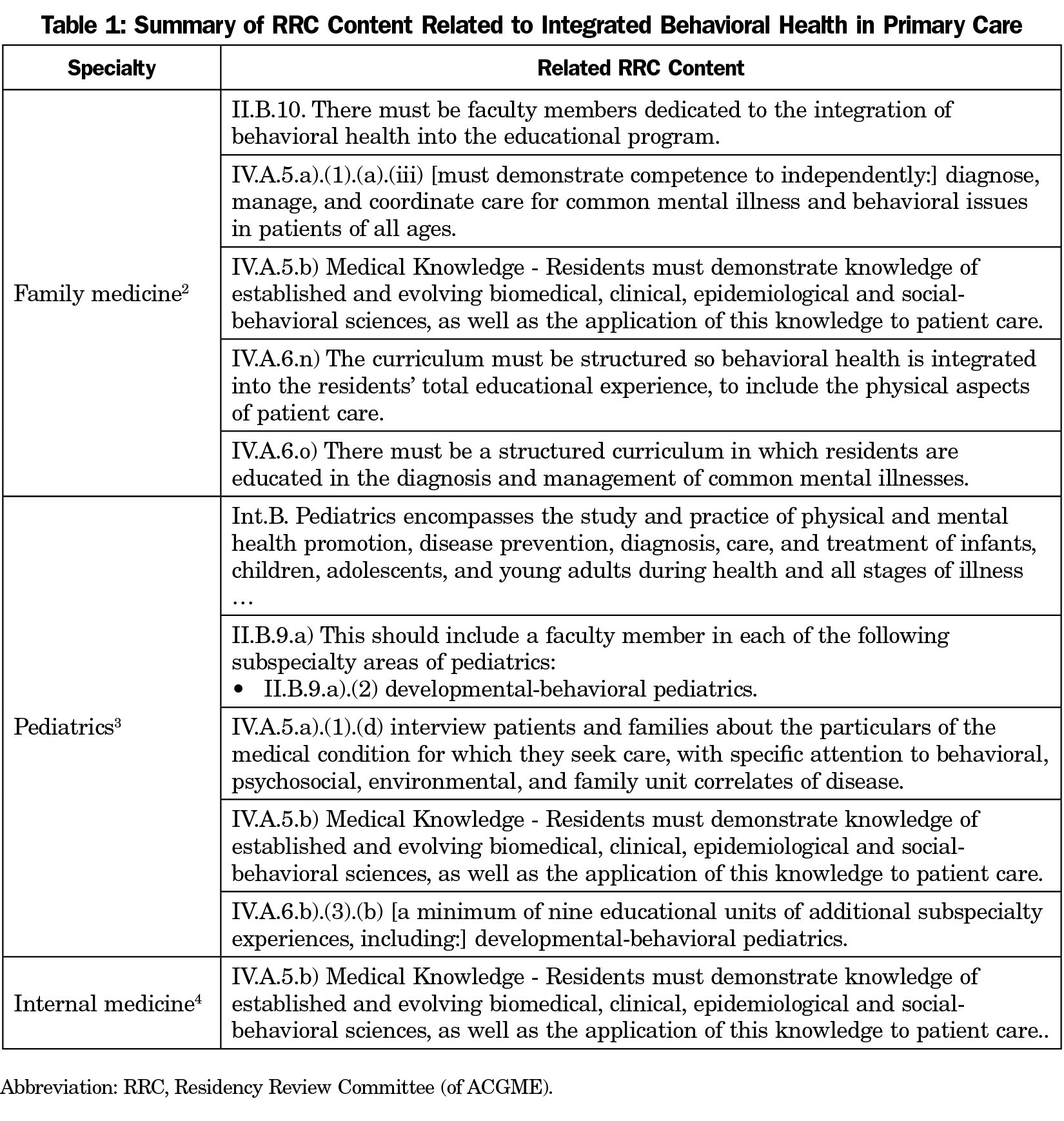
We appreciated Dr Martin and colleagues’ efforts to define the essential skills for family medicine residents practicing integrated behavioral health (IBH) in the March 2019 issue of Family Medicine.1 The resultant work identified 21 observable competencies related to the practice of IBH by family medicine residents. To put the level of guidance provided by Martin et al in context we searched the current Accreditation Council for Graduate Medical Education’s (ACGME) Residency Review Committee (RRC) requirements for family medicine, internal medicine, and pediatrics to identify current standards for primary care residency training in IBH. We reviewed the documents by identifying all content using the search: “menta*,” “behavi*,” and “integrat*.” Table 1 summarizes the findings.
While it would be cumbersome and impractical for the ACGME to provide the granularity of 21 observable competencies for all of the elements defining the scope of family medicine, it is striking how little guidance is provided within primary care for establishing best practices in IBH training. Only family medicine provides a requirement for programs to have faculty members dedicated to the integration of behavioral health into the educational program. Pediatrics requires exposure to faculty with subspecialty training in developmental-behavioral pediatrics, but this is less likely to align with the development of IBH training models than the language of the family medicine RRC requirements. The ability to shape primary care curricula rests in the relative prioritization of the multiple competing demands facing primary care educators. The burden facing the ACGME is to identify the core elements of primary care and to emphasize the elements with the strongest evidence base for improving patient-centered outcomes. IBH is an area where strong evidence suggests its implementation drives improved outcomes. We should work to improve the guidance provided to primary care educators in how to prioritize, implement, and measure the best practices of IBH.
Based on Martin et al’s initial work, improving training in delivering team-based care and enhancing communication skills with interdisciplinary professionals are priorities consistent with essential practices that have been explicated for IBH.5 Enhanced guidance for IBH training could take several forms, including (1) changes to the RRC requirements for family medicine, internal medicine, and pediatrics; (2) the development of more detailed supplementary guidance from the ACGME based upon Martin and colleagues’ 21 competencies explicating the core IBH elements and suggested strategies for their implementation; and/or (3) enhanced opportunities for technical assistance and implementation support to build IBH training capacity. As programs gain experience integrating some or all of the identified IBH competencies into their training curricula, we need to support mechanisms for rigorous evaluation and wide-based dissemination of best practices to the field. Ultimately, we hope centralized training resources and pathways for real-time technical assistance will become available at a national level to support programs seeking to expand their IBH training.



There are no comments for this article.