Background and Objectives: As the opioid crisis worsens across the United States, the factors that impact physician training in management of substance use disorders become more relevant. A thorough understanding of these factors is necessary for family medicine residency programs to inform their own residency curricula. The objective of our study was to identify factors that correlate with increased residency training in addiction medicine across a broad sample of family medicine residencies.
Methods: We performed secondary analysis of a national family medicine residency program director survey conducted in 2015-2016 (CERA Survey PD-8). We obtained data from the Council of Academic Family Medicine Educational Research Alliance (CERA) Data Clearinghouse. We analyzed residency clinic site designation as a patient-centered medical home (PCMH), federally-qualified health center (FQHC), or both, for their correlation with faculty member possession of DEA-X buprenorphine waiver license, as well as required residency curriculum in addiction medicine.
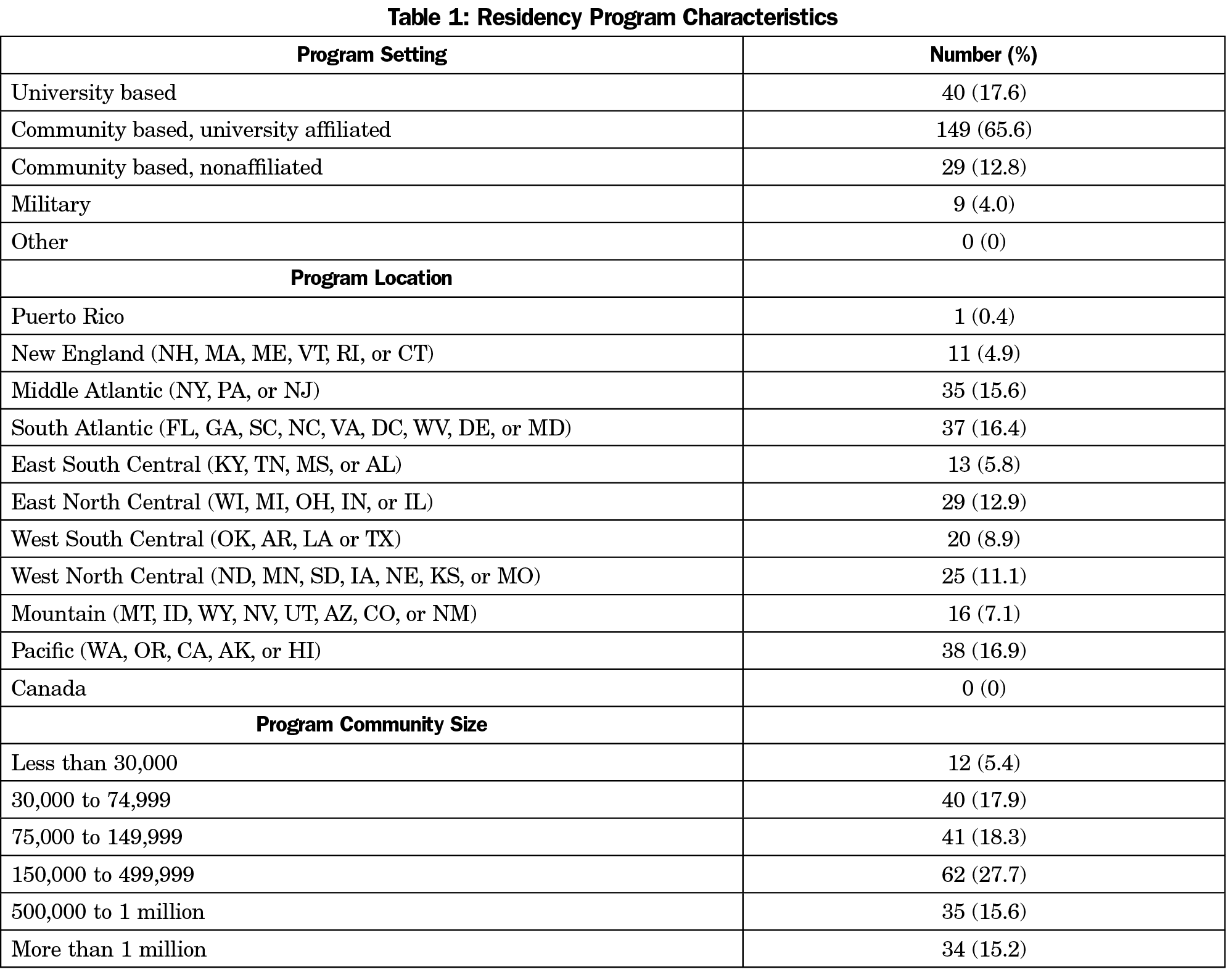
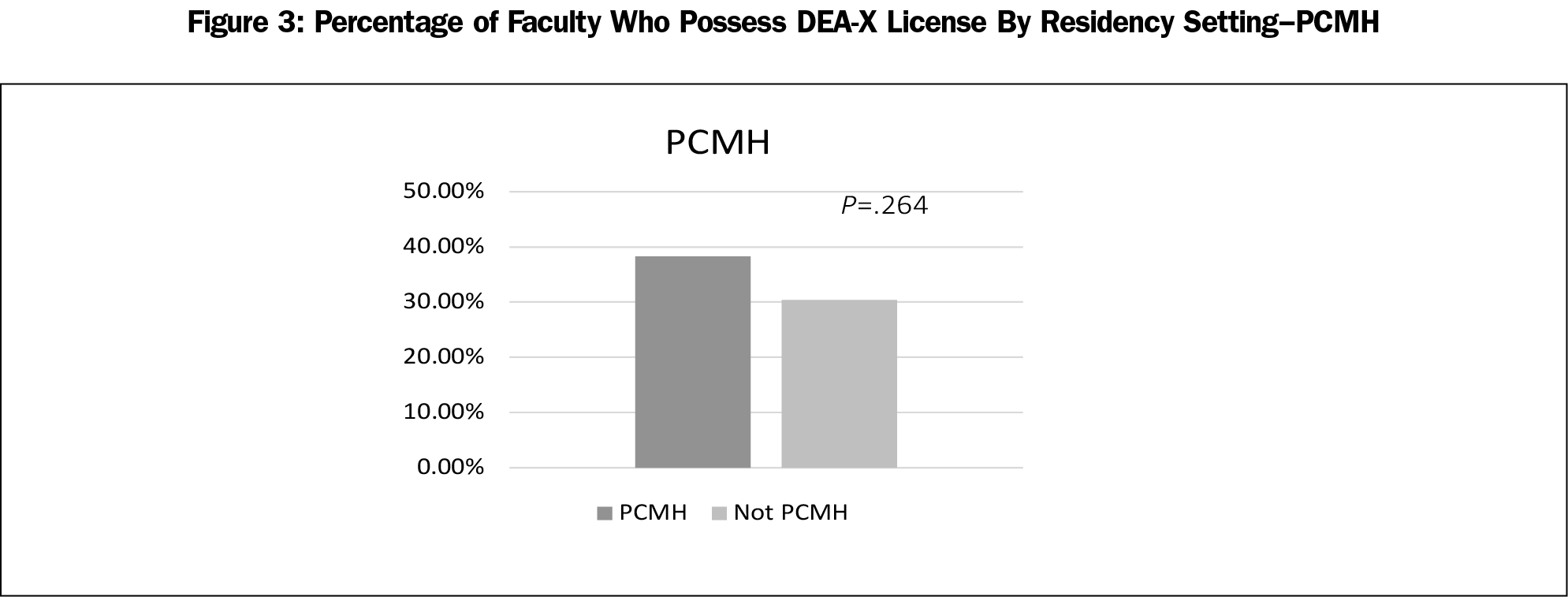
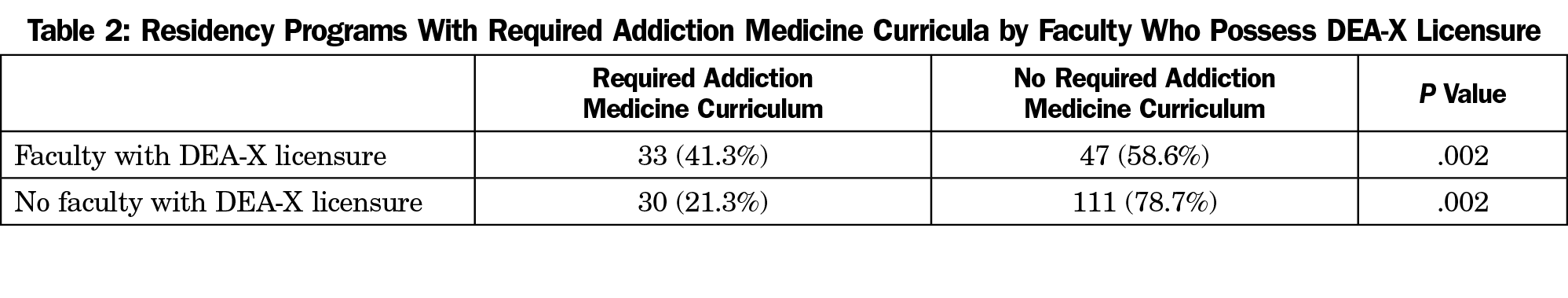
Results: Residency programs situated in an FQHC were more likely to have faculty members who possessed DEA-X buprenorphine waiver licenses (P=.025). Residency clinics that were both a PCMH as well as an FQHC also correlated strongly (P=.001). Furthermore, residencies with faculty who possessed a DEA-X license were significantly more likely to have a required curriculum in addiction medicine (P=.002).
Conclusions: Our quantitative secondary analysis of CERA survey data of family medicine residency program directors revealed that resident training in addiction medicine is strongly correlated with both residency clinic setting (FQHC or FQHC/PCMH) as well as residency faculty possession of DEA-X licenses.
Death from opioids has increased significantly in the United States, from 8,050 in 1999 to 70,237 in 2017.1 In 2015, approximately 2 million individuals reported having a substance use disorder involving prescription opioids, and 600,000 reported a substance use disorder involving heroin. Medications for treating opioid use disorder (OUD) have been shown to be effective in decreasing opioid use and opioid-related mortality. However, many physicians do not prescribe these medications.
Physicians’ scope of practice is profoundly influenced by their training; thus residency training is important in training physicians to provide opioid use disorder treatment. Buprenorphine treatment is effective, however only 2.2% of US physicians have the required DEA-X waiver to be able to prescribe buprenorphine.2,3 In a study of psychiatry residents, 38.5% of residents that received buprenorphine training in residency continued to prescribe after residency, while zero respondents who had not received training in residency prescribed buprenorphine.4 A recent publication by Tong et al showed a strong correlation between residency training in buprenorphine and future prescribing of the medicine in practice.5 A survey of providers in California showed that physicians who completed an addiction medicine rotation during their training were more confident in providing care for those with substance use disorders.6
We propose that residencies located in federally-qualified health centers (FQHCs) as well as patient-centered medical homes (PCMHs) are more likely to provide substance use disorder training. PCMHs are more likely to offer interdisciplinary services, including counseling, and thus may be better able to support a variety of services including comprehensive substance use disorder treatment, while FQHCs are more likely to serve patients at risk of substance use disorders.7
Data were obtained from the publicly available Council of Academic Family Medicine Educational Research Alliance (CERA) Data Clearinghouse. CERA conducts biannual cross-sectional surveys of all US family medicine residency program directors. The second of two 2015 CERA omnibus surveys to family medicine residency directors included specific questions on addiction medicine.8 In this survey, 461 US family medicine residency program directors in the Association of Family Medicine Residency Directors (AFMRD) database received an email invitation to participate in the survey in December 2015 followed by two email reminders prior to the survey closing in February 2016. The data were made publicly available in May 2016 on the Society of Teachers of Family Medicine website. The American Academy of Family Physicians’ Institutional Review Board approved the project.
We analyzed data using STATA IC13 (College Station, TX); we used univariate statistics to describe residency characteristics and the outcomes of interest: presence of an addiction medicine curriculum and faculty member who possessed a DEA-X buprenorphine waiver license. We used bivariate statistics and χ2 analysis to describe and assess the association between residency practice characteristics and the outcomes of interest.
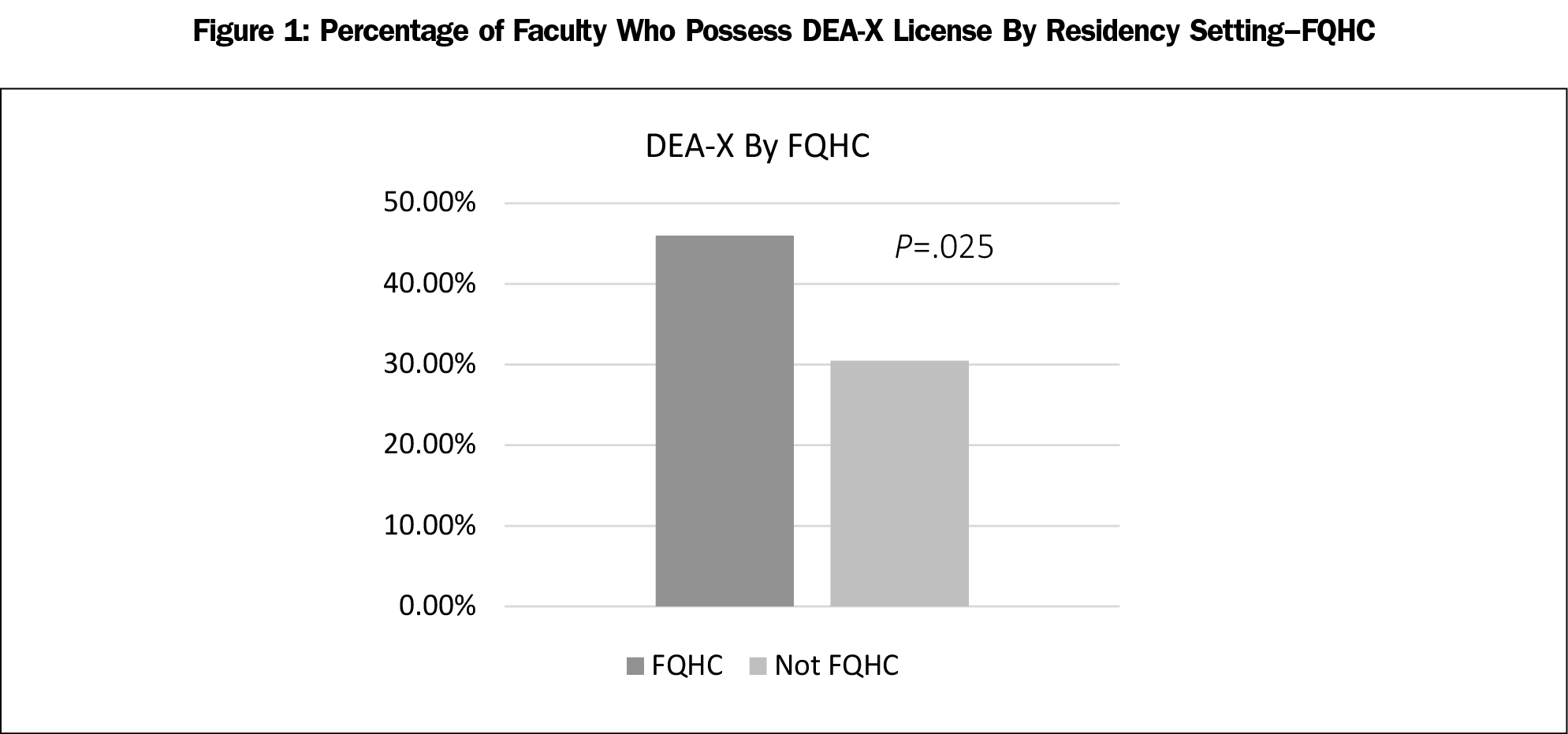
The CERA residency program directors’ survey had an overall response rate of 49.24% (227/461), with 99.5% of the respondents or 49.0% of the overall sample (226/461) answering the question about a required curriculum in addiction medicine. Table 1 shows further residency characteristics.
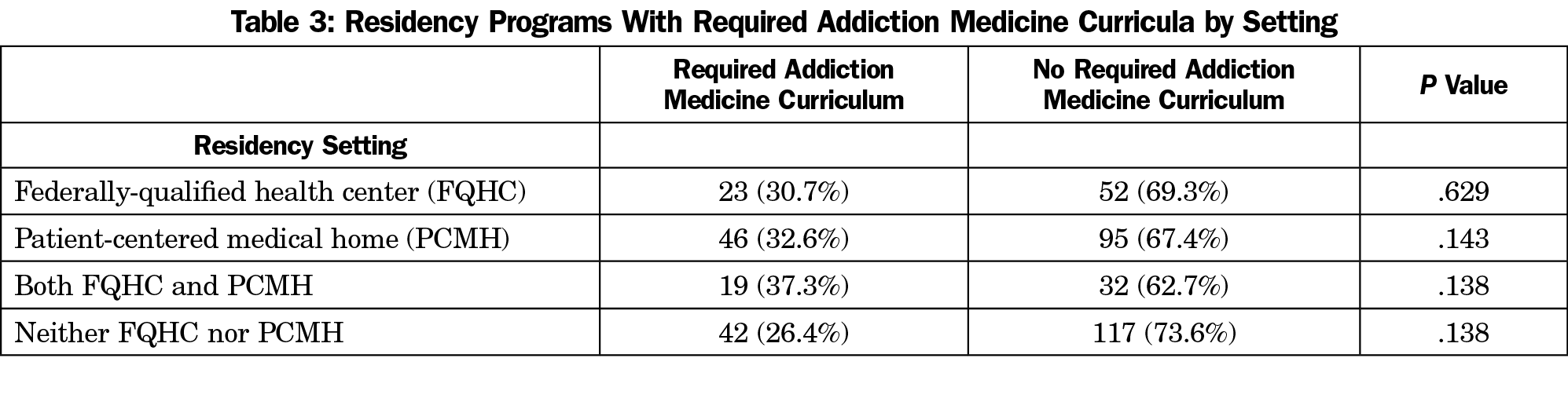
Residency programs situated in an FQHC were more likely to have at least one faculty member who possessed a DEA-X buprenorphine waiver license (P=.025); 45.9% of FQHCs reported having at least one such faculty member, while only 30.4% of non-FQHC residency clinics reported any faculty with DEA-X licenses (Figures 1-3). Although residencies with clinics designated a PCMH did not show a statistically significant association with faculty members having DEA-X licenses, clinics that were both a PCMH as well as an FQHC showed a significant association with having at least one faculty member who possessed a DEA-X license (P=.001). Results showed that 54.9% of programs with clinics designated both a PCMH and an FQHC reported faculty members who possess DEA-X licenses. Furthermore, residencies with faculty who possessed a DEA-X license were also significantly more likely to have a required addiction medicine curriculum (P=.002), with 41.3% of programs having such faculty licensure reporting required addiction medicine curricula, while only 21.3% of programs without such faculty licensure reported required curricula (Table 2). Residency location was not associated with faculty DEA-X licensure or presence of a required addiction medicine curriculum.
This study is the first to demonstrate that residency programs situated in an FQHC, in particular clinics designated both an FQHC as well as a PCMH, were more likely to have faculty members who possessed a DEA-X license. With the United States currently wracked by the opioid crisis, and with residents in many different specialties training in underserved areas that are hit particularly hard by this issue, it is clear that robust residency training in addiction medicine is a public health necessity.
We recognize from this analysis that residency setting is a strong indicator of training in addiction medicine and advocates for programs such as the Teaching Health Center Graduate Medical Education program as well as other community-based residency training programs. Although these survey data only represent family medicine residency programs, we expect that these data are applicable to other specialties that manage substance use disorders, such as internal medicine, pediatrics, OB/GYN, medicine/pediatrics, and psychiatry.
There are several limitations to this study. The CERA survey had a limited response rate (49.24%). The survey itself is of program directors and relies on their recall of certain facts that could potentially lead to inaccurate reporting of faculty DEA-X licensure. Furthermore, the details of a “required addiction curriculum” are not addressed and we expect there is likely a large degree of variation in the quality and quantity of training that residents receive.
This quantitative secondary analysis of CERA survey data of family medicine residency program directors revealed that family medicine resident training in addiction medicine is strongly correlated with both residency clinic setting (FQHC or FQHC/PCMH) as well as residency faculty possession of DEA-X licenses. Residency programs, not only in family medicine but all specialties, should research how they can increase appropriate and effective treatment of substance use disorders.
Acknowledgments
Presentation: This study was presented at the 2018 North American Primary Care Research Group (NAPCRG) Annual Meeting 2018, Chicago, IL.
References
- National Center for Health Statistics. NCHS Data Brief (Data Brief no. 329): Drug overdose deaths in the United States, 1999–2017. Published; 2018.
- Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014;(2):CD002207. https://doi.org/10.1002/14651858.CD002207.pub4
- Rosenblatt RA, Andrilla CH, Catlin M, Larson EH. Geographic and specialty distribution of US physicians trained to treat opioid use disorder. Ann Fam Med. 2015;13(1):23-26. https://doi.org/10.1370/afm.1735
- Suzuki J, Connery HS, Ellison TV, Renner JA. Preliminary survey of office-based opioid treatment practices and attitudes among psychiatrists never receiving buprenorphine training to those who received training during residency. Am J Addict. 2014;23(6):618-622. https://doi.org/10.1111/j.1521-0391.2014.12143.x
- Tong ST, Hochheimer CJ, Peterson LE, Krist AH. Buprenorphine Provision by Early Career Family Physicians. Ann Fam Med. 2018;16(5):443-446. https://doi.org/10.1370/afm.2261
- Reddy AT, Andersen RM, Gelberg L. Clinicians’ Beliefs and Practices Regarding Drug Use Care of Their Community Health Center Patients. J Addict Med. 2015;9(6):447-453. https://doi.org/10.1097/ADM.0000000000000158
- Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK. The de facto US mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993;50(2):85-94. https://doi.org/10.1001/archpsyc.1993.01820140007001
- O’Connor PG, Nyquist JG, McLellan AT. Integrating addiction medicine into graduate medical education in primary care: the time has come. Ann Intern Med. 2011;154(1):56-59. https://doi.org/10.7326/0003-4819-154-1-201101040-00008




There are no comments for this article.