Background and Objectives: Time spent in the electronic health record (EHR), away from direct patient care, is associated with physician burnout. Yet there is a lack of evidence quantifying EHR use among family physicians. The purpose of the study was to describe a method for quantifying habits and duration of use within the electronic health record in family medicine residents and faculty with particular attention paid to time spent after hours.
Methods: We audited EHR time for family medicine residents and faculty using an EHR vendor-provided, web-based tracking system. We collected and analyzed the number of patient encounters, total time in the EHR per patient, total time in the EHR after hours by physicians for a 6-month time period.
Results: Over the 6-month period reviewed, family medicine trainees and faculty saw between one and 164 patients monthly, spent between 17 and 217 minutes in the EHR per patient, and spent between 0 and 33 hours in the EHR after hours per month.
Conclusions: Family medicine residents spend a significant amount of time completing EHR tasks after hours. Objective EHR data can be used by family medicine residency programs to devise interventions to decrease inefficient use of the EHR, decrease after-hours EHR use, and improve well-being.
There is an increasing national focus on physician wellness and burnout. Half of family physicians report one symptom of burnout, defined as emotional exhaustion, depersonalization, and lack of personal efficacy.1 Wellness is described as an “optimal state of physical, mental, and social well-being.”2 A well physician is professionally fulfilled and “experiences happiness or meaningfulness, self-worth, self-efficacy, and satisfaction at work.” Resident well-being requires harmony with work and home lives.3 Many habits related to well-being are learned in residency.
Use of electronic health records (EHR), “an increase in clerical duties,”2 and after-hours EHR use are all associated with lack of well-being.4-6 Primary care residents who spend more self-reported time working with an EHR after hours have increased burnout and less satisfaction with work-life balance..7 Based on focus group and survey data obtained internally, it is the experience of the residents and faculty in our own program that after-hours EHR use detracts substantially from well-being. However, it was not known how much time was spent by our residents and faculty working with the EHR after hours.
A few studies have quantified physician and resident time spent in the EHR, or “EHR time.” EHR activity of primary care residents and family medicine faculty have been studied in inpatient and outpatient settings.8-11 Methods used to track EHR use include keystrokes and “mouse miles,”8 event logging, direct observation, diaries, and time motion studies.9-11 Studies consistently show marked variation between physicians in EHR time, more time on the computer than in direct patient care, and substantial after-hours EHR use.8-11 We are not aware of a prior study that has used EHR keystrokes and mouse miles to quantify EHR use in an ambulatory setting in a family medicine residency.
The purpose of the study was to quantify and describe variation in resident and faculty EHR use in one family medicine residency program including after-hours use. Objective EHR data and variation between physicians potentially could be used by programs to devise interventions to improve EHR efficiency, decrease after-hours EHR use, and improve well-being.
Subjects
We studied 24 family medicine trainees (postgraduate years 1 through 3) and 10 family medicine faculty at the University of Arizona College of Medicine-Phoenix Family Medicine Residency. All clinicians received training in the EHR software, including 8 hours of hands-on classroom education and 4 hours of one-on-one coaching by the EHR vendor, as part of the residency clinic’s transition to Cerner. The transition occurred in September of 2016, 3 months prior to the start of our study period.
Study Design and Data Collection
The institutional review board reviewed this research and granted exemption from formal review. Our cross-sectional study took place at the family medicine residency continuity clinic of a large, urban academic medical center. We collected and analyzed time spent in the electronic health record by family medicine physicians over a 6-month period (January 2017 through June 2017) using Cerner Advance, a web-based application that collects and presents user specific usage data for time spent in the Cerner Electronic Health Record (Cerner Corp, Kansas City, MO), including time spent doing specific activities. EHR time was restricted to active time in the EHR associated with care in the ambulatory setting only. Active time is defined by Cerner Advance as three or more mouse clicks per minute, 15 or more keystrokes per minute, 1,700 or more mouse miles (pixels) per minute of mouse movement. After-hours use is defined as time spent between the hours of 6:00 pm and 6:00 am and on weekends. Primary data points collected included number of patients seen, total time per patient, and total time spent after hours. All resident patient encounters have an attributed supervising faculty physician. Therefore, we were unable to collect full data for faculty physicians. We analyzed data using MedCalc statistical software.
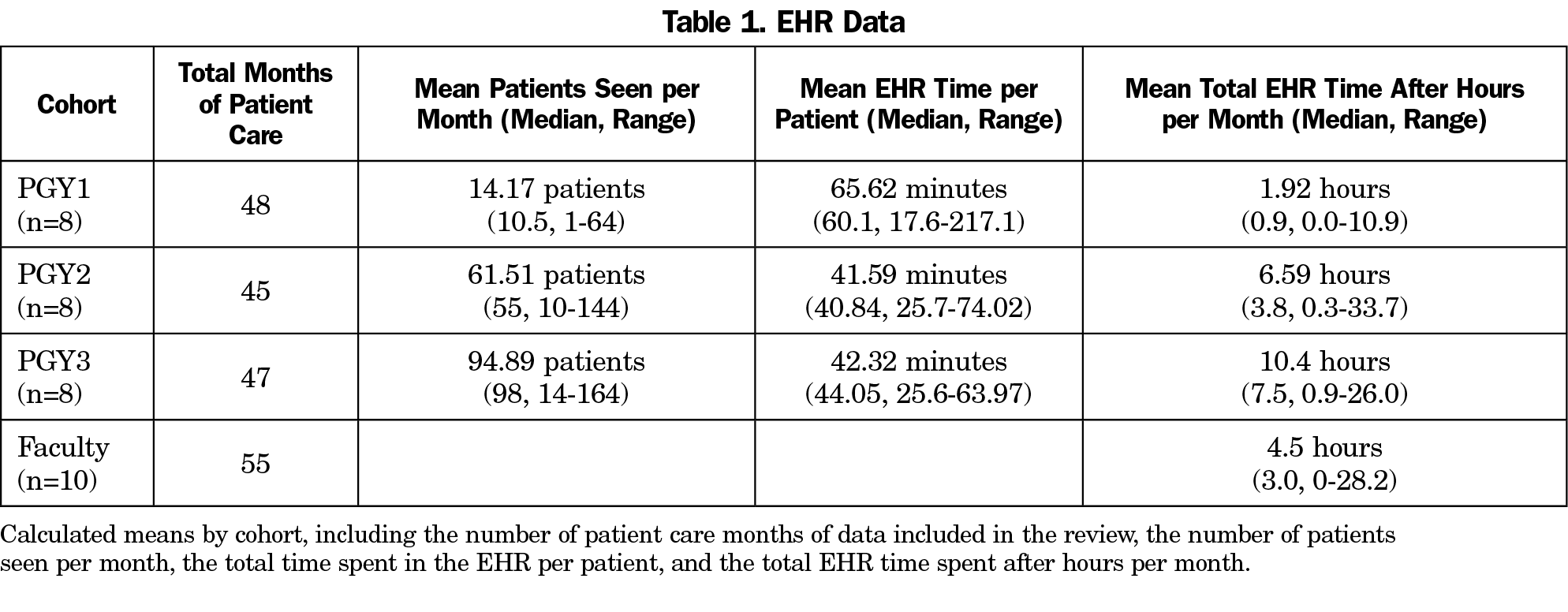
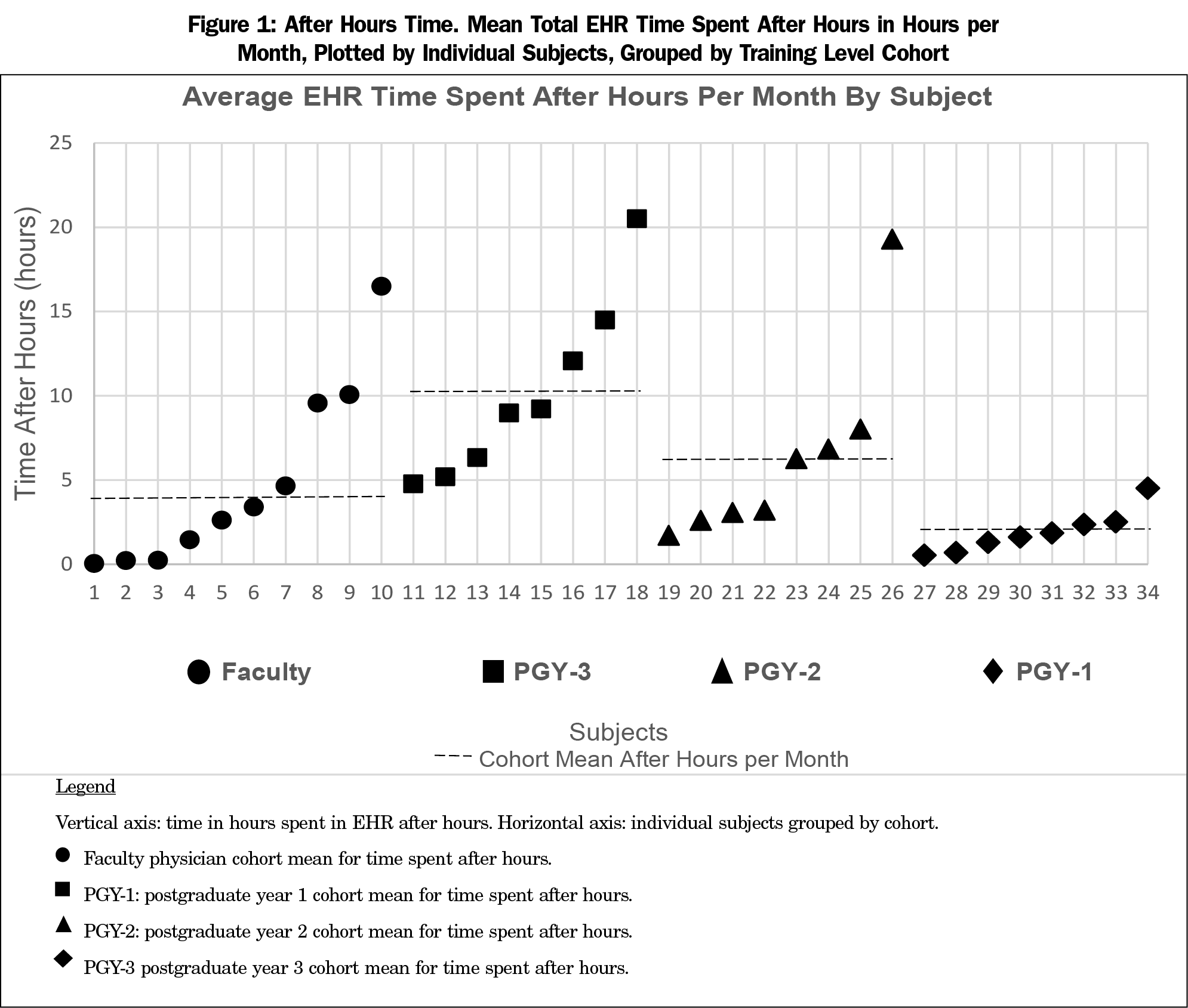
Table 1 shows the number of patients seen and EHR time for each cohort. Over the 6-month interval, time spent varied widely as shown in Figure 1. Total time after hours per month ranged from 0.9 to 26 hours within the postgraduate year-3 (PGY-3) cohort, from 0.3 to 33.7 hours within the PGY-2 cohort, and from 0 to 10.9 hours within the PGY-1 (postgraduate year-1) cohort.
The faculty cohort exhibited similar wide distribution: after-hours time ranged from 0 to 28.2 hours monthly.
EHR time data is accessible and informative. Family physicians spend a significant amount of time completing tasks in the EHR, including a large proportion after hours. EHR time varies widely: physician time spent in the EHR after normal work hours ranges from no time to over 33 hours per month. This variation continued regardless of level of training. Our objective measurement of EHR use provides insight into a pressing issue for the training and sustaining of the family physician workforce.
Our study has two major limitations: the limited ability to measure faculty EHR time and proximity of the study to an EHR transition. Current methods for monitoring time spent in the EHR do not allow us to differentiate between time a faculty physician spends precepting a resident’s patient versus a patient encounter completed on their own. We gathered data near an EHR transition, and while we allowed for 3 months of use prior to starting the retrospective collection, we suspect that improving efficiency has likely occurred.
Our study demonstrates that residency programs can quantify EHR time using a program embedded in Cerner. Additionally, marked variation in time spent after hours suggests opportunities to improve physician efficiency and decrease after-hours use. Residencies can identify physicians more likely to be overwhelmed by after-hours work and study personalized interventions to improve efficiency, decrease time spent after hours, and improve well-being.
Acknowledgments
The authors acknowledge the work and support of Sabrina Rocke, DO, University of Arizona College of Medicine Phoenix; Shari Pressley, MD, University of Arizona College of Medicine Phoenix; and Daniel Jones, Cerner Corp.
The content of this manuscript was presented as a poster presentation at the STFM Annual Spring Conference in May 2018, in Washington, DC.
References
- Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377-1385. https://doi.org/10.1001/archinternmed.2012.3199
- Bohman B, Dyrbye L, Sinsky C, Linzer M, Olson K, Babbott S, Murphy M, deVries P, Hamidi M, Trockel M. Physician Well-Being: The Reciprocity of Practice Efficiency, Culture of Wellness, and Personal Resilience. NEJM Catalyst http://catalyst.nejm.org/physician-well-being-efficiency-wellness-resilience/. Accessed April 22, 2019.
- Raj KS. Well-being in residency: A systematic review. J Grad Med Educ. 2016;8(5):674-684. https://doi.org/10.4300/JGME-D-15-00764.1
- Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc. 2014;21(e1):e100-e106. https://doi.org/10.1136/amiajnl-2013-001875
- Spinelli WM, Fernstrom KM, Britt H, Pratt R. “Seeing the patient is the joy:” a focus group analysis of burnout in outpatient providers. Fam Med. 2016;48(4):273-278.
- Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91(7):836-848. https://doi.org/10.1016/j.mayocp.2016.05.007
- Robertson SL, Robinson MD, Reid A. Electronic health record effects on work-life balance and burnout within the I3 population collaborative. J Grad Med Educ. 2017;9(4):479-484. https://doi.org/10.4300/JGME-D-16-00123.1
- Chen L, Guo U, Illipparambil LC, et al. Racing against the clock: internal medicine residents’ time spent on electronic health records. J Grad Med Educ. 2016;8(1):39-44. https://doi.org/10.4300/JGME-D-15-00240.1
- Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(5):419-426. https://doi.org/10.1370/afm.2121
- Young RA, Burge SK, Kumar KA, Wilson JM, Ortiz DF. A Time-Motion Study of Primary Care Physicians’ Work in the Electronic Health Record Era. Fam Med. 2018;50(2):91-99. https://doi.org/10.22454/FamMed.2018.184803
- Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165(11):753-760. https://doi.org/10.7326/M16-0961



There are no comments for this article.