Background and Objectives: For residents, uncertainty can be a source of motivation, interest, and stimulation, but it can also cause fear and anxiety that can lead to burn-out. Considering the prevalence of uncertainty in family medicine and the potential reactions from residents, reactions to uncertainty constitute an important research topic. This study sought to measure the evolution of reactions to uncertainty of family medicine residents in their first and second year, during a 6-month clinical rotation in a family physician’s office.
Methods: This study utilized a prospective epidemiological cohort design of first- and second-year family medicine residents during a 6-month clinical rotation in a family physician’s office during the 2018-2019 academic year. Data were collected at the beginning and end of the clinical rotation for the entire student population using the Physicians’ Reactions to Uncertainty (PRU) questionnaire.
Results: One hundred-two respondents were matched at the end of the clinical rotation and were included in the analysis. At baseline, there were no significant differences between first- and second-year residents in each dimension of the PRU. Anxiety due to uncertainty decreased significantly in residents of both years. Concern about bad outcomes decreased, but not significantly, in both years. Reluctance to disclose uncertainty to patients decreased in first-year residents.
Conclusions: During a 6-month clinical rotation, anxiety due to uncertainty decreased in first- and second-year residents. The frequency and the type of uncertain situations residents encountered could be investigated in future studies to better understand residents’ reactions to uncertainty.
Eric Beresford defined the source of uncertainty in medicine as inadequate resources in three types of knowledge: technical (inadequate technical or procedural knowledge), personal (not knowing patients’ wishes), or conceptual (difficulty applying abstract criteria to concrete situations).1
In family medicine, the care of patients of all ages with undifferentiated chronic and acute conditions, the position of family physicians as a patient’s first contact (a patient may consult with an early presentation of a clinical issue that can be incomplete), and the complexity of human pathologies make uncertainty inherent in daily practice.2-4
Family physicians consider uncertainty to be part of their identity.5 Uncertainty can be a source of motivation, interest, and stimulation.6-8 Uncertain situations permit a perpetual reflexivity in common practice and the avoidance of boredom. Uncertainty is also a way of avoiding overconfidence which could lead to medical errors.9
However, uncertainty can also be a source of fear and anxiety6-8 that can lead to burnout.10 A bad reaction to uncertainty, when associated with fear and anxiety, can lead to an increase in the prescription of complementary diagnostic tests associated with increasing patient charges.2,11,12
Family medicine residents are exposed to uncertainty from their first clinical rotation. In the same way physicians do, residents can have various reactions to uncertainty.
Facing uncertainty can be stimulating and motivate residents to learn the complex way of managing a consultation. Residents define uncertainty as part of their practice, especially when facing patients with chronic complex situations and/or complex environments.13
For those with bad reactions to uncertainty, however it could lead to difficulty, fear, and burnout.10,14,15
Considering the prevalence of uncertainty in family medicine and the potential bad reactions among residents, coping with uncertainty is an important learning outcome of medical training. The literature provides data on residents’ reactions to uncertainty in cross-sectional studies. Longitudinal studies could help to assess temporal trends in reactions to uncertainty during a clinical rotation.16
In France, residency in family medicine follows 6 years of medical school. All residency programs in France last 3 years and are based on (1) six clinical rotations of 6 months each, (2) 200 hours of teaching, and (3) formative evaluation. Residency programs are built on a competency-based approach to allow a progressive model of teaching.
Clinical rotations can occur in hospitals or in family physicians’ offices. Family medicine residents are first placed in an autonomous situation from their first year during a 6-month clinical rotation in a family physician medical office, supervised by a family physician. Residents conduct family medicine consultations under the direct supervision of a family physician 4 days per week. They can also carry out four to six consultations per day autonomously, under the indirect supervision of the supervising physician.
Two hundred hours of teaching in seminars or similar settings is centered on 11 situations defined by the French National College of Teachers of Family Physicians (Collège National des Généralistes Enseignants) as prevalent in family medicine: patients with chronic illnesses, patients with acute illnesses, children and adolescent health, sexual and reproductive health, couple and family issues affecting health, occupational health, medico-legal issues, management of difficult patients, social issues affecting health, and care of patients from others cultures.17 During this 6-month clinical rotation, theoretical teaching comprises six sessions of classroom training of 1 day each, none of which are specifically focused on uncertainty.
Residents also have a formative evaluation that includes, for every 6-month period: two written reports about complex clinical situations they have encountered (covering the biomedical, behavioral, and social backgrounds of the situation, their own reflections and the results of a narrative review); three mixed peer groups including first-, second-, and third-year residents. The formative evaluation is supervised by a family physician preceptor, who they meet three times in 6 months. The aim of the formative evaluation is to develop residents’ reflexivity.
This study explored two hypotheses: (1) the reaction to uncertainty will evolve positively during the course of a 6-month outpatient rotation, and (2) second-year residents, having already completed a 6-month outpatient rotation, will have a better reaction to uncertainty.
The objective of this study was to measure the evolution of reactions to uncertainty of first- and second-year residents during a 6-month clinical rotation in a family physician’s office.
This study utilized a prospective epidemiological cohort design of first- and second-year family medicine residents during a 6-month clinical rotation in a family physician’s office during the 2018-2019 academic year.
Study Population
The population studied consisted of family medicine residents registered in the faculty of medicine of Toulouse (Southwest France) during the 2018-2019 academic year, undergoing a 6-month clinical rotation in a family physician’s office. This population consisted in 81 first-year residents and 71 second-year residents.
Data Collection
Data were collected using the Physicians’ Reactions to Uncertainty (PRU) questionnaire.11 The French version of this questionnaire was validated with a population of residents.18 It comprises 15 items divided into four dimensions: anxiety due to uncertainty (five items), concern about bad outcomes (three items), reluctance to disclose uncertainty to patients (five items) and reluctance to disclose mistakes to physicians (two items). Each item is marked on a Likert scale from 1 to 6 (1: strongly disagree, 6: strongly agree). Following an analysis of the global score, we analyzed each dimension separately.
To evaluate the evolution from the baseline score, the cutoff points used were: low score (below 2 points), medium (between 2 and 4 points), and high score (between 4 and 6 points).
Data collection occurred in two phases for the whole of the population studied (first- and second-year residents). In a first phase the questionnaire was given on paper at the beginning of the clinical rotation (first month, November 2018) to the whole population, during two classroom sessions (one dedicated to first-year, one to second-year residents). In a second phase, the same population was sampled at the end of the clinical rotation (last month, April 2019) during a classroom session for the first-year residents, and during the choice of their next clinical rotation for the second-year residents. These two phases enabled measurement of the evolution during the clinical rotation of reactions to uncertainty in the two populations studied.
Date of birth was requested at the beginning of the questionnaire to match the first- and sixth-month data. Sex and study year were also requested.
Data Analysis
We performed a descriptive analysis for each item (mean, standard deviation, minimum, maximum, first quartile, third quartile). We performed this same analysis for each dimension, with the Cronbach a coefficients showing homogeneity of the items in each dimension (at the beginning of the clinical rotation: 0.91, 0.71, 0.63, and 0.86 respectively for each dimension; at the end of the clinical rotation: 0.85, 0.75, 0.76, and 0.86 respectively for each dimension).
We calculated evolution significance using the Wilcoxon rank-sum test. The analytic part enabled measurement of the correlation between certain dependent variables (sex, current year of residency) and the evolution of reactions to uncertainty. For results following a normal distribution, we calculated the correlation with a Student t test with a risk inferior to 5%. Results are expressed in points (+/- confidence interval), and calculations were made with the Microsoft Excel and SPSS software.
Ethics
This research study did not require the approval of an ethics committee in accordance with the March 5, 2012 legislation (law 2012-300 known as Jardé law) amended on June 16, 2012 (amendment 2016-800), as it consisted of a pedagogic study undertaken in the framework of training evaluation, students were informed about the study, its design, and anonymity was maintained.
Residents chose to participate and were allowed to decline or withdraw at any time without any explanation needed. The questionnaire requested no name or surname, and the only personal data collected was the date of birth. We did not perform cross-dating with the date of birth and the year of residency at any time.
Sampling
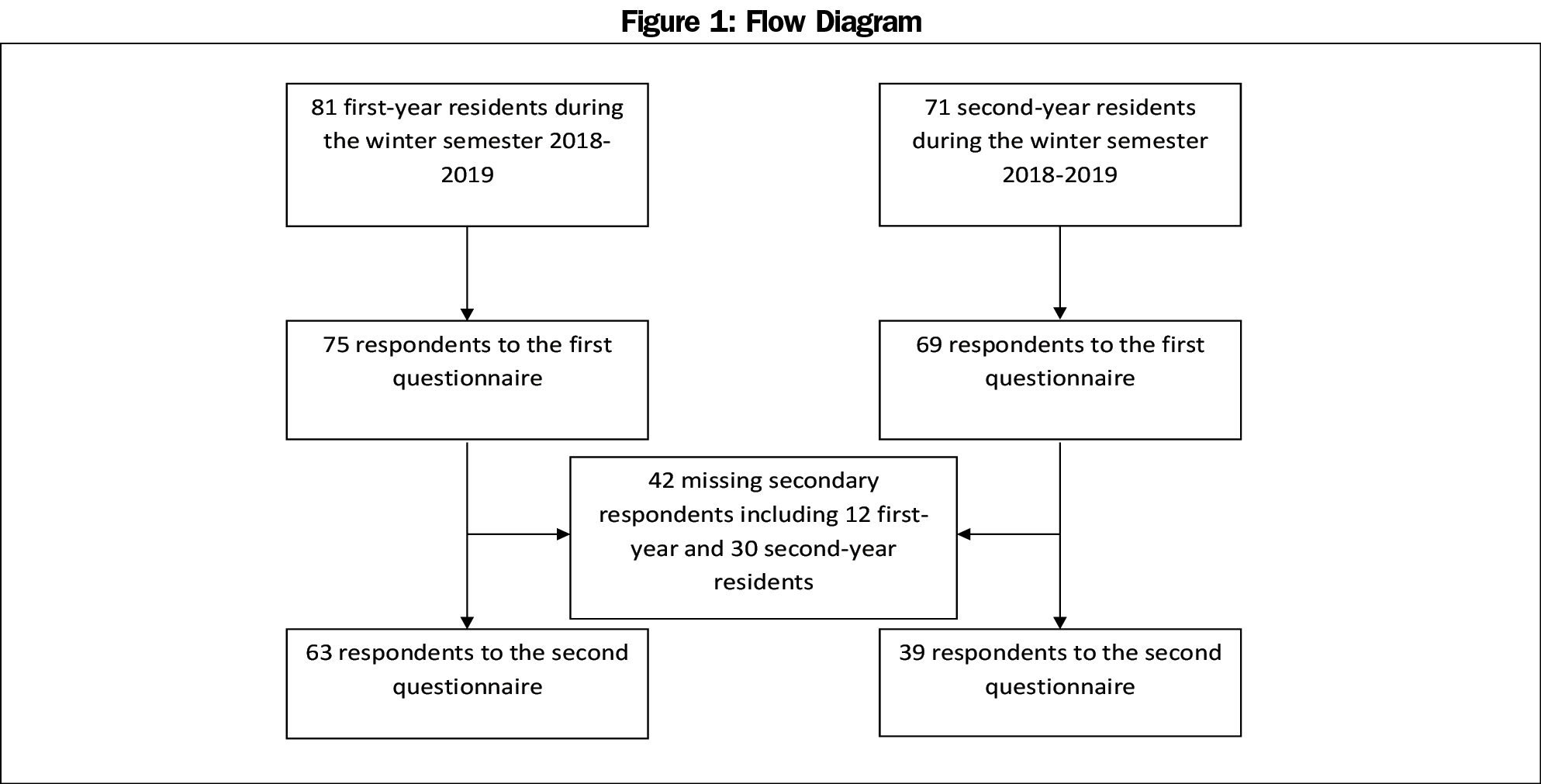
Of the 152 first- and second-year family medicine residents in Toulouse, France, 144 responded to the first questionnaire. One hundred-two could be matched after responding to the second questionnaire; 42 could not be matched. The participation rate was 95% for the first questionnaire, and 67% following the matching with the second questionnaire (Figure 1). The questionnaires from the beginning of the clinical rotation that could not be matched at the end of the clinical rotation did not show statistically different responses from the matched questionnaires (P=.61).
Global Evolution
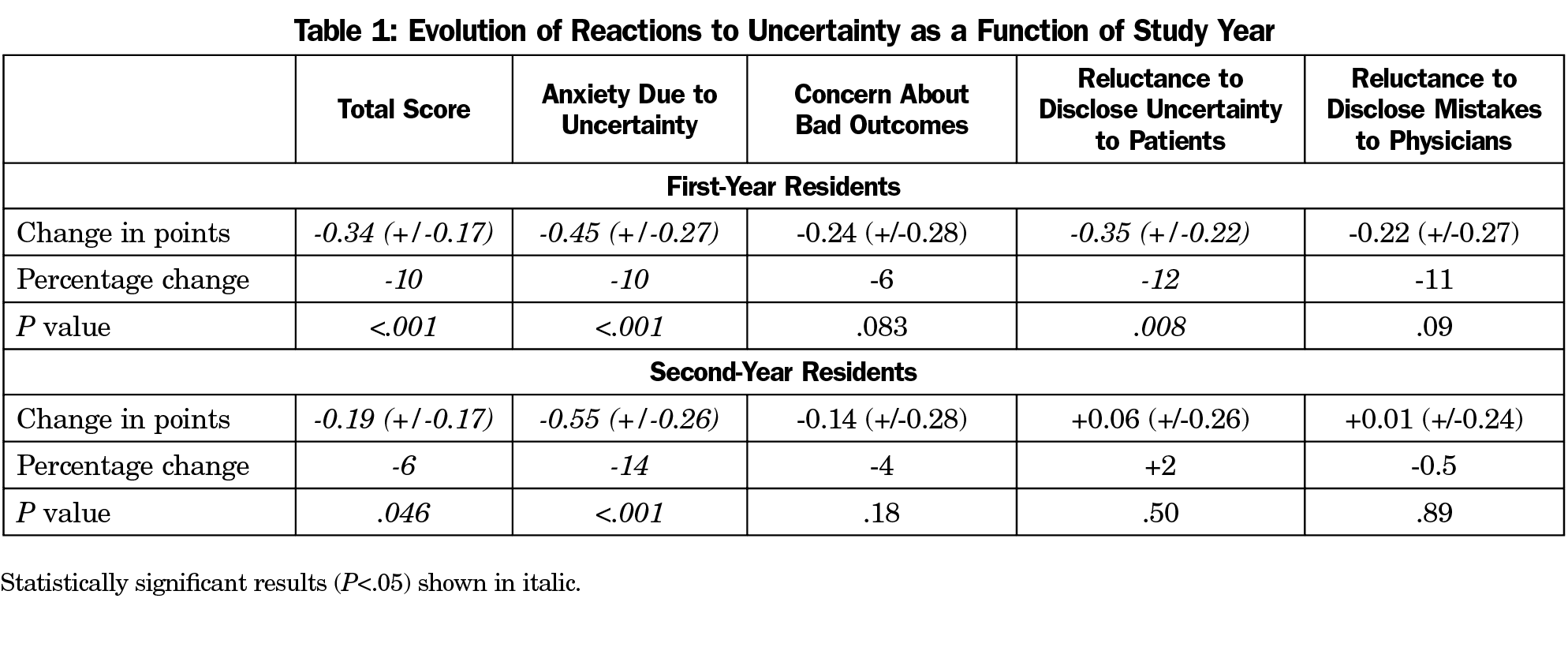
Reactions toward uncertainty improved during the course of a 6-month clinical rotation in a family physicians’ office in first- and second-year residents (Table 1). The evolution from the baseline score showed an improvement in the reactions in residents who had a medium or high score at the beginning of the clinical rotation, whereas the reactions worsened in residents who had a low baseline score. This was more apparent in dimensions concerning “anxiety due to uncertainty” and “reluctance to disclose uncertainty to patients.”
Evolution as a Function of Sex
Sex did not have a strong influence on the evolution of the reactions to uncertainty (Figure 3). Only one item had a statistical trend: the evolution of “concern about bad outcomes” was slightly decreased in males (-0.39 +/-0.39 points) compared to females (-0.12 +/-0.24 points), but not significantly (P=.25). This is noteworthy considering that “concern about bad outcomes” was lower in males (2.99 (+/- 0.44) points) than in females (3.63 [+/- 0.25] points; P=.02) at the beginning of the clinical rotation.
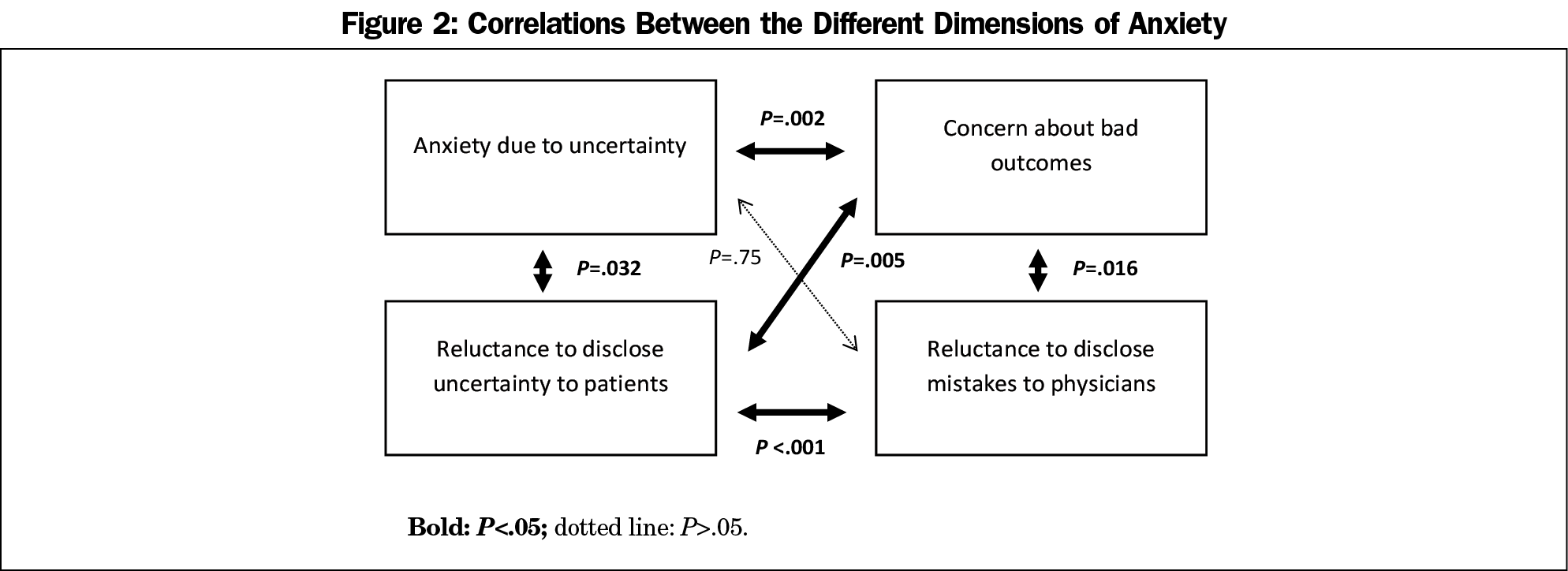
Correlation Between Dimensions
We found a high correlation between the evolution of reactions in each dimension. Each dimension was correlated with the others except for “anxiety due to uncertainty,” which was not correlated with “reluctance to disclose mistakes to physicians” (Figure 2).
Evolution as a Function of the Study Year
At the beginning of the clinical rotation, there were no significant differences between the mean scores of first- and second-year residents (P=.14), or between the scores of first- and second-year residents in each dimension of the PRU (Table 2).
The study year influenced the evolution of “reluctance to disclose uncertainty to patients.” It decreased in first-year residents (P=.008), but was considered unchanged in second-year residents (P=.50). The difference between first- and second-year residents was statistically significant (P=.02).
Summary of the Results
Reactions toward uncertainty in first and second years family medicine residents improved during the course of a 6-month clinical rotation in a family physician’s office. Anxiety due to uncertainty decreased and concern about bad outcomes tended to decrease with time in both groups of residents, whereas reluctance to disclose uncertainty to patients and reluctance to disclose mistakes to physicians decreased in first-year residents, but not in second-year residents. Sex did not have a significant influence on reactions to uncertainty, though a statistical trend was noted regarding concern about bad outcomes, which decreased further in males than in females.
About the Study Results
The results confirmed our first hypothesis that reactions to uncertainty evolves positively during the course of a 6-month outpatient rotation. The modest improvement in reactions to uncertainty could be explained by the brief rotation in a family physician’s office (only 6 months).
Our second hypothesis was not confirmed; there were no differences at baseline regarding reactions to uncertainty between first-year and second-year residents despite the fact that second-year residents undertook a clinical rotation in their first year or residency. Year of residency has an impact on the strategies used to cope with uncertain situations.19 One hypothesis could be that the second-year residents’ skills to cope with uncertainty are developed, but the reactions to uncertainty remain stable. Another hypothesis could be that 1 year of experience was not sufficient to see a significant difference in reactions to uncertainty. An Australian study conducted on 3 years of residency in family medicine identified that residents in earlier residency terms had higher scores for “anxiety due to uncertainty,” “concern about bad outcomes,” and “reluctance to disclose uncertainty to patients.”20
Sex did not have a strong influence on the evolution of the reactions to uncertainty, contrary to other studies that showed significant differences between male and female for both populations of residents and physicians.20-22 The small size of the sample could account for the nonsignificant results in our study in contrast with the literature.
Anxiety due to uncertainty decreased significantly for both first- and second-year residents. This is a significant result considering that anxiety due to uncertainty could lead to difficulties such as burnout.10,14,15 Participating in a family physician’s consultation and being able to see the family physician accepting and coping with uncertainty may have helped the residents see the positive aspect of uncertainty. Participation in peer groups as a part of the teaching during the clinical rotation, where participants shared clinical situations that led to anxiety, could be another explanation.8
Concern about bad outcomes tended to decrease during the course of a clinical rotation but not significantly. Concern about bad outcomes could be a positive reaction in some circumstances, for example to avoid a premature closure diagnosis.23 The clinical rotation during which residents discover new clinical situations could reinforce this concern. The family physician supervisor must encourage the resident to manage this reaction, so as to complete the consultation to the required level, and at the same time avoid any nonnecessary examinations.
Reluctance to disclose uncertainty to patients decreased in first-year residents but not in second-year residents. In the literature, higher training level and patient-centered approach are associated with ease in disclosing uncertainty to patients.20,24
Revealing uncertainty to the patient, verbally or nonverbally, can lead to lower patient satisfaction.25 It can also lead to a deterioration in the doctor-patient relationship in young patients with a low sociocultural background and who haven’t known their family physician for a long time.26 However, revealing certain types of uncertainty can have a positive effect on the relationship between a doctor and his patient. These types of uncertainty depend on the patient, his/her personality, and life history.26 Doctors who express uncertainty more clearly to the patient often have more positive communication skills and share more information with their patient.27
Reluctance to disclose mistakes to physicians decreased during the course of a clinical rotation for first-year residents. For residents, reluctance to disclose mistakes to physicians could include a difficulty not directly linked to the managing of uncertainty. Disclosing a mistake to a clinical teacher could impact the judgment of the teacher on the resident’s work and progression. Farnon et al showed that there is a “hierarchy of assistance” and residents ask their referent physician for help as a last resort due to fears of losing autonomy, revealing knowledge gaps, and being a bother.28 However, it is encouraging that first-year residents felt more able to disclose mistakes to physicians at the end of the clinical rotation, as disclosure allows feedback which is an important part of clinical learning in the context of uncertainty.29
Study Strengths and Limitations
To our knowledge, there is no study focusing on the evolution of reactions to uncertainty, as all data found in the literature were on cross-sectional studies. The novelty of our study is a strength as reactions to uncertainty change during the course of a residency, and because the clinical rotation in a family physician’s office could be one of the main supports to learning how to cope with uncertainty. We performed this evaluation using a questionnaire validated in French in a population of residents.
One limitation of the study was represented by the nongeneralizability of the data due to the fact that the study was conducted in a single faculty of medicine, during 2 study years, representing a small and homogeneous sample of 102 residents. Another limit was the rate of loss to follow-up. This loss was correlated with the residents’ availability during the second delivery of the questionnaire for the second-year residents: the choice of their next clinical rotation was a stressful moment, and many declined to participate in the study; in addition, some questionnaires were not correctly filled out. Finally, the measures of residents’ reactions to uncertainty were not associated with any baseline measure of residents’ experiences of uncertainty, in particular how often they felt uncertain, or in which situations, etc. Our study did not permit interpretation of the impact of a clinical rotation on coping with uncertainty.
Perspectives on Teaching
To propose specific pedagogic approaches on reactions to uncertainty, the gap in the literature could be filled through further studies focusing on (1) what level of anxiety due to uncertainty and concern about bad outcomes is likely to have a positive and stimulating effect on learning; and (2) how frequently and in what situations residents have bad reactions to uncertainty.
For now, perspectives on teaching are focused on the pedagogic skills and approaches to help residents cope with uncertainty.
Dealing and coping with uncertainty is a core clinical competency for residents in most countries.30 The aims are to help residents accept uncertainty and cope with it instead of trying to diminish it.24 Reactions and emotions involving uncertainty can have positive aspects that must be taken into account. Facing medical uncertainty is described by residents as a cause of major stress.31 However, it is not a problem limited to insecure, failing residents, but is an inherent part of care,2 especially for complex chronic patients.32
Students’ epistemological positions influence their reactions to uncertainty: a biopsychosocial epistemology is associated with fewer stress reactions to uncertainty, and a biomedical epistemology is associated with more stress reactions to uncertainty.7
Residents’ biopsychosocial epistemology could be reinforced when they learn how to propose a patient-centered approach, focusing on understanding the patient’s reasons for consulting and his environment. In this situation, a patient -centered approach is proposed to cope with uncertainty.24 For this goal, teaching could aim to:
- integrate the psychological, social, and environmental dimensions to help understand the whole person and the family context24,33; residents, when confronted with complex contextual factors feel uncertain during clinical reasoning13;
- integrate communication skills in consultation, in order to understand the patients’ demand to cope with uncertainty; and to communicate the uncertainty to patient and his/her family33; and
- conduct a narrative review to explore the known and unknown limits of medical science.34,35
The pedagogic method proposed could include:
- simulation-based intervention during classroom time, effective in improving residents’ skills in communicating about diagnostic uncertainty with patients and families and favored by residents36,37;
- the practice of inquiry, to share case-based clinical uncertainty in small group settings in order to enhance clinical judgment through collegial collaboration38; and
- a literature-searching skills workshop that could improve research abilities postintervention.39
A 6-month clinical rotation was associated with a decrease of the reaction “anxiety due to uncertainty.” Residents’ reactions to uncertainty are a concern for family medicine, as the prevalence of uncertainty is high and the residents’ reactions can have positive or negative effects on their learning. The frequency and type of uncertain situations residents encounter could be investigated in future studies to better understand residents’ reactions to uncertainty. Targeted learning on communications skills and a patient-centered approach could be included in clinical rotation to help residents cope with uncertainty.
Acknowledgments
The authors thank the teachers for their cooperation in the distribution of the questionnaire to students, and they thank the students who responded to the request to participate.
References
- Beresford EB. Uncertainty and the shaping of medical decisions. Hastings Cent Rep. 1991;21(4):6-11. https://doi.org/10.2307/3562993
- Ledford CJ, Cafferty LA, Seehusen DA. Socializing Identity Through Practice: A Mixed Methods Approach to Family Medicine Resident Perspectives on Uncertainty. Fam Med. 2015;47(7):549-553.
- Biehn J. Managing uncertainty in family practice. Can Med Assoc J. 1982;126(8):915-917.
- Politi MC, Légaré F. Physicians’ reactions to uncertainty in the context of shared decision making. Patient Educ Couns. 2010;80(2):155-157. https://doi.org/10.1016/j.pec.2009.10.030
- Carney PA, Waller E, Eiff MP, et al. Measuring family physician identity: the development of a new instrument. Fam Med. 2013;45(10):708-718.
- Nevalainen M, Kuikka L, Pitkälä K. Medical errors and uncertainty in primary healthcare: a comparative study of coping strategies among young and experienced GPs. Scand J Prim Health Care. 2014;32(2):84-89. https://doi.org/10.3109/02813432.2014.929820
- Evans L, Trotter DRM. Epistemology and uncertainty in primary care: an exploratory study. Fam Med. 2009;41(5):319-326.
- Luther VP, Crandall SJ. Commentary: ambiguity and uncertainty: neglected elements of medical education curricula? Acad Med. 2011;86(7):799-800. https://doi.org/10.1097/ACM.0b013e31821da915
- Berner ES, Graber ML. Overconfidence as a cause of diagnostic error in medicine. Am J Med. 2008;121(5)(suppl):S2-S23. https://doi.org/10.1016/j.amjmed.2008.01.001
- Cooke GPE, Doust JA, Steele MC. A survey of resilience, burnout, and tolerance of uncertainty in Australian general practice registrars. BMC Med Educ. 2013;13(1):2. https://doi.org/10.1186/1472-6920-13-2
- Allison JJ, Kiefe CI, Cook EF, Gerrity MS, Orav EJ, Centor R. The association of physician attitudes about uncertainty and risk taking with resource use in a Medicare HMO. Med Decis Making. 1998;18(3):320-329. https://doi.org/10.1177/0272989X9801800310
- Bhise V, Rajan SS, Sittig DF, Morgan RO, Chaudhary P, Singh H. Defining and Measuring Diagnostic Uncertainty in Medicine: A Systematic Review. J Gen Intern Med. 2018;33(1):103-115. https://doi.org/10.1007/s11606-017-4164-1
- McBee E, Ratcliffe T, Picho K, et al. Consequences of contextual factors on clinical reasoning in resident physicians. Adv Health Sci Educ Theory Pract 2015;20(5):1225–12-36. https://doi.org/10.1007/s10459-015-9597-x
- Kimo Takayesu J, Ramoska EA, Clark TR, et al. Factors associated with burnout during emergency medicine residency. Acad Emerg Med. 2014;21(9):1031-1035. https://doi.org/10.1111/acem.12464
- Simpkin AL, Khan A, West DC, et al. Stress From Uncertainty and Resilience Among Depressed and Burned Out Residents: A Cross-Sectional Study. Acad Pediatr. 2018;18(6):698-704. https://doi.org/10.1016/j.acap.2018.03.002
- Cooke G, Tapley A, Holliday E, et al. Responses to clinical uncertainty in Australian general practice trainees: a cross-sectional analysis. Med Educ. 2017;51(12):1277-1288. https://doi.org/10.1111/medu.13408
- University Department of Family Medicine of Paris Diderot. Eleven Situations. https://dmg.medecine.univ-paris-diderot.fr/p/les-11-familles-de-situation. Accessed February 5, 2020.
- Le Roux V. French cultural and psychometric validation of the PRU Physician’s Reactions to Uncertainty. The PRU scales were developed in the U.S. to measure physicians’ affective reactions to uncertainty. [Validation culturelle et psychometrique française du PRU Physicians’ Reactions to Uncertainty scales, questionnaire américain de mesure des réactions affectives des médecins face à l’incertitude.] MD thesis. Brest, France: University Bretagne Occidentale; 2015.
- Hamui-Sutton A, Manzano Patiño AP, Gutiérrez- Barreto SE, et al. On medical uncertainty and coping strategies during resident education. JEHD 2018;7(1):98-108.
- Cooke G, Tapley A, Holliday E, et al. Responses to clinical uncertainty in Australian general practice trainees: a cross-sectional analysis. Med Educ. 2017;51(12):1277-1288. https://doi.org/10.1111/medu.13408
- Gerrity MS, Earp JAL, DeVilles RF. Uncertainty and professional work: perceptions of physicians in clinical practice. Am J Sociol. 1992;97(4):1022-1051. https://doi.org/10.1086/229860
- Geller G, Faden RR, Levine DM. Tolerance for ambiguity among medical students: implications for their selection, training and practice. Soc Sci Med. 1990;31(5):619-624. https://doi.org/10.1016/0277-9536(90)90098-D
- Sacchi S, Cherubini P. The effect of outcome information on doctors’ evaluations of their own diagnostic decisions. Med Educ. 2004;38(10):1028-1034. https://doi.org/10.1111/j.1365-2929.2004.01975.x
- Yaphe J. Teaching and Learning About Uncertainty in Family Medicine. In: WONCA Europe. The World Book of Family Medicine – European edition, first edition. Ljubljana (Slovenia); 2015.
- Johnson CG, Levenkron JC, Suchman AL, Manchester R. Does physician uncertainty affect patient satisfaction? J Gen Intern Med. 1988;3(2):144-149. https://doi.org/10.1007/BF02596120
- Ogden J, Fuks K, Gardner M, et al. Doctors expressions of uncertainty and patient confidence. Patient Educ Couns. 2002;48(2):171-176. https://doi.org/10.1016/S0738-3991(02)00020-4
- Gordon GH, Joos SK, Byrne J. Physician expressions of uncertainty during patient encounters. Patient Educ Couns. 2000;40(1):59-65. https://doi.org/10.1016/S0738-3991(99)00069-5
- Farnan JM, Johnson JK, Meltzer DO, Humphrey HJ, Arora VM. Resident uncertainty in clinical decision making and impact on patient care: a qualitative study. Qual Saf Health Care. 2008;17(2):122-126. https://doi.org/10.1136/qshc.2007.023184
- Chaou CH, Chang YC, Yu SR, et al. Clinical learning in the context of uncertainty: a multi-center survey of emergency department residents’ and attending physicians’ perceptions of clinical feedback. BMC Med Educ. 2019;19(1):174. https://doi.org/10.1186/s12909-019-1597-8
- Kim K, Lee YM. Understanding uncertainty in medicine: concepts and implications in medical education. Korean J Med Educ. 2018;30(3):181-188. https://doi.org/10.3946/kjme.2018.92
- Nevalainen MK, Mantyranta T, Pitkala KH. Facing uncertainty as a medical student—a qualitative study of their reflective learning diaries and writings on specific themes during the first clinical year. Patient Educ Couns. 2010;78(2):218-223. https://doi.org/10.1016/j.pec.2009.07.011
- van lersel MB, Brantjes E, de Visser M et al. Tolerance of clinical uncertainty by geriatric residents: a qualitative study. Eur Geriatr Med 2019;10: 517-22.
- Blasco PG. Family Medicine Miles Programme: Getting Students Involved Where There is No Family Medicine in Medical School. In: WONCA Europe. The World Book of Family Medicine – European edition, first edition. Ljubljana (Slovenia); 2015.
- Ledford CJW, Seehusen DA, Chessman AW, Shokar NK. How we teach U.S. medical students to negotiate uncertainty in clinical care: a CERA study. Fam Med. 2015;47(1):31-36.
- Smith AK, White DB, Arnold RM. Uncertainty—the other side of prognosis. N Engl J Med. 2013;368(26):2448-2450. https://doi.org/10.1056/NEJMp1303295
- Olson ME, Borman-Shoap E, Mathias K, Barnes TL, Olson APJ. Case-based simulation empowering pediatric residents to communicate about diagnostic uncertainty. Diagnosis (Berl). 2018;5(4):243-248. https://doi.org/10.1515/dx-2018-0025
- Rising KL, Papanagnou D, McCarthy D, Gentsch A, Powell R. Emergency medicine resident Perceptions about the need for increased training in communicating diagnostic uncertainty. Cureus. 2018;10(1):e2088. https://doi.org/10.7759/cureus.2088
- Kenyon T, Allen CW, Siegel A. Using practice inquiry to engage uncertainty in residency education. In: Siegel Sommers L, Launer J, eds. Clinical Uncertainty in Primary Care, The challenge of collaborative engagement. New York: Springer; 2014.
- Just ML. Is literature search training for medical students and residents effective? a literature review. J Med Libr Assoc. 2012;100(4):270-276. https://doi.org/10.3163/1536-5050.100.4.008





There are no comments for this article.