Background and Objectives: In Kenya, little data exists on point-of-care ultrasound (POCUS) training and use for family medicine physicians. In 2017, a 3-day POCUS workshop assembled most of the family medicine physicians in Kenya. Through surveys, we assessed how this workshop could affect the level of POCUS use, skill, and confidence in family medicine practitioners in the long term.
Methods: Structured surveys, distributed before, after, and 10 months postworkshop assessed demographics, POCUS use, barriers, comfort, and skills based on attendee self-assessment. We compared data from the preworkshop surveys to postsurveys and post-postsurveys to assess immediate and long-term differences. Wilcoxon signed-rank test was used to evaluate continuous data, and significance was based on a P value of <.05.
Results: The proportion of participants who self-reported using POCUS increased significantly between presurvey and post-postsurvey (29.7% to 63.2%, P=.0161). Mean confidence scores increased significantly from presurvey to postsurvey and post-postsurvey. For all body systems, self-reported mean skill scores increased significantly from presurvey to postsurvey and post-postsurvey. Lack of access to machines and mentorship are substantial barriers to increasing POCUS use.
Conclusions: This study highlights the utility of one-time POCUS training in increasing long-term POCUS uptake by participants. While encouraging, our findings also show barriers to increasing POCUS use. These barriers must be addressed, potentially through intradepartmental and interorganizational exchanges of resources to ensure that future POCUS workshops are successful in supporting POCUS use in Kenya.
Access to diagnostic imaging is a challenge in health facilities of low- and middle-income countries (LMICs). A 2011 World Health Organization (WHO) survey reported that the density of computerized tomography (CT) scans was 2.06 per million people in LMICs compared to 44.31 in high-income countries.1 As an alternative, point-of-care ultrasound (POCUS) use has recently increased in LMICs.2
POCUS is attractive for multiple reasons. Units are compact and operate with rechargeable batteries, minimal infrastructure and training are required, and diagnosis can be done solo at the bedside. The WHO stated that capital costs for the most advanced ultrasound machine were 10% of those for a CT machine.3 Although quality evidence is lacking, a systematic review demonstrated that portable ultrasound may have a clinical impact in up to 70% of cases.2
In Kenya (an LMIC), family physicians are well situated to utilize POCUS in multiple settings yet lack formal training. In 2017, the Kenya Association of Family Physicians (KAFP) organized a 3-day training in collaboration with Moi, Aga Khan, Kenyatta, and Kabarak Universities, as well as the Contra Costa, University of Massachusetts, and Brown University family medicine (FM) residency programs. Contra Costa FM has been conducting POCUS workshops for over 5 years4 with a course based on American College of Emergency Physician Guidelines. Our study aimed to assess the immediate and long-term (10-month) impact of an adapted version of this course on POCUS use, confidence, and skills for FM trainees and faculty in Kenya.
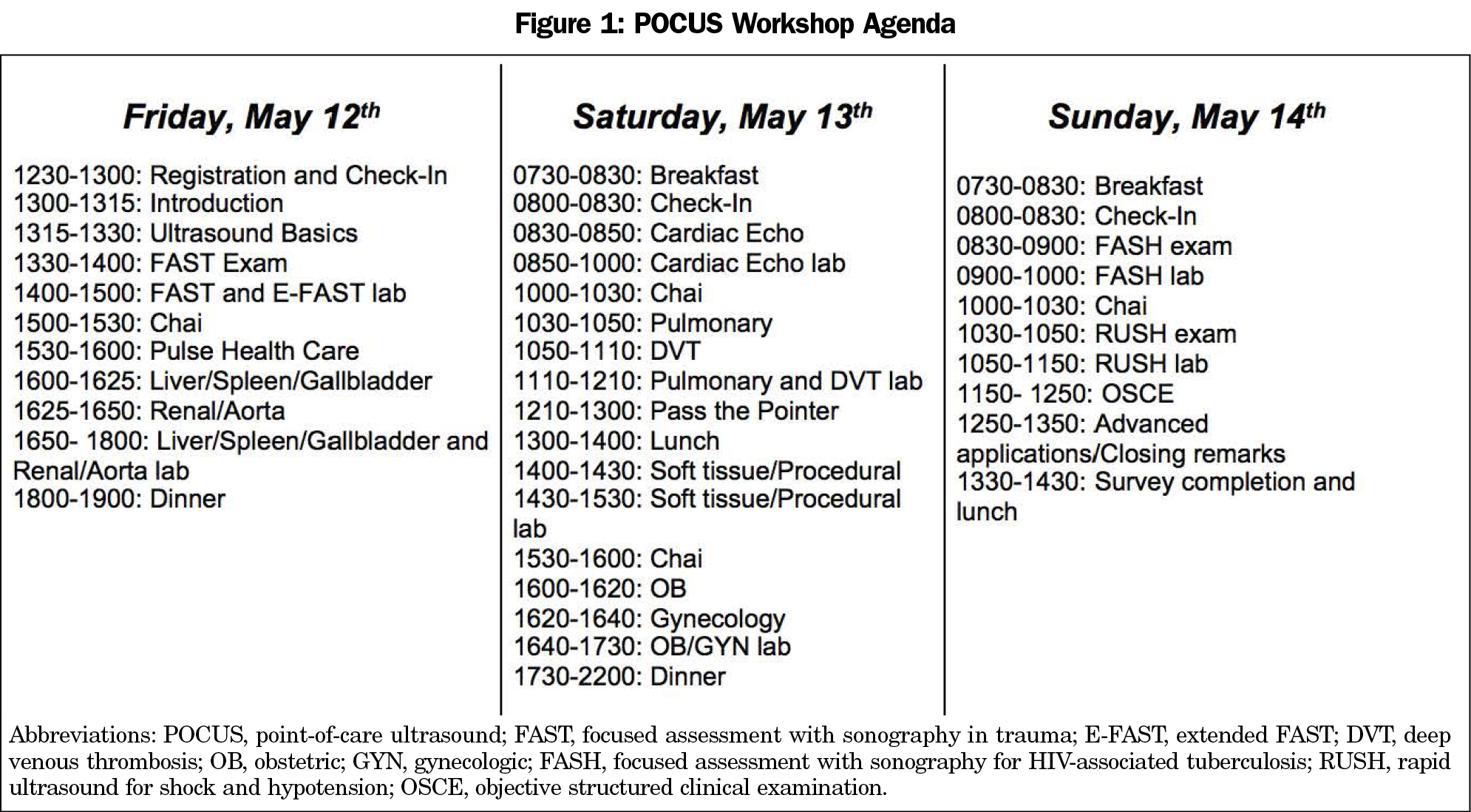
In May 2017, we conducted a 3-day POCUS course for all FM physicians and trainees in Kenya, with residents (registrars) and faculty (consultants) from four out of five FM residency programs attending. The course comprised lectures, large-group demonstrations, and hands-on scanning. See Figure 1 for course agenda.
We distributed pre- and poststructured surveys before and immediately after the workshop, and 10 months postworkshop (Appendix 1). Question types included multiple choice, open-ended, and Likert scale.
Surveys were anonymous but linked by a unique identifier. A single investigator (L.J.) entered all data into a Microsoft Excel (version 1901) spreadsheet and used Wilcoxon signed-rank test to evaluate continuous data. Significance was based on a P value of <.05. Statistical analysis was performed using Stata/IC 15.
The University of Massachusetts Institutional Review Board reviewed the project and determined that it was not human subjects research given that this was a program evaluation and survey data was anonymous.
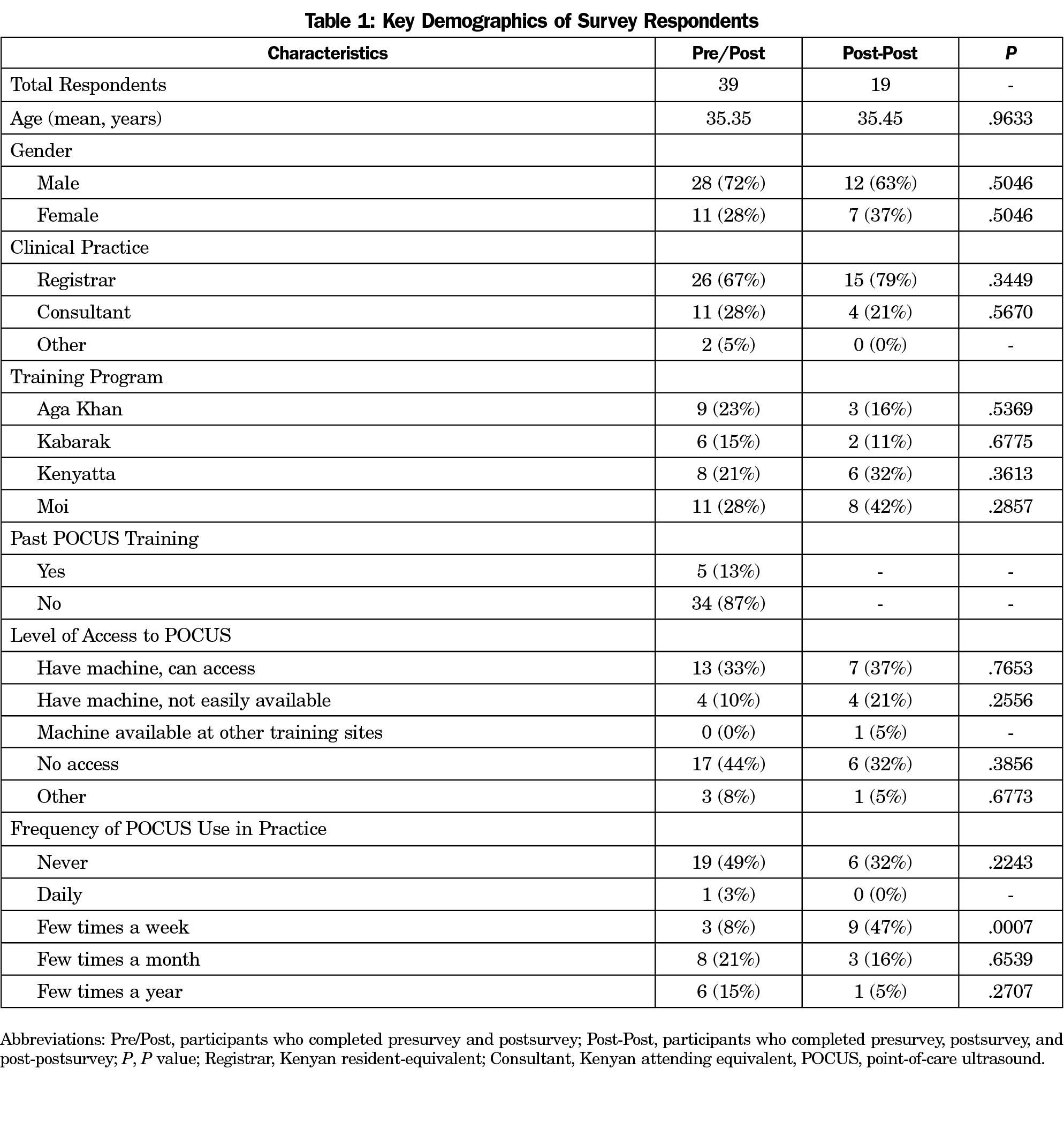
Of 41 participants, 39 completed the surveys and were included in pre/post analysis. Of these participants, 28 (72%) were male and 11 (28%) were female; 26 (67%) were registrars; 34 (87%) reported never having POCUS training previously. Twenty (51%) participants completed the 10-month post-postsurvey, 19 (49%) of whom were matched to the original pre- and posttraining analysis and were included in post-post analysis (Table 1).
The three most cited barriers on presurvey were cost of machine, insufficient training, and lack of formal POCUS curriculum (Figure 2). The proportion of respondents who cited lack of training as a barrier to POCUS use decreased significantly from presurvey to postsurvey (47.37% to 5.13%, P=.00000) and from presurvey to post-postsurvey (47.37% to 15.79%; P=.0198). The proportion of participants who self-reported using POCUS increased significantly between presurvey and post-postsurvey (29.7% to 63.2%; P=.0161).
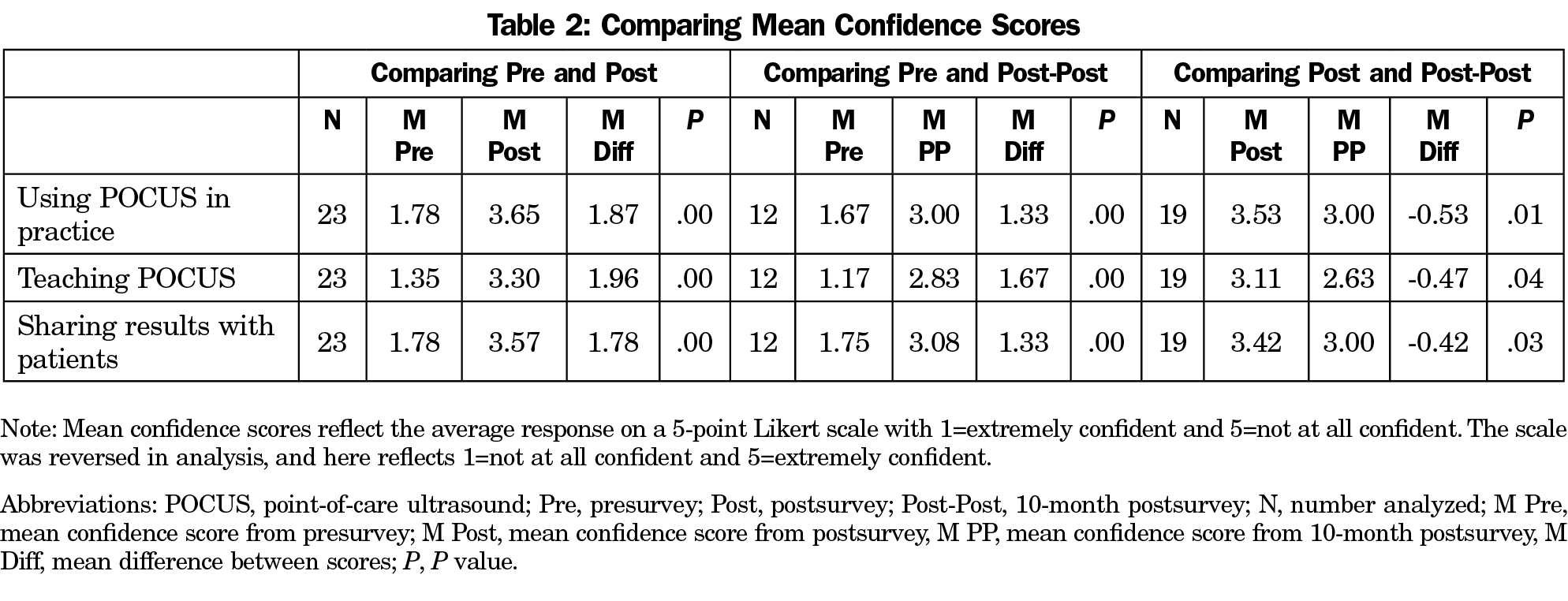
Participants rated their confidence in using POCUS in practice, teaching POCUS, and sharing POCUS findings with patients. For all three questions, mean confidence score increased significantly from presurvey to postsurvey, and from presurvey to post-postsurvey, but decreased significantly from postsurvey to post-postsurvey (Table 2).
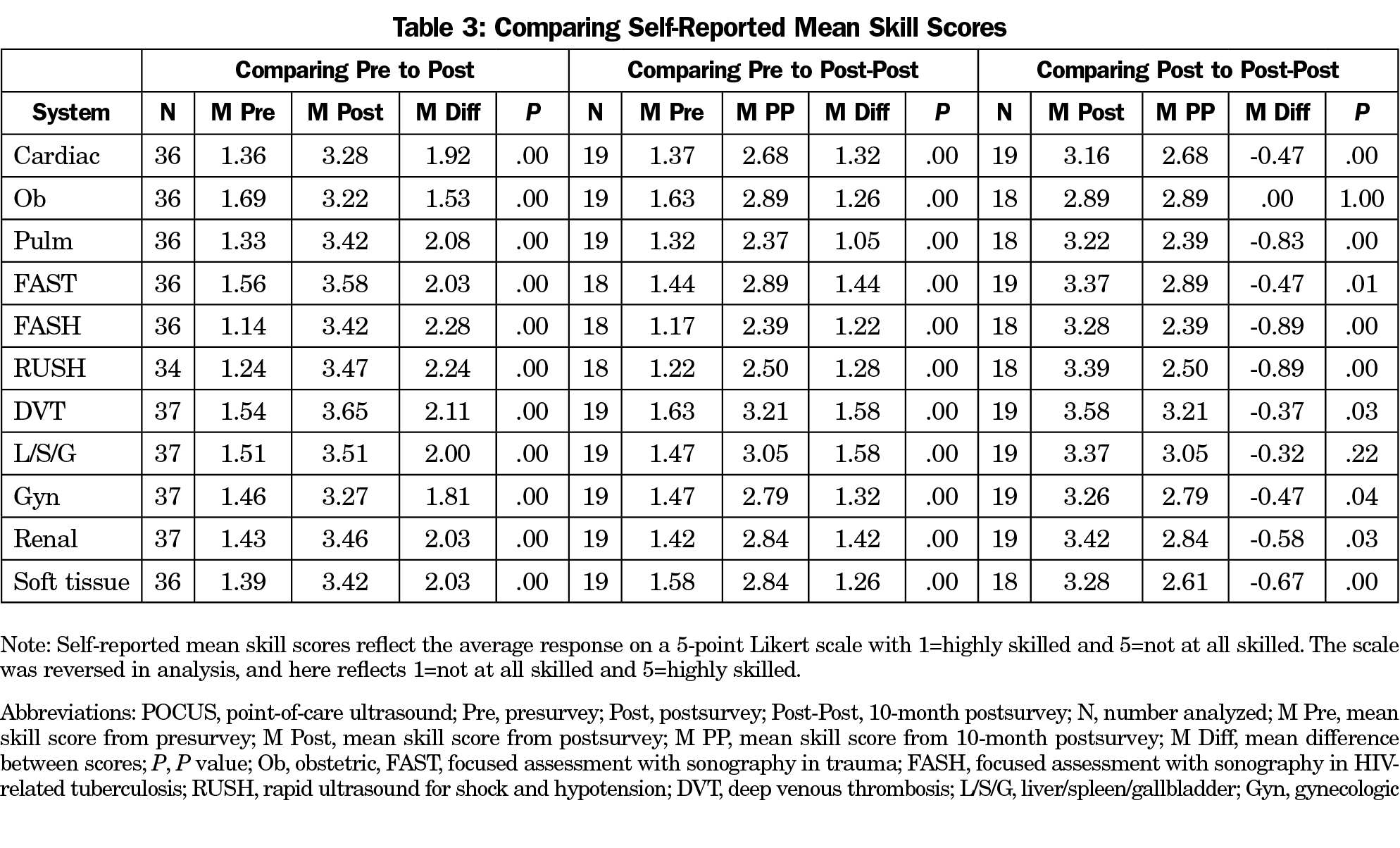
For all body systems, self-reported mean skill scores increased significantly from presurvey to postsurvey, and from presurvey to post-postsurvey. Self-reported mean skill scores decreased significantly across all body systems from postsurvey to post-postsurvey, except for obstetric and liver/spleen/gallbladder (Table 3).
Considering the potential of POCUS use by FM physicians in Kenya, it is necessary to determine whether training modalities such as short workshops are effective. Our findings show that self-reported use, skills, and confidence with POCUS increased significantly after a short workshop and that this increase, while declining slightly after 10 months, remained significantly elevated from preworkshop levels. This highlights the utility of one-time, basic POCUS training in increasing long-term POCUS uptake by participants and confirms findings of previous studies.5,6 The workshop played a key role in addressing the lack of training that was noted by most trainees as a barrier in the presurvey and in other studies.7
Our study was one of the first to assess perceived barriers to POCUS use in an LMIC 10 months after a POCUS workshop, allowing insight into the reasons for the decline in skills and confidence over that period. Lack of ready access to a machine was the most commonly cited barrier to POCUS use. Ultrasound devices, while relatively inexpensive, remain cost prohibitive in LMICs.8,9 Nongovernmental organizations are distributing POCUS machines to rural health care facilities across the country, but full coverage to all facilities is yet to be realized.
The other commonly cited barrier related to lack of continuous, onsite POCUS training. Although faculty attended the workshop, they were also in the learning stages. Collaborations among departments and other institutions both nationally and internationally could provide opportunities for such mentorship.
This study has several strengths. Our workshop marked the first time that most Kenyan FM physicians and trainees were gathered together, and our survey results provide new insight into the state of the field of family medicine in Kenya. Additionally, our 10-month post-postsurvey assessed the impacts of the workshop over time, suggesting that although uptake remains increased compared to preworkshop levels, future workshops must facilitate machine donations and foster accessible teaching relationships to promote sustainability.
Acknowledgments
Study findings were presented at the STFM Annual Spring Conference, May 7, 2018, Washington, DC, as an oral presentation entitled “On The Same Wavelength: Assessing a Cross-Cultural POCUS Workshop in Kenya.”
Financial Support: The 2017 POCUS Workshop was partially funded by Pulse Healthcare Limited.
References
- Velazquez-Berumen A. WHO Perspectives on Health Technologes: Medical Imaging. Presentation 2011 Annual Meeting of European Society of Radiology. Vienna, Austria; March 4, 2011.
- Becker DM, Tafoya CA, Becker SL, Kruger GH, Tafoya MJ, Becker TK. The use of portable ultrasound devices in low- and middle-income countries: a systematic review of the literature. Trop Med Int Health. 2016;21(3):294-311. https://doi.org/10.1111/tmi.12657
- Future use of new imaging technologies in developing countries. Report of a WHO Scientific Group. World Health Organ Tech Rep Ser. 1985;723:1-67.
- Jayasekera NB, Point of Care Ultrasound (POCUS) at Contra Costa. https://cchealth.org/residency/ghf/pocus.php#resources. Accessed July 12, 2018.
- Henwood PC, Rempell JS, Liteplo AS, et al. Point-of-care ultrasound use over six-month training period in Rwandan district hospitals. Afr J Emerg Med. 2013;3(4)(suppl):S5-S6. https://doi.org/10.1016/j.afjem.2013.08.010
- Wanjiku GW, Bell G, Wachira B. Assessing a novel point-of-care ultrasound training program for rural healthcare providers in Kenya. BMC Health Serv Res. 2018;18(1):607. https://doi.org/10.1186/s12913-018-3196-5
- Shah S, Bellows BA, Adedipe AA, Totten JE, Backlund BH, Sajed D. Perceived barriers in the use of ultrasound in developing countries. Crit Ultrasound J. 2015;7(1):28. https://doi.org/10.1186/s13089-015-0028-2
- Sue K. The occasional ED ultrasound: focused assessment with sonography for trauma (FAST). Can J Rural Med. 2015;20(1):33-39.
- Blois B. Office-based ultrasound screening for abdominal aortic aneurysm. Can Fam Physician. 2012;58(3):e172-e178.
- Moore DE Jr, Green JS, Gallis HA. Achieving desired results and improved outcomes: integrating planning and assessment throughout learning activities. J Contin Educ Health Prof. 2009;29(1):1-15. https://doi.org/10.1002/chp.20001




There are no comments for this article.