Global Health at the Wake Forest School of Medicine and the Department of Family and Community Medicine.
References
- Calvert KL, McGurgan PM, Debenham EM, Gratwick FJ, Maouris P. Emergency obstetric simulation training: how do we know where we are going, if we don’t know where we have been? Aust N Z J Obstet Gynaecol. 2013;53(6):509-516. https://doi.org/10.1111/ajo.12120
- Dauphin-McKenzie N, Celestin MJ, Brown D, González-Quintero VH. The advanced life support in obstetrics course as an orientation tool for obstetrics and gynecology residents. Am J Obstet Gynecol. 2007;196(5):e27-e28. https://doi.org/10.1016/j.ajog.2006.10.912
- Deutchman M, Dresang L, Winslow D. Advanced life support in obstetrics (ALSO) international development. Fam Med. 2007;39(9):618-622.
- Dresang LT, González MM, Beasley J, et al. The impact of Advanced Life Support in Obstetrics (ALSO) training in low-resource countries. Int J Gynaecol Obstet. 2015;131(2):209-215. https://doi.org/10.1016/j.ijgo.2015.05.015
- Poore JA, Cullen DL, Schaar GL. Simulation-based interprofessional education guided by Kolb’s Experiential Learning Theory. Clin Simul Nurs. 2014;10(5):e241-e247. https://doi.org/10.1016/j.ecns.2014.01.004
- Engels PT, de Gara C. Learning styles of medical students, general surgery residents, and general surgeons: implications for surgical education. BMC Med Educ. 2010;10(1):51. https://doi.org/10.1186/1472-6920-10-51
- Walker LJ, Fetherston CM, McMurray A. Perceived changes in the knowledge and confidence of doctors and midwives to manage obstetric emergencies following completion of an Advanced Life Support in Obstetrics course in Australia. Aust N Z J Obstet Gynaecol. 2013;53(6):525-531. https://doi.org/10.1111/ajo.12110
- Ayres-de-Campos D, Deering S, Siassakos D. Sustaining simulation training programmes—experience from maternity care. BJOG. 2011;118(suppl 3):22-26. https://doi.org/10.1111/j.1471-0528.2011.03177.x



There are no comments for this article.