Background and Objectives: Academic medical centers (AMC) are among some of the most expensive places to provide care. One way to cut costs is by decreasing unnecessary referrals to specialists for procedures that can be provided by well-trained primary care physicians. Our goal is to measure the financial impact of an office-based minor procedure service driven entirely by family physicians.
Methods: We examined claims data for procedures performed on patients insured under our AMC’s home-grown accountable care organization-style health plan (Stanford Health Care Alliance [SHCA]). Descriptive statistics was used to compare the volume and cost of procedures performed by family medicine (FM) versus specialty care (SC). We preformed a subanalysis of SC procedures to explore the degree to which consultation and facility fees increased costs for SC. We used mathematical modeling to estimate the impact on cost of care if procedures were shifted from SC to FM and to calculate a return on investment (ROI).
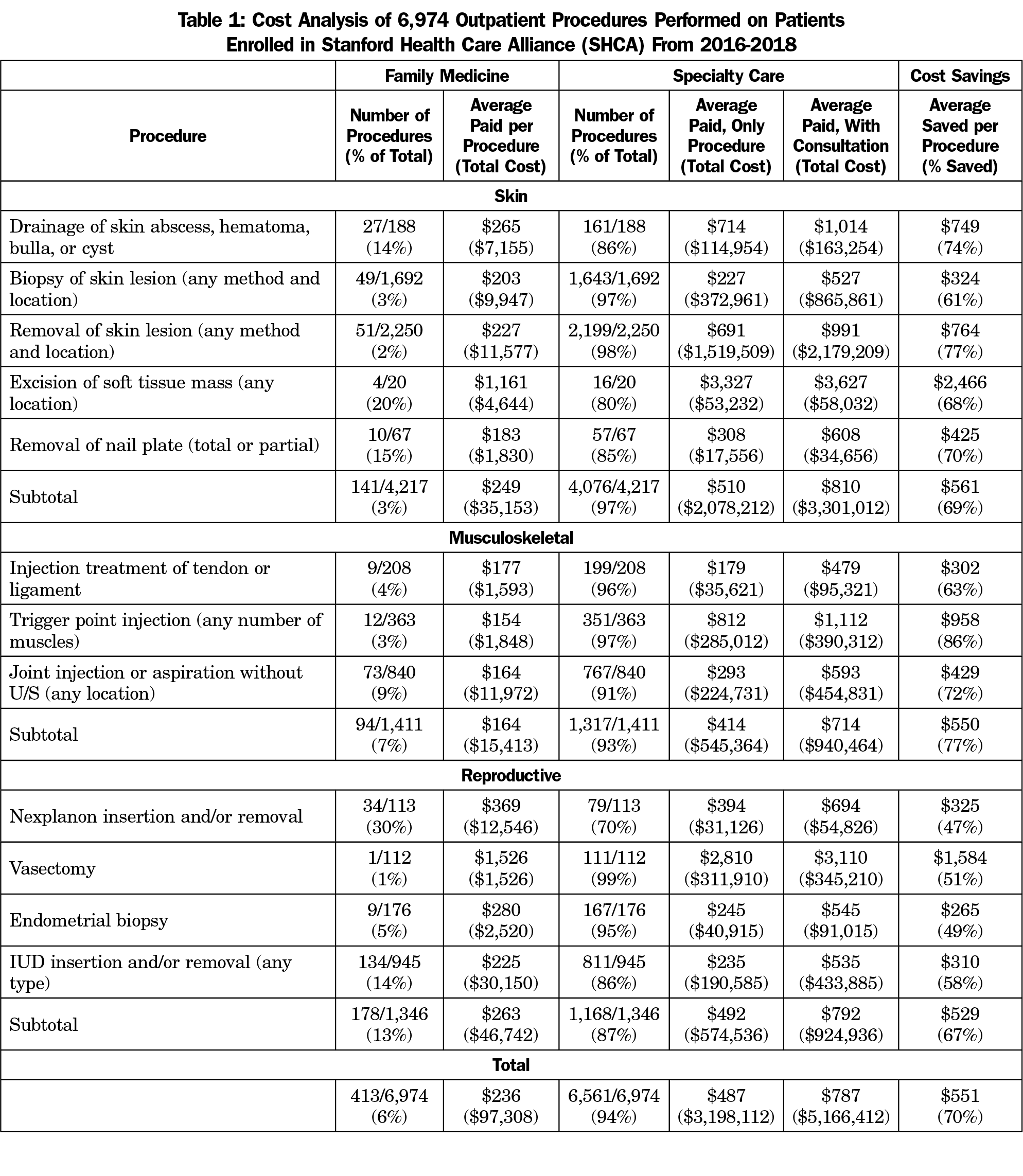
Results: Our data set examined 6,974 outpatient procedures performed on SHCA patients from 2016-2018 at a cost of $5,263,720 to SHCA. FM performed 6% of procedures at an average cost of $236 per procedure, while SC performed 94% of procedures at an average cost of $787 per procedure. FM saved money for all 12 types of skin, musculoskeletal, and reproductive procedures assessed; the average saved per procedure was $551. This represents a 70% cost savings. ROI was 2.33; for every $1 spent on FM procedures, SHCA saved $2.33.
Conclusion: A family medicine minor procedure service significantly lowered health spending at our AMC.
Health care costs in the United States are rising faster than inflation and are estimated to reach 19% of the gross domestic product by 2027.1 Among health systems, academic medical centers (AMCs) are some of the most expensive places to provide care.2-5 Known for their contributions to education and research, AMCs are now being challenged to place equal emphasis on patient care and drive down costs.6 One way to cut costs is by decreasing unnecessary referrals to specialists for health services that could be safely and effectively provided by well-trained primary care physicians.7-8 Family physicians are trained in a wide range of office-based procedures, and more than 60% of practicing family physicians perform procedures.8-9
Launched in 2015, the Stanford Family Medicine Minor Procedure Service is a program run by six family physicians designed to decrease unnecessary subspecialty referrals for office-based minor procedures within Stanford University’s network of primary care clinics. The program accepts referrals from a pool of about 80 primary care providers in 10 clinics across Stanford’s service area in Northern California. Patients referred to the service by their primary care providers are seen within 1 week and do not require a separate visit for consultation as is customary for specialty referrals. In this way, it is an open access procedure service driven by family physicians. The objective of this study was to measure the impact of this program on the cost of care provided to a subset of patients who are insured under Stanford’s home-grown accountable care organization (ACO)-style health plan, using claims data to compare family medicine against specialty care.
Data Source
Stanford Health Care Alliance (SHCA) is a select network health plan for Stanford University employees, postdoctoral scholars, medical staff, and few local large-group employers. SHCA is administered by Aetna and had 38,000 enrollees in 2019. Its family medicine (FM) and specialty care (SC) providers are employed by Stanford. We obtained claims data for procedures performed on SHCA patients from January 1, 2016 to December 31, 2018 using a list of 63 current procedural terminology (CPT) codes (see Appendix A). The data set included number of procedures, amount paid per procedure by SHCA, specialty of provider performing the procedure (FM vs SC), and where the procedure was performed (office vs hospital outpatient, [HO]). HO is an outpatient clinic that is considered a part of the hospital—a designation that incurs an extra facility fee. Data is from ambulatory clinics only and excludes the emergency department and outpatient surgical centers; it also excludes any follow-up visits and equipment costs (except if part of HO fees).
Data Analysis
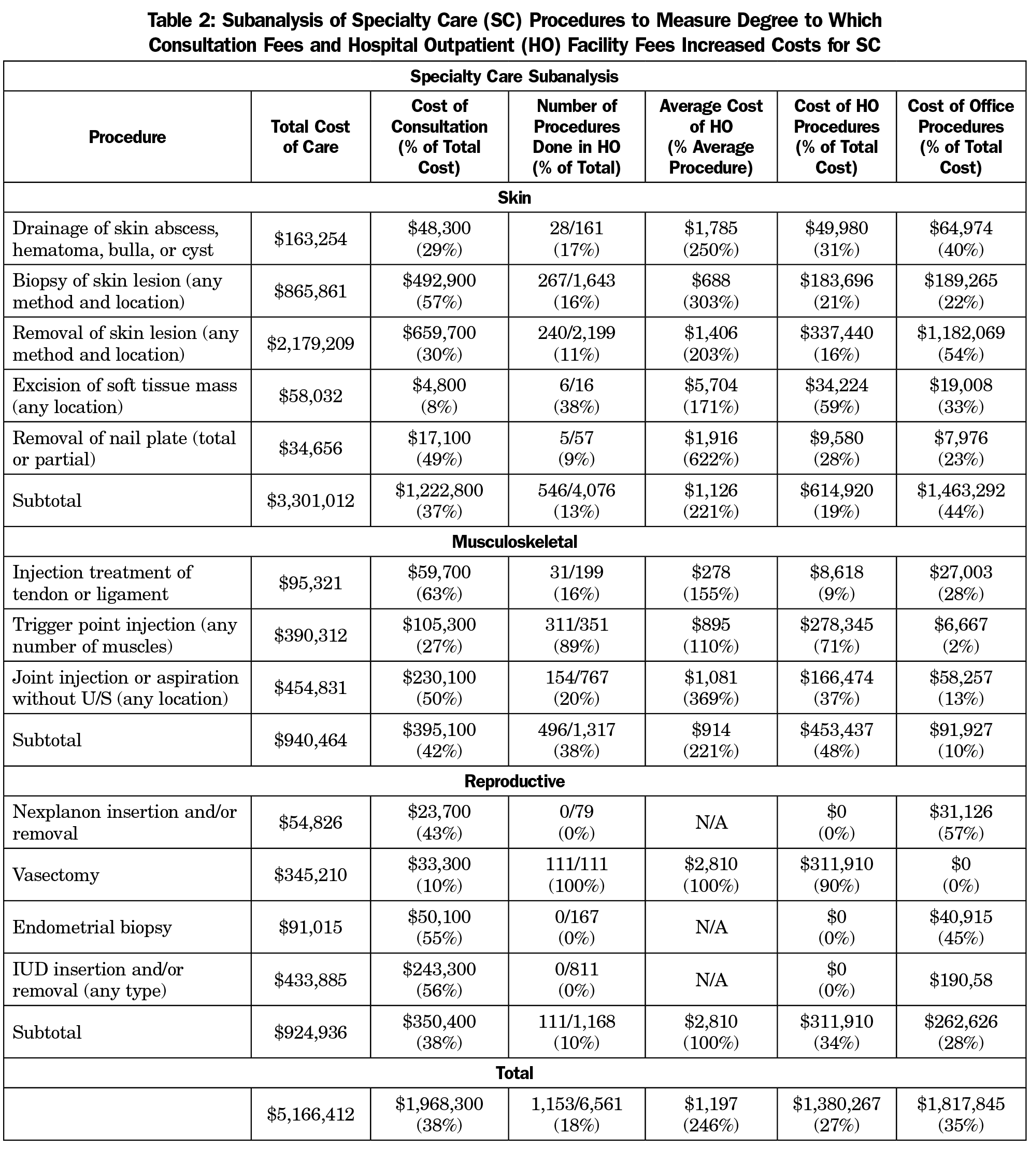
Descriptive statistics was used to measure differences in cost between FM and SC procedures across all categories. A subanalysis of SC procedures was done to explore the degree to which consultation fees and HO facility fees increased costs for SC. The average consultation fee per procedure was estimated to be $300 across all specialties based on paid claims, using the CPT codes 99242-25 and 99243-25. We performed mathematical modeling to estimate the impact on total cost of care if the proportion of procedures performed by FM relative to SC was adjusted.
The Stanford University Institutional Review Board exempted this study.
Our data set examined 6,974 outpatient procedures performed on SHCA patients from 2016-2018 at a cost of $5,263,720 to SHCA. FM performed 6% of procedures at an average cost of $236 per procedure, while SC performed 94% of procedures at an average cost of $787 per procedure. FM saved money for all 12 types of skin, musculoskeletal, and reproductive procedures assessed; the average saved per procedure was $551—a 70% cost savings (Table 1).
Consultation fees accounted for 38% of the total cost of SC procedures (Table 2); however, even without consultation, the average SC procedure was still more than twice as costly as FM (Table 1). While FM performed all procedures in the office, SC performed 18% of its procedures in the HO setting. These HO procedures cost 246% above average and accounted for 27% of SC costs.
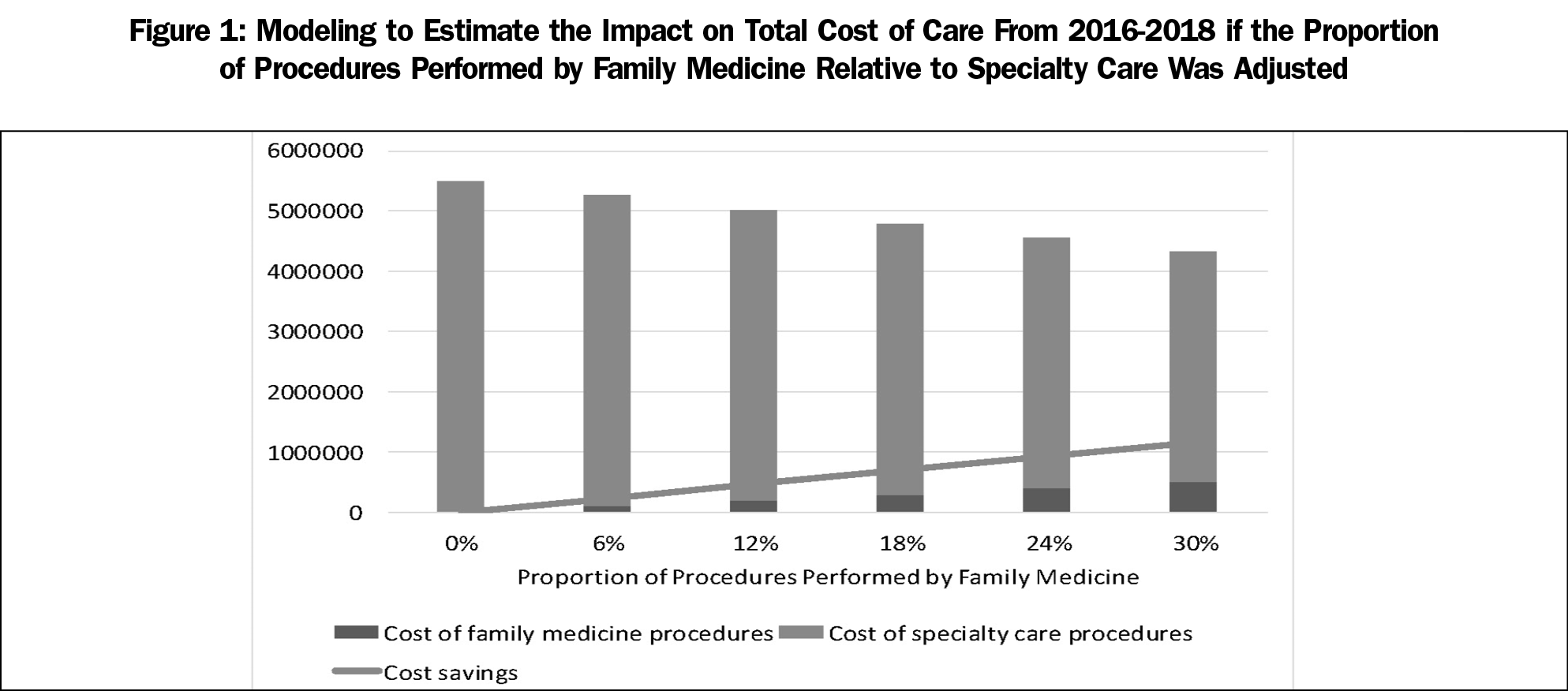
Our modeling shows that for every 6% shift in procedural volume from SC to FM, SHCA would save approximately $240,000 (Figure 1). If FM performed one in four procedures, SHCA would save $1 million over 3 years. The calculated return on investment (ROI) was 2.33.
As the United States pivots toward value-based care, new models of care delivery need to be explored that decrease costs while improving quality of care.10 To our knowledge, this is the first study to measure the financial impact of an intentionally designed, office-based procedure referral service driven entirely by family physicians. Our data shows the potential for significant cost savings for ACO-style and capitated health plans; even with a program that is very modest in size, the ROI is considerable: for every dollar spent on FM procedures, SHCA saved $2.33.
The biggest driver of cost savings for the minor procedure service was eliminating the need for a separate consultative visit through an open access design. The second-greatest driver of savings was avoiding the high HO facility fees that were charged in almost one in five procedures done by SC providers, who are more likely to work in clinics that are considered part of the hospital system—especially at AMCs. Our experience suggests that diverting procedures away from the hospital to FM offices lowers costs, particularly if those practices are organized around a shared service that reduces visits.
Our results are in consistent with prior research that has demonstrated cost savings when minor procedures are provided in the primary care setting.11-14 Although outside the scope of this study, other studies have shown that patients are more satisfied and have shorter wait times when minor procedures are performed by primary care physicians rather than specialists.11-15
Limitations
Our study was performed at a single AMC, so the results may not be generalizable to other health systems. We examined claims data from a single insurer, which may not reflect actual cost savings for other health plans; for example, facility fees and procedure costs may vary depending on negotiated fee structures. We estimated consultation fees based on paid claims to the best of our abilities, since this data was not readily available. Lastly, our data did not allow us to identify if SC procedures were more complex than FM’s, and whether patient outcomes and complication rates differed between FM and SC.
A family medicine minor procedure service significantly lowered health spending at our AMC. Future research should explore the impact of such programs on quality of care, patient experience, joy of practice, education, and workforce development for family physicians.
Acknowledgments
The authors thank all the physicians and staff who have contributed to the Stanford Family Medicine Minor Procedure Service. The authors also thank Dr Megan Mahoney and Dr Sang Chang for supporting the development and expansion of this program over the years.
References
- Sisko AM, Keehan SP, Poisal JA, et al. National health expenditure projections, 2018-27: economic and demographic trends drive spending and enrollment growth. Health Aff (Millwood). 2019;38(3):491-501. https://doi.org/10.1377/hlthaff.2018.05499
- Newhouse JP. Accounting for teaching hospitals’ higher costs and what to do about them. Health Aff (Millwood). 2003;22(6):126-129. https://doi.org/10.1377/hlthaff.22.6.126
- Mechanic R, Coleman K, Dobson A. Teaching hospital costs: implications for academic missions in a competitive market. JAMA. 1998;280(11):1015-1019. https://doi.org/10.1001/jama.280.11.1015
- Taylor DH Jr, Whellan DJ, Sloan FA. Effects of admission to a teaching hospital on the cost and quality of care for Medicare beneficiaries. N Engl J Med. 1999;340(4):293-299. https://doi.org/10.1056/NEJM199901283400408
- The Commonwealth Fund. Leveling the Playing Field: Financing the Missions of Academic Health Centers. https://www.commonwealthfund.org/publications/fund-reports/1997/may/leveling-playing-field-financing-missions-academic-health. Published May 1, 1997. Accessed August 29, 2019.
- Nuckols T, Weingarten S, Priselac TM. What value-based payment means for academic medical centers. NEJM Catalyst. https://catalyst.nejm.org/value-based-payment-academic-medical-centers/. Published May 30, 2019. Accessed July 20, 2019.
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502. https://doi.org/10.1111/j.1468-0009.2005.00409.x
- Bazemore A, Petterson S, Peterson LE, Phillips RL Jr. More Comprehensive Care Among Family Physicians is Associated with Lower Costs and Fewer Hospitalizations. Ann Fam Med. 2015;13(3):206-213. https://doi.org/10.1370/afm.1787
- Coutinho AJ, Cochrane A, Stelter K, Phillips RL Jr, Peterson LE. Comparison of Intended Scope of Practice for Family Medicine Residents With Reported Scope of Practice Among Practicing Family Physicians. JAMA. 2015;314(22):2364-2372. https://doi.org/10.1001/jama.2015.13734
- Burwell SM. Setting value-based payment goals—HHS efforts to improve U.S. health care. N Engl J Med. 2015;372(10):897-899. https://doi.org/10.1056/NEJMp1500445
- O’Cathain A, Brazier JE, Milner PC, Fall M. Cost effectiveness of minor surgery in general practice: a prospective comparison with hospital practice. Br J Gen Pract. 1992;42(354):13-17.
- George S, Pockney P, Primrose J, et al. A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial. Health Technol Assess. 2008;12(23):iii-iv, ix-38.
- Lowy A, Brazier J, Fall M, Thomas K, Jones N, Williams BT. Minor surgery by general practitioners under the 1990 contract: effects on hospital workload. BMJ. 1993;307(6901):413-417. https://doi.org/10.1136/bmj.307.6901.413
- Brown JS, Smith RR, Cantor T, Chesover D, Yearsley R. General practitioners as providers of minor surgery—a success story? Br J Gen Pract. 1997;47(417):205-210.
- Arribas Blanco JM, Gil Sanz ME, Sanz Rodrigo C, et al. [Effectiveness of dermatologic minor surgery in the office of the family physician and patient satisfaction in relation with ambulatory surgery]. Med Clin (Barc). 1996;107(20):772-775.



There are no comments for this article.