Background and Objectives: Discharge delay of hospitalized patients is costly, inefficient, and can impede care of pending admissions. Through pharmacist colocation and daily discharge medication reconciliation meetings, we aimed to improve discharge efficiency and decrease the number of electronic pages.
Methods: We conducted a quality improvement initiative on the family medicine inpatient teaching service at a large academic medical center using two interventions: colocation and daily discharge medication reconciliation meetings of pharmacist and family medicine residents. We assessed: (1) discharge delay, defined as the time between discharge order and pharmacist’s completion of discharge medication reconciliation and patient education; (2) the number of electronic messages between the pharmacist and family medicine team, assessed 1 month before and 1 month after implementation of the interventions. We also assessed team members’ postinitiative views on collaboration, discharge safety, and timeliness, and knowledge acquisition using three 5-point Likert statements.
Results: Ninety-five preintervention and 54 postintervention patients met eligibility criteria. Discharge delay prior to intervention was 72.7±58.4 minutes and 47.6±37.4 minutes postintervention. The number of electronic messages between pharmacist and family medicine team pager decreased from 118 to 14 during the months studied. Team members felt collaboration, safe and timely discharges, and acquisition of new knowledge improved.
Conclusions: Colocation of workspaces and daily medication reconciliation meetings were associated with decreased discharge delay and decreased pages between team members. Further study is needed to assess its reproducibility, impact on resident education and patient satisfaction, cost-effectiveness, and ability to scale to other services.
Delayed discharge of patients medically ready to leave the hospital is common, expensive, delays new admissions, and has negative effects on patient health and satisfaction.1 Pharmacist involvement in discharge processes may be associated with decreased health care utilization,2 improved patient satisfaction, increased medication adherence,3 decreased medication errors,4 and improved quality, safety, and efficiency of care.5 Interdisciplinary teams with pharmacist-assisted discharge medication reconciliation may improve discharge efficiency,6 and performing discharge medication reconciliation the night before discharge may lead to earlier discharges and decreased readamissions.7
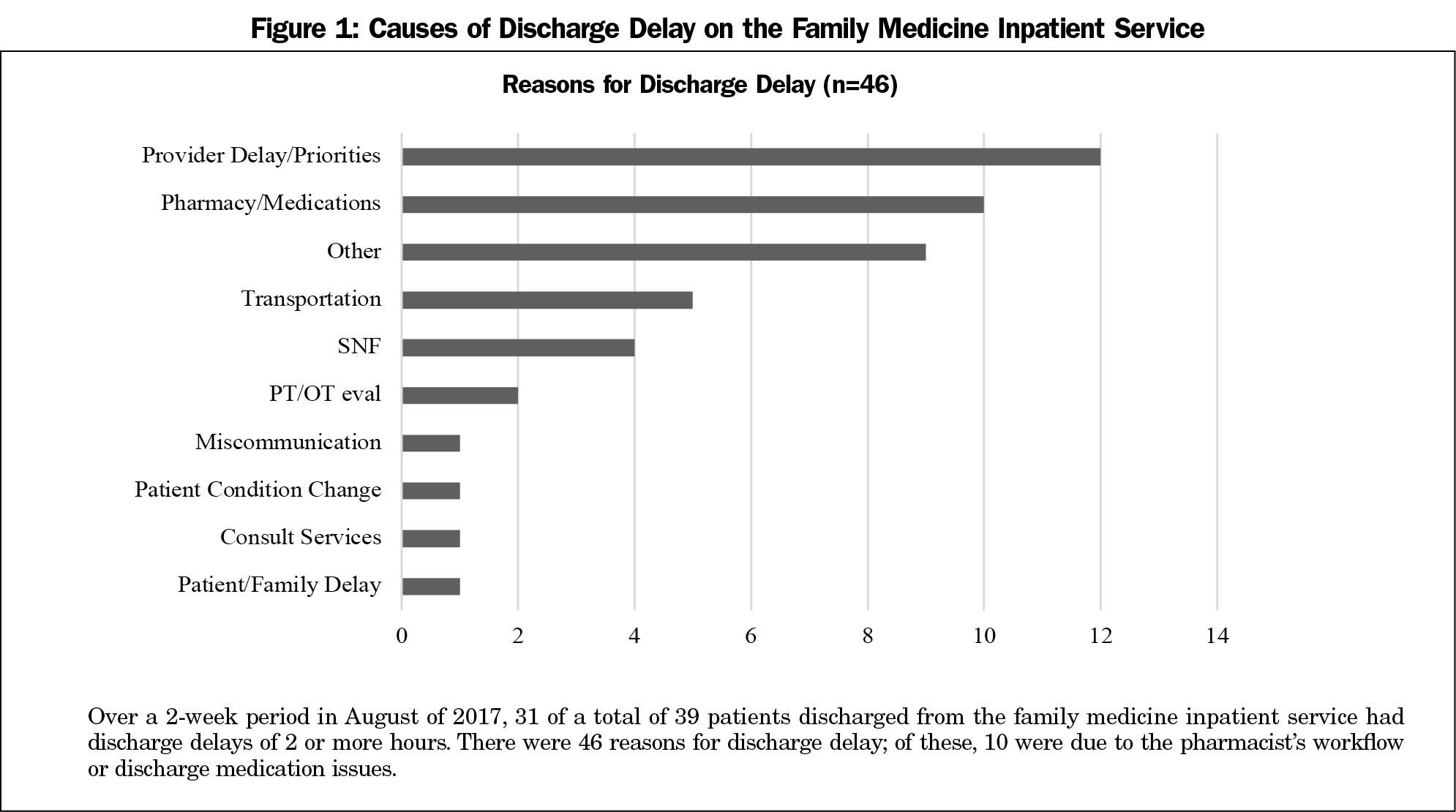
A 2-week manual count on our family medicine inpatient unit found 31 of 39 (79.5%) of discharges were delayed at least 2 hours after medical readiness. Of 46 reasons for delay, 10 were attributed to pharmacist workflow or medication issues (Figure 1). Through detailed process mapping, we recognized delays were often related to pharmacist-resident communication and reworking discharge medication orders. We conducted a quality improvement initiative to address both issues by integrating the pharmacist’s workspace into the family medicine team room (colocation) and holding daily discharge-related team meetings.
This quality improvement initiative was exempt from institutional review board oversight. Deidentified data were obtained from electronic health records consistent with the Health Insurance Portability and Accountability Act (HIPAA). The initiative took place at a large academic teaching hospital within a single inpatient service consisting of one attending physician, one nurse practitioner, two senior residents, two first-year residents, and one pharmacist . Preintervention data were collected in October 2017, and postintervention data in January 2018. The eligibility criterion was being a family medicine inpatient on our teaching unit. The intervention comprised two components: the pharmacist’s workspace was moved into the family medicine team’s workspace (colocation), and pharmacist and residents met at 2 pm daily to initiate discharge medication reconciliation for one to three patients expected to discharge the following day. The pharmacist reviewed the medication reconciliation and orders were pended or signed during the meeting.
The primary outcome measure was “discharge delay”, defined as time between the resident placing the discharge order and the pharmacist completing the medication reconciliation and patient education, measured via electronic medical record time stamps. The secondary outcome was the number of pages between the pharmacist and the family medicine team during the pre- and postassessment periods. Results were compared using descriptive statistics and a t test. Residents and pharmacists were not aware these outcomes were being measured. We also assessed via three 5-point Likert scale statements the degree to which team members felt the intervention: (1) improved collaboration, (2) facilitated safe and timely discharges, and (3) improved their knowledge base.
The family medicine service discharged 119 and 106 patients in the pre- and postintervention months; 95 and 54 met eligibility, respectively. Of the 22 weekdays in January 2018, meetings occurred 15 times (68.2% adherence) for 16.9±9.5 minutes. Meeting adherence improved when both the residents and pharmacists received an automatic reminder page and adherence was limited by clinical responsibilities (eg, patient urgencies, admissions). Discharge delay was reduced by 25.1 minutes, from 72.7±58.4 minutes to 47.6±37.4 minutes (P=.002). The percentage of discharges taking more than 100 minutes decreased from 25% to 4%. The number of pages between pharmacist and residents decreased from 118 to 14, or from 1.0 to 0.13 pages per patient. The resident response rate on the questionnaire was 70.5% (12/17); residents noted improved collaboration (4.3±١.٢/٥), facilitation of safe and timely discharges (٣.٨±١.١/٥), and new knowledge acquisition (٤.٠±١.٢/٥).
The main findings of this pilot-level quality improvement initiative are that colocation of family medicine inpatient team and pharmacist and collaborative meetings may be associated with discharge delay reduction and fewer pages between pharmacist and residents, which was viewed favorably. The pre/post nature of our initiative limits claims to causality; findings are suggestive. To our knowledge, there were no other concomitant initiatives at our institution. The response to internal presentation to hospital personnel suggested other services did not experience these changes, which further suggests causality between our intervention and results. Discharge delay is a national problem, and has been associated with mortality, infections, and decreased patient mobility.1 In this quality improvement initiative, efforts on the day prior to discharge appear to have reduced workload on the day of discharge for both pharmacist and physician, thus shortening time to discharge of medically ready patients. Our findings have been met locally with enthusiasm; other teaching services in our hospital have recently implemented similar efforts.
These findings are consistent with studies reporting early entry of discharge medications can improve efficiency on day of discharge.7 We suspect the mechanism of improvement is multifactorial including increase efficiency by addressing discharge issues earlier and provider collaboration evaluating complex medical issues in real time. Pharmacist involvement in discharge processes may improve patient safety; a 22% decrease in medication errors was reported when pharmacists prepared the discharge medication reconciliation.8 In our study, residents participated in the reconciliation process for educational purposes. The meetings for discharge medication reconciliation allowed the pharmacist to supervise and provide guidance, which likely improves patient safety. Also consistent with prior work is our finding that colocation is associated with positive response among pharmacists and residents. Clinical staff located central to communication had improved job satisfaction compared with those more distal and less face to face.9 Colocation may therefore be relevant to the discussion of job satisfaction.
This study was limited by a small sample size and nonvalidated outcome measures. We included an unequal number of discharges prior to and after the interventions, though our total number of discharges was consistent in the pre/post periods. We are unable to separate the effects of colocation and meetings, and suspect they have synergistic effects. Team personnel and attending physicians were different in the pre- and postperiods, adding variability.
In summary, this pilot-level quality improvement initiative suggests that colocation of physicians and pharmacists and daily discharge meetings may reduce discharge delay and decrease use of electronic pages while improving team satisfaction. Planned work includes assessing these interventions on other units, reviewing patient satisfaction with the discharge process, improving meeting adherence by demonstrating the value of meetings, and evaluating impact on resident education.
Acknowledgments
Presentations: Data from this study were previously presented as follows:
Bonk N, Goplen A, McElray K. Improving Hospital Discharge Efficiency by Resident-Pharmacist Collaboration. Family Medicine Midwest, Madison, WI; November 9, 2018.
Bonk N, Goplen A, McElray K, Milsap A. Improvement in Discharge Delays Through Pharmacist Collaboration and Resident Education. Society of Hospital Medicine Annual Conference, Washington, DC. March 25, 2019
Bonk N, Goplen A, McElray K, Milsap A, Rabago D. Improving Hospital Discharge Efficiency Through Resident-Pharmacist Collaboration. Society of Teachers of Family Medicine Annual Spring Conference, Toronto, Canada. April 29, 2019
Bonk N, Goplen A, McElray K, Milsap A, Rabago D. Improvement in Discharge Delays Through Pharmacist Collaboration and Resident Education. North American Primary Care Research Group (NAPCRG) Annual Conference; Toronto, Canada. November 18, 2019.
References
- Rojas-García A, Turner S, Pizzo E, Hudson E, Thomas J, Raine R. Impact and experiences of delayed discharge: A mixed-studies systematic review. Health Expect. 2018;21(1):41-56. doi:10.1111/hex.12619
- Mueller SK, Sponsler KC, Kripalani S, Schnipper JL. Hospital-based medication reconciliation practices: a systematic review. Arch Intern Med. 2012;172(14):1057-1069. doi:10.1001/archinternmed.2012.2246
- Sarangarm P, London MS, Snowden SS, et al. Impact of pharmacist discharge medication therapy counseling and disease state education: Pharmacist Assisting at Routine Medical Discharge (project PhARMD). Am J Med Qual. 2013;28(4):292-300. doi:10.1177/1062860612461169
- Keeys C, Kalejaiye B, Skinner M, et al. Pharmacist-managed inpatient discharge medication reconciliation: a combined onsite and telepharmacy model. Am J Health Syst Pharm. 2014;71(24):2159-2166. doi:10.2146/ajhp130650
- Kaboli PJ, Hoth AB, McClimon BJ, Schnipper JL. Clinical pharmacists and inpatient medical care: a systematic review. Arch Intern Med. 2006;166(9):955-964. doi:10.1001/archinte.166.9.955
- Statile AM, Schondelmeyer AC, Thomson JE, et al. Improving discharge efficiency in medically complex pediatric patients. Pediatrics. 2016;138(2):e20153832. doi:10.1542/peds.2015-3832
- Durvasula R, Kayihan A, Del Bene S, et al. A multidisciplinary care pathway significantly increases the number of early morning discharges in a large academic medical center. Qual Manag Health Care. 2015;24(1):45-51. doi:10.1097/QMH.0000000000000049
- Craynon R, Hager DR, Reed M, Pawola J, Rough SS. Prospective daily review of discharge medications by pharmacists: effects on measures of safety and efficiency. Am J Health Syst Pharm. 2018;75(19):1486-1492. doi:10.2146/ajhp170638
- Mundt MP, Zakletskaia LI. Professional communication networks and job satisfaction in primary care clinics. Ann Fam Med. 2019;17(5):428-435. doi:10.1370/afm.2442



There are no comments for this article.