The United States lacks enough primary care physicians to meet the needs of the public and ensure optimum health outcomes.1 Medical students who choose to enter family medicine represent the largest contribution to the primary care workforce compared to other specialties.2 Much is known about the demographics, student factors, and medical school experiences that predict a student choosing to become a family physician.3-6 Validated instruments such as the Brief Family Medicine Interest Survey (FMIS) exist to determine a student’s likelihood of eventually choosing family medicine as a career upon matriculation to medical school.7 A previous study by this group suggested that family medicine interest group (FMIG) participation was one extracurricular activity that was associated with entering family medicine as a career; other studies have been mixed.8-10 The goal of this study was to determine if FMIG participation is associated with increased choice of family medicine career given different levels of initial interest, as nearly all US medical schools host FMIGs.11 It was our prediction that engagement with FMIG is associated with increased choice of family medicine as a specialty.
BRIEF REPORTS
Association of Family Medicine Interest at Matriculation to Medical School and FMIG Participation With Eventual Practice as a Family Physician
Amanda Kost, MD, MEd | Kimberly Kardonsky, MD | Jeanne Cawse-Lucas, MD | Tomoko Sairenji, MD, MS
Fam Med. 2019;51(8):682-686.
DOI: 10.22454/FamMed.2019.239373
Background and Objectives: An adequate family medicine workforce is needed to improve health and health care outcomes in the United States, yet few medical students in the US become family physicians. Indicators of family medicine interest upon medical school matriculation exist. Family medicine interest groups (FMIGs) may influence student choice. This study examines the association of FMIG participation with various matriculation interest indicators to predict which students go on to become family physicians.
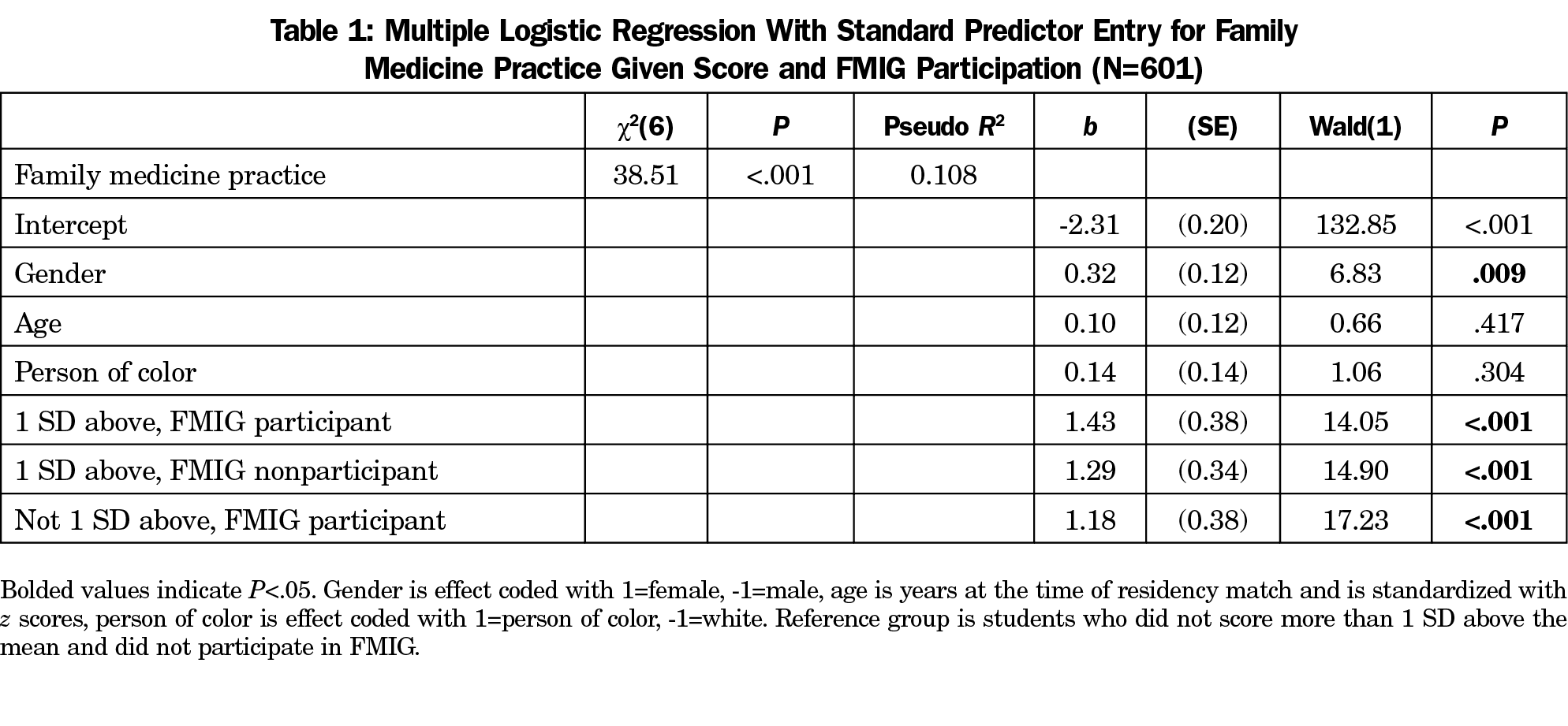
Methods: The American Medical Association Masterfile was used to identify the practice specialty of 601 graduates of the University of Washington School of Medicine who matriculated between 2003 and 2007. Graduates’ scores on the Family Medicine Interest Survey (FMIS) and whether a student listed family medicine as their top choice upon matriculation along with FMIG participation and demographic characteristics were used in a binary logistic regression model to predict eventual practice. The model output was used to calculate odds ratios and predicted probabilities of family medicine practice given initial family medicine interest and FMIG participation.
Results: FMIG participation was associated with higher odds ratios and increased predicted probability of becoming a family physician regardless of initial interest although the magnitude of the difference varied. FMIG participants who listed family medicine as their top specialty had a 68% predicted probability of entering family medicine compared to 8% probability if they did not list family medicine first and did not participate in FMIG. FMIG participation was associated with odds ratios between 3.27-4.19 for entering family medicine regardless of FMIS score.
Conclusions: Among University of Washington students with family medicine as their top specialty choice upon matriculation, FMIG participation was associated with higher odds of entering the specialty. The same was true, although to a lesser degree, for students who had a high score on the FMIS.
Data Sources
The 2015 American Medical Association Masterfile was used to identify the eventual practice specialty of 601 University of Washington School of Medicine (UWSOM) graduates who matriculated to medical school between 2003 and 2007. The validation and comparison of the FMIS and the single-item screen was previously described. Students were surveyed during orientation week at the time of matriculation, and scores for these instruments were calculated for all 601 graduates in the sample. Participation in FMIG was determined through program records from the Department of Family Medicine. FMIG participation was defined as having attended at least one FMIG event. Data about the number of events attended by each participant was not available for the time period of study.
Variables
The composite score on the Family Medicine Brief Interest Instrument was standardized using z scores. The variable of writing family medicine as the top specialty choice at matriculation was effect coded: the response “family medicine” was given 1, all other responses –1, including 7% of students who reported being undecided in specialty choice. Practice outcomes were dummy coded, with 1 being family medicine and 0 being all others.
To determine the interaction of FMIG with the single-item screen and the FMIS, two sets of categorical variables were created. The first set of categorical variables captured students with and without FMIG participation, and composite score one standard deviation (1 SD) above the mean on the 15 item-FMIS:
- FMIG participants who scored higher than 1 SD above the mean
- FMIG participants who did not score higher than 1 SD above the mean
- FMIG nonparticipants who scored higher than 1 SD above the mean
- FMIG nonparticipants who did not score higher than 1 SD above the mean (reference group)
The second set of categorical variables captured students with and without FMIG participation, listing family medicine as top specialty choice:
- FMIG participants who listed family medicine first
- FMIG participants who did not list family medicine first
- FMIG nonparticipants who listed family medicine first
- FMIG nonparticipants who did not list family medicine first (reference group)
Student age, gender, and race/ethnicity were used to control for demographic differences in specialty choice. The age of the student at the time of match to residency was standardized using z scores. The gender of the student was effect coded, with 1 being female and -1 being male. Race/ethnicity was effect coded, with 1 being a person of color and -1 being white.
Procedures
Binary logistic regression with standard predictor entry was performed to establish the relationship between the outcome variables of family medicine practice with each set of categorical variables (FMIG participation and scoring more than 1 SD above the mean; FMIG participation and listing family medicine first) while controlling for the demographic variables of age, gender, and race/ethnicity. Odds ratios and predicted probabilities of family medicine practice were calculated using the regression coefficients.
The University of Washington Institutional Review Board deemed this study exempt. Analyses were performed with SPSS Version 19, IBM.
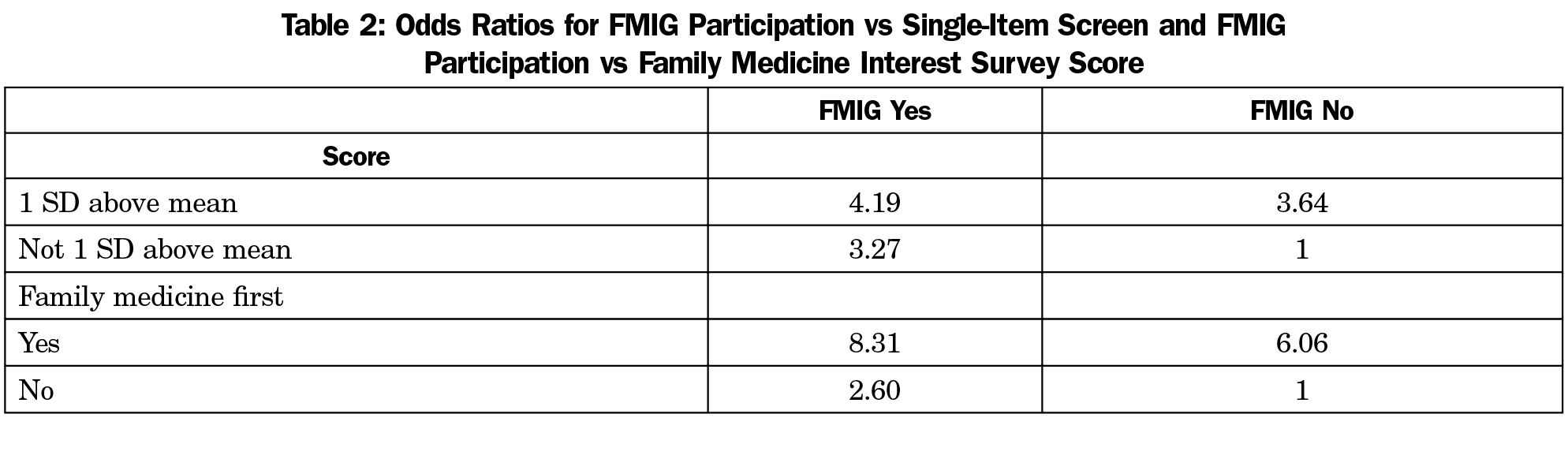
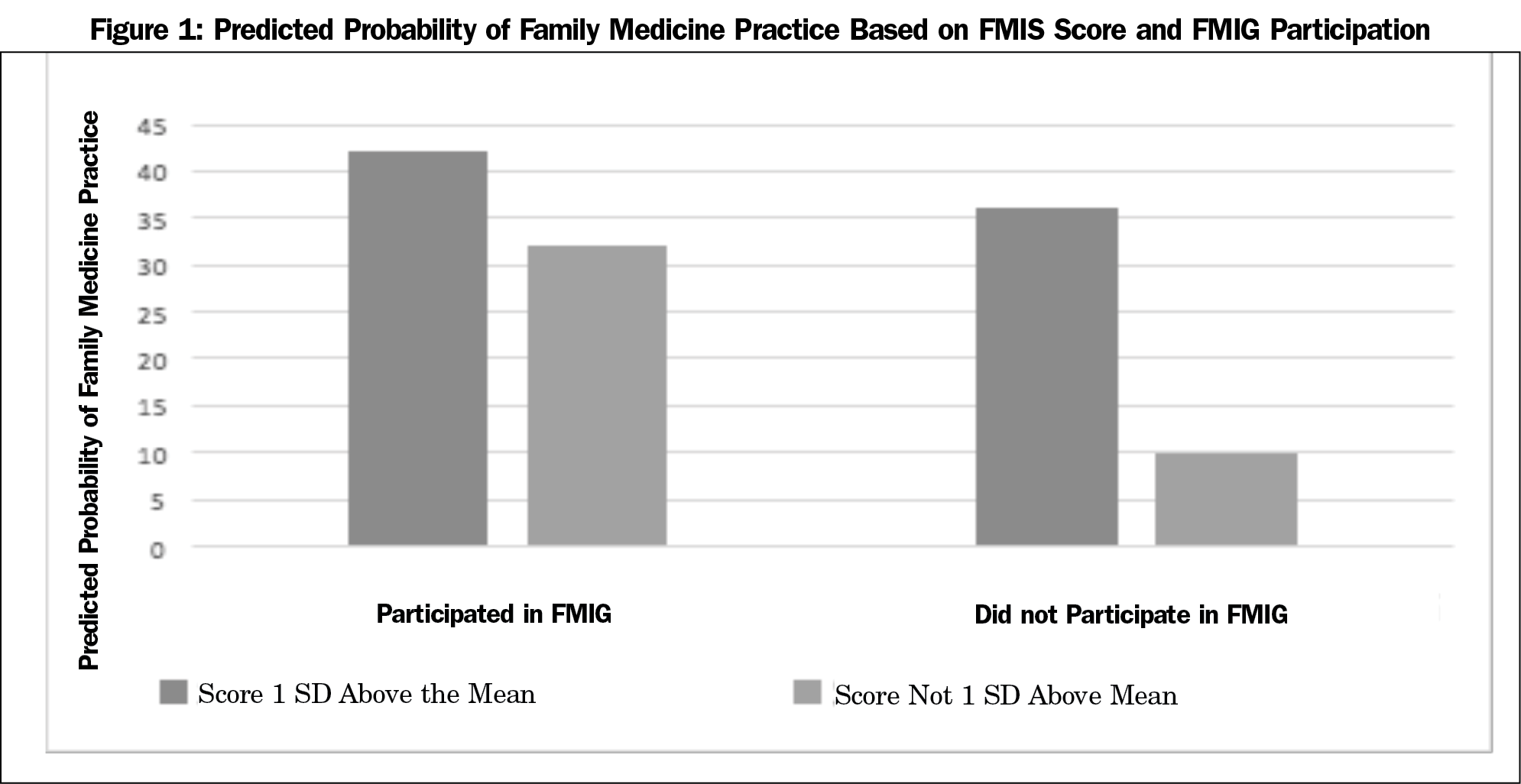
Compared to the reference group that did not score more than 1 SD above the mean and did not participate in FMIG, all other possible group combinations were significantly predictive of family medicine practice (Table 1). FMIG participants who scored more than 1 SD above the mean on the FMIS had an odds ratio of 4.19 compared to the reference group (Table 2). However, FMIG participation had a greater impact on those who did not score 1 SD above the mean, with a 22% difference in predicted probability of entering family medicine compared to only 6% difference for those who did score 1 SD above the mean (Figure 1).
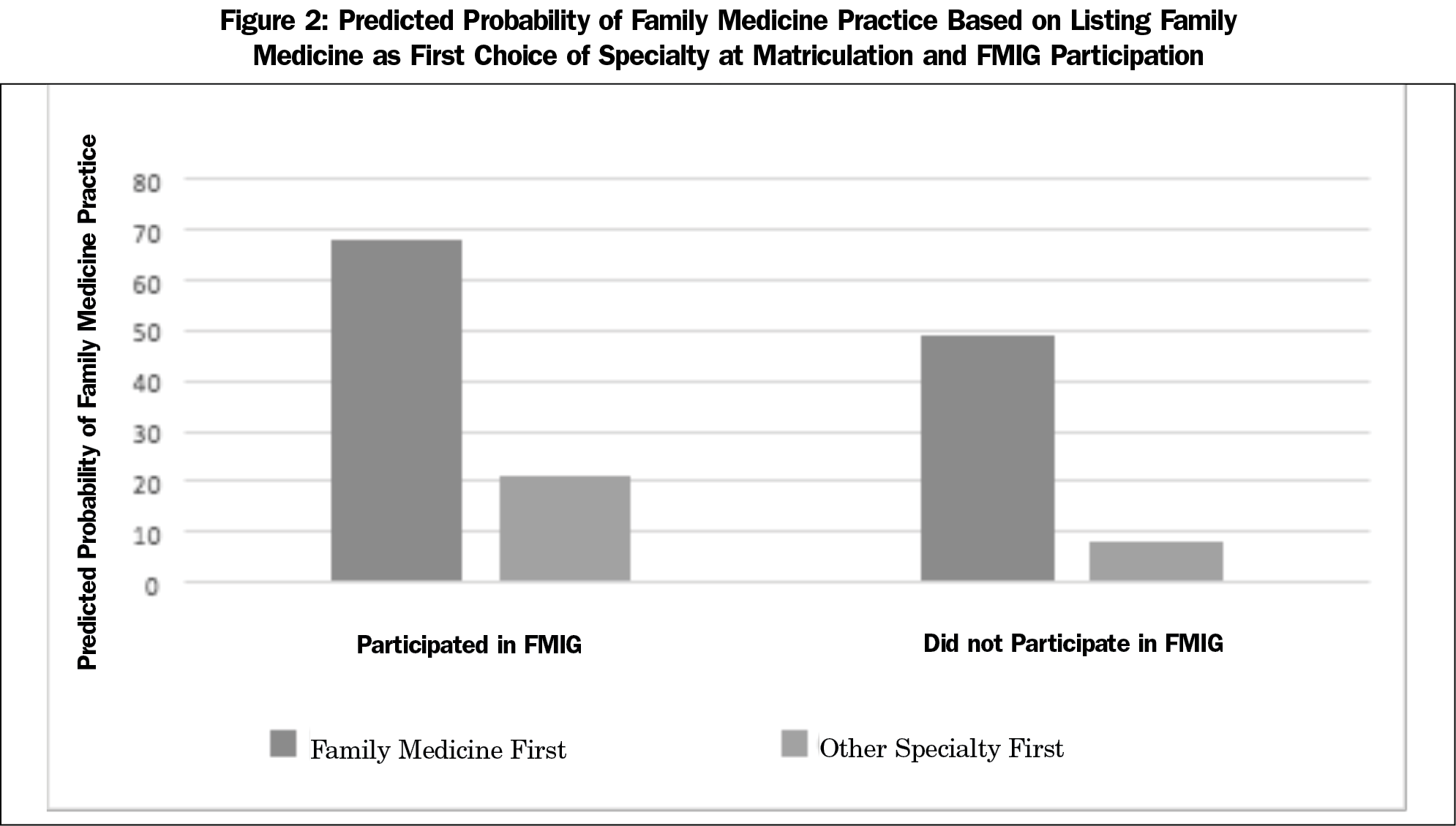
Similarly, compared to the reference group that did not list family medicine as their top specialty choice and did not participate in FMIG, all other possible group combinations were significantly predictive of family medicine practice (Table 3). Listing FM first and participating in FMIG was associated with an odds ratio of 8.31 of entering family medicine compared with the reference group. Of the students who listed family medicine as their top specialty, 19% more students who participated in FMIG ended up in family medicine practice compared to nonparticipants. There was only a 13% increase in predicted probability of family medicine practice for those who participated in FMIG and listed another specialty (Figure 2).
Similar to prior studies, FMIG participation was associated with higher rates of eventual family medicine practice compared to those who did not participate even if students matriculated to school thinking family medicine was their top specialty choice or had high scores on an instrument to measure interest.8 However, the impact of FMIG participation was variable. The association of FMIG participation was greater for students with lower scores on initial family medicine interest survey and for those who listed family medicine as their top specialty choice. FMIG participation is associated with a stronger impact on students with lower FMIS scores and those who listed family medicine as their first choice specialty. While FMIG may reaffirm interest in the discipline for students who are already interested, it may also introduce the specialty to undecided students or increase awareness of its breadth and opportunities to students who were initially uninterested.
Strengths of this study include a large number of graduates over a 5-year period and use of practice data as an outcome measure. Limitations include that it occurred at a single institution so replication of the findings should take place at other schools before accepting it as widely generalizable. Students select into FMIG participation so selection bias may account for the findings. Another limitation is dichotomizing FMIG participation; future studies should explore the association between the number of FMIG events a participant attends and eventual practice outcomes.
FMIG participation is associated with more students entering family medicine. As most US medical schools have FMIGs with limited resources, faculty advisors of such groups may want to consider targeting students who have demonstrated significant interest by indicating family medicine is their top choice upon matriculation. Another target would be those who score lower on the FMIS, although an increase is certainly also seen in students who did not initially intend to match in family medicine. Welcoming everyone and promoting the specialty widely will help reach students who may not initially consider a family medicine career, along with sustaining interest for those who matriculate to school with plans to become a family physician.
Acknowledgments
This study was presented as a seminar under the title “How Do You Know Who Is Interested in Family Medicine and What Are You Going to Do About it?” at the Society of Teachers of Family Medicine Annual Spring Conference in San Diego, CA, May, 2017.
References
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502. https://doi.org/10.1111/j.1468-0009.2005.00409.x
- Bowman RC. Measuring primary care: the standard primary care year. Rural Remote Health. 2008;8(3):1009.
- Lawson SR, Hoban JD, Mazmanian PE. Understanding primary care residency choices: a test of selected variables in the Bland-Meurer model. Acad Med. 2004;79(10)(suppl):S36-S39. https://doi.org/10.1097/00001888-200410001-00011
- Bennett KL, Phillips JP. Finding, recruiting, and sustaining the future primary care physician workforce: a new theoretical model of specialty choice process. Acad Med. 2010;85(10)(suppl):S81-S88. https://doi.org/10.1097/ACM.0b013e3181ed4bae
- Jeffe DB, Whelan AJ, Andriole DA. Primary care specialty choices of United States medical graduates, 1997-2006. Acad Med. 2010;85(6):947-958. https://doi.org/10.1097/ACM.0b013e3181dbe77d
- Specialty and Geographic Distribution of the Physician Workforce. What Influences Medical Student & Resident Choices? Washington, DC: Robert Graham Center; 2009.
- Kost A, Cantone RE, Schneider B, Sairenji T, Palmer R. Validation and Comparison of a Brief Instrument vs a Single-Item Screen to Predict Entry to Family Medicine at Matriculation to Medical School. Fam Med. 2018;50(9):672-678. https://doi.org/10.22454/FamMed.2018.258795
- Kost A, Cawse-Lucas J, Evans DV, Overstreet F, Andrilla CHA, Dobie S. Medical student participation in family medicine department extracurricular experiences and choosing to become a family physician. Fam Med. 2015;47(10):763-769.
- Wei McIntosh E, Morley CP. Family medicine or primary care residency selection: effects of family medicine interest groups, MD/ MPH dual degrees, and rural medical education. Fam Med. 2016;48(5):385-388.
- Hinchey S, LaRochelle J, Maurer D, Shimeall WT, Durning SJ, DeZee KJ. Association between interest group participation and choice of residency. Fam Med. 2011;43(9):648-652.
- Heidelbaugh J, Cooke J, Wimsatt L. Opportunities for medical student engagement with family medicine. Fam Med. 2013;45(7):484-491.
Lead Author
Amanda Kost, MD, MEd
Affiliations: Department of Family Medicine, University of Washington School of Medicine, Seattle, WA
Co-Authors
Kimberly Kardonsky, MD - Department of Family Medicine, University of Washington, Seattle, WA
Jeanne Cawse-Lucas, MD - University of Washington School of Medicine, Department of Family Medicine, Seattle, WA
Tomoko Sairenji, MD, MS - Department of Family Medicine, University of Washington, Seattle, WA
Corresponding Author
Kimberly Kardonsky, MD
Correspondence: Health Sciences Center (E-304), Box 356390, Seattle, WA 98195. 206-543-9425. Fax 206-543-3821.
Email: kardok2@uw.edu
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 



There are no comments for this article.