Nonsteroidal anti-inflammatory drugs (NSAIDs) are one of the most commonly used pain medications among US adults, with about 70 million people regularly taking NSAIDs annually.1,2 NSAIDs are continually prescribed inappropriately in high-risk patients despite clear recommendations from current clinical practice guidelines and recent supporting literature that recommend to avoid NSAID use long-term in patients with chronic kidney disease (CKD),1,3-6 preexisting hypertension (HTN),1,6-13 and heart failure (HF).14-18 This puts patients at risk for greater morbidity and mortality. The primary objective of this study was to determine the impact of direct, pharmacist-led education to family medicine providers on rates of inappropriate prescribing of NSAIDs in high-risk populations.
BRIEF REPORTS
Pharmacist-Led Provider Education on Inappropriate NSAID Prescribing Rates
Jangus B. Whitner, PharmD | Nicole A. Fabiili, PharmD | Jordan Siewart, DO | Karen Akasaka, DO | Anna Nelson, MD, MS
Fam Med. 2020;52(8):592-596.
DOI: 10.22454/FamMed.2020.147410
Background and Objectives: Nonsteroidal anti-inflammatory drugs (NSAIDs) are one of the most commonly used pain medications among US adults with about 70 million people regularly taking NSAIDs annually. Despite clear recommendations from current clinical practice guidelines and recent supporting literature, NSAIDs are continually prescribed inappropriately in patients with chronic kidney disease (CKD), hypertension (HTN), and heart failure (HF). The purpose of this project was to determine the impact of direct pharmacist-led education to providers on rates of inappropriate prescribing of NSAIDs in high-risk populations in a family medicine setting.
Methods: This study included all adult (aged 18 years or older) patient charts with NSAIDs prescribed, refilled, or recorded within the specified time periods. We defined inappropriate orders as oral and of chronic duration (at least 90 days) with at least one high-risk International Classification of Diseases-10 chart diagnosis (HTN, HF, CKD). This was a single-center, retrospective chart review of prescribing rates during a 3-month period before and after provider education delivered by a pharmacist.
Results: We identified a total of 325 charts from preintervention and 489 charts postintervention that met inclusion criteria. Of those, the charts with orders categorized as inappropriate were 90 versus 44, respectively. The rate of inappropriate prescribing of NSAIDs significantly decreased from 27.7% to 9.0% (P<.0001) postintervention. Among chronic NSAID users, both serum creatinine and systolic blood pressure significantly increased following NSAID initiation.
Conclusions: A single pharmacist-led education intervention to primary care providers on inappropriate NSAID use in high-risk patient populations had a significant impact on minimizing inappropriate NSAID prescribing patterns within a family medicine outpatient office.
We chose a single-site family medicine residency center for this pre/post-intervention study. The primary outcome was to determine the impact of direct provider education on rates of inappropriate prescribing of oral NSAIDs in high-risk patients (those with CKD, HF, or HTN). The secondary outcomes focused on an aggregate group of high-risk patients across both phases—comparing changes in serum creatinine (SCr) and blood pressure (BP) measurements before and after the identified start date of chronic NSAID use. Data from each identified chart was reviewed independently by a single investigator, documented in a spreadsheet, and stored on secure ProMedica Health System computers. The ProMedica Institutional Review Board approved this study.
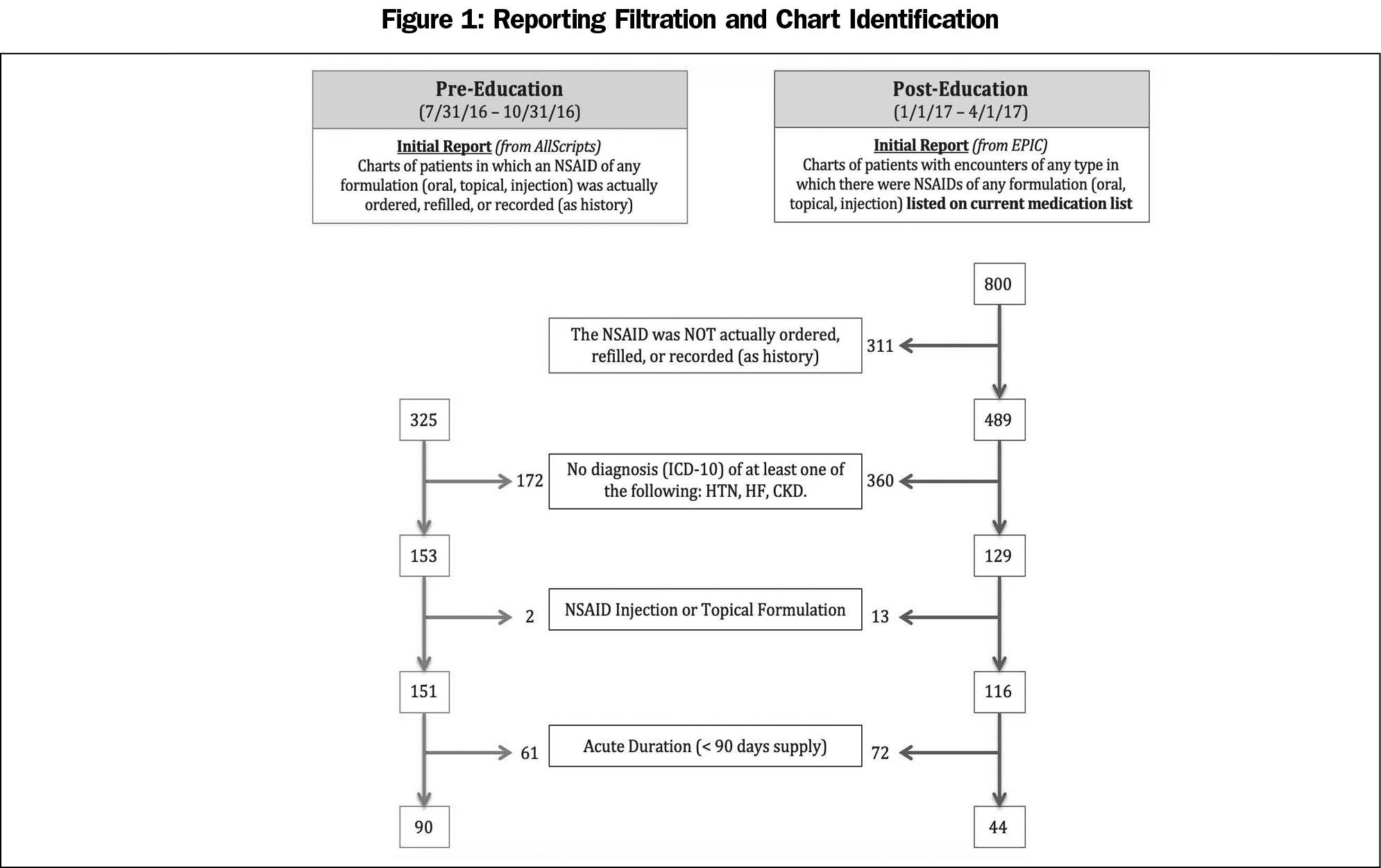
Preintervention
Investigators completed a 3-month retrospective chart review (July 31 2016 through October 31, 2016) through the electronic medical record (EMR), AllScripts. Investigators ran a report to identify the denominator: charts of adult patients, at least 18 years old, who had NSAIDs (of any formulation) ordered, refilled, or recorded (as history) within the specified time frame. We then reviewed the charts for accuracy to ensure the charts identified by the report truly had NSAID orders actually prescribed, refilled, or recorded. Then we reviewed the charts per the filtration process detailed in Figure 1 to identify the inappropriate group, defined as at least one high-risk diagnosis (an International Classification of Diseases [ICD] code designating a comorbidity of CKD [of any cause], HTN, or HF), oral NSAID order, and prescribed chronically (at least 90 days). Topical/injectable orders were excluded from the inappropriate categorization.
Intervention
Pharmacists provided education on appropriate NSAID prescribing practices on December 16, 2016. This didactic, 50-minute noon conference presentation was delivered to prescribing providers (attending physicians, resident physicians, certified nurse practitioners, and a clinical pharmacist) and nonprescribing pharmacy residents, pharmacy students, and medical students. Content included a literature review of NSAID use in high-risk populations, alternative therapy options, and related case-based questions. The majority of the prescribing providers (74.1%) were present.
Postintervention
Investigators performed the same data collection process/review for 3 months (January 1, 2017 through April 1, 2017) using the office’s new EPIC electronic medical record (EMR) system.
Statistical Analysis
We considered a P value <.05 statistically significant. We performed analysis as follows: primary outcome (χ2), baseline characteristics (Student t test, χ2, Fisher exact test), and secondary outcomes (paired t tests).
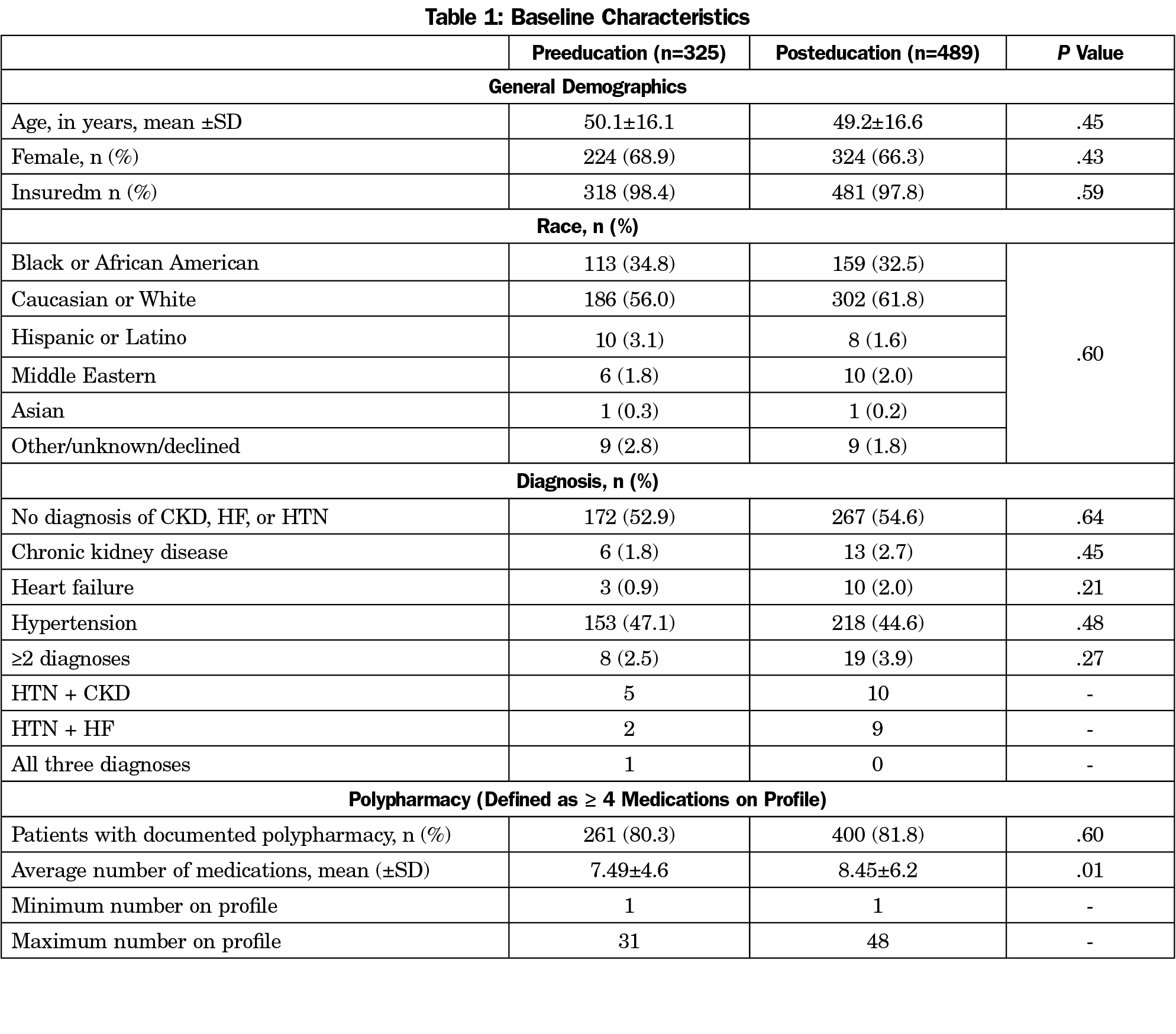
A combined total of 1,125 charts were identified by the EMR reports, and 814 charts were confirmed to have a NSAID order (of any formulation) across the review periods (325 pre- vs 489 postintervention, Figure 1). The fraction of patients who were prescribed NSAIDs of any duration who also had a diagnosis of CKD, HTN, or HF was lower in the postintervention period (47.1% vs 26.4%), as was the incidence of chronic prescriptions (59.6% vs 37.9%). Baseline characteristics were similar between pre- and postgroups with the exception of mean number of medications per patient profile significantly higher in the postintervention group (7.49 vs 8.45, P=0.01, Table 1).
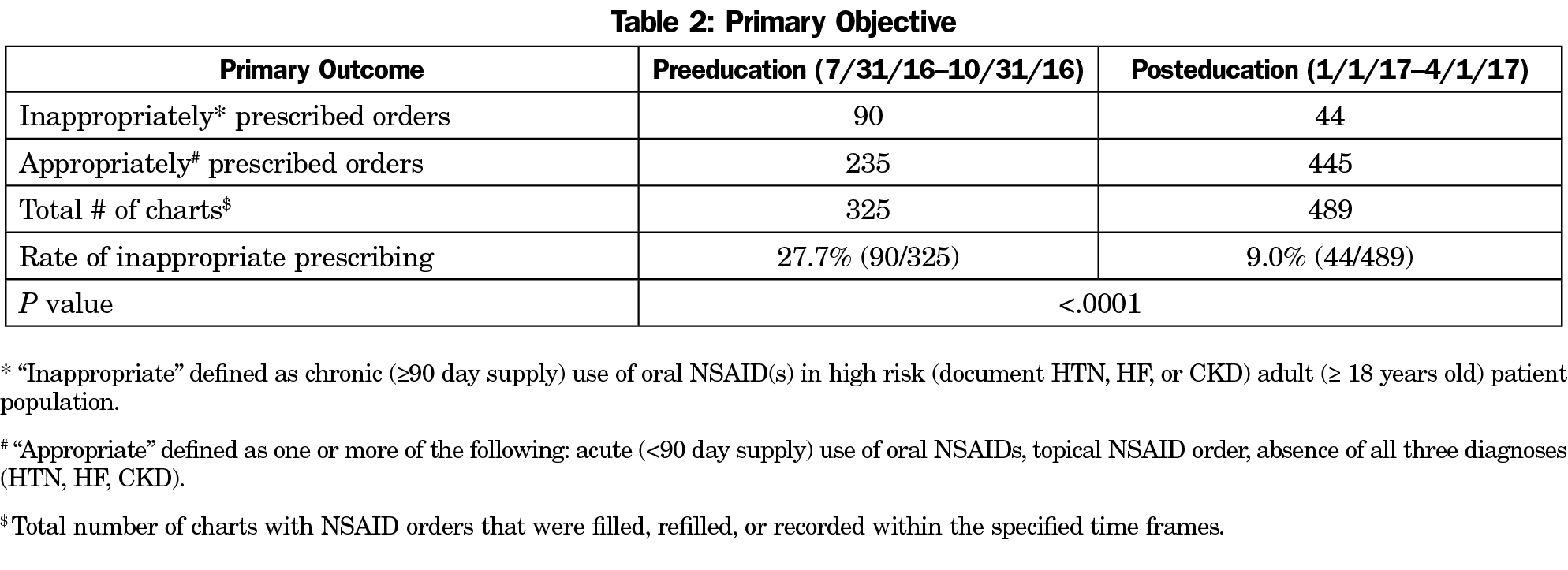
The primary outcome yielded a significant reduction of inappropriately prescribed NSAID orders in high-risk populations from 27.6% to 9.0% postintervention, (P<.0001, Table 2).
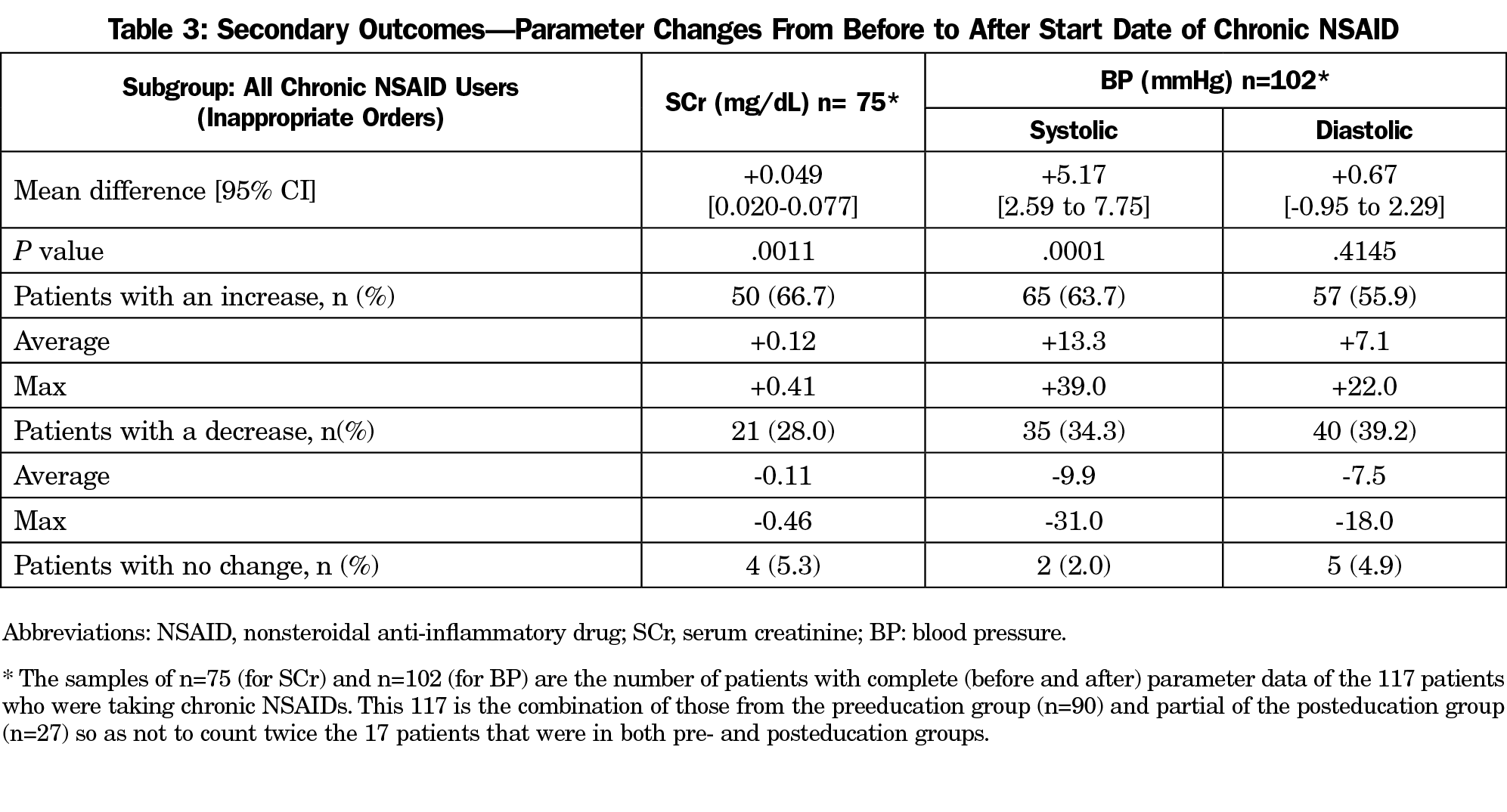
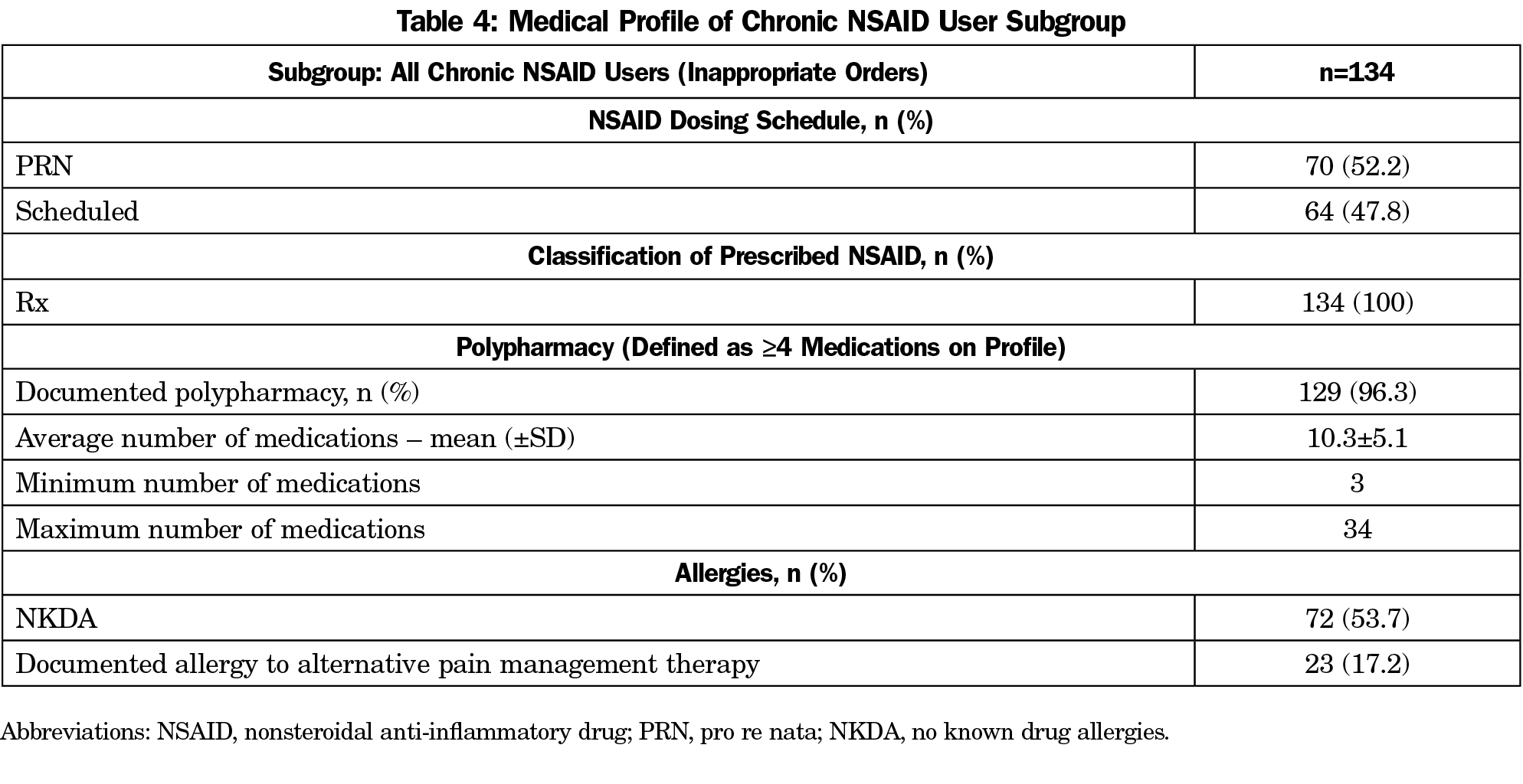
Secondary outcomes (Table 3) specifically looked at the subgroup of all 117 high-risk chronic NSAID users: those from pre- (n=90) and postintervention (n=27) groups with removal of the 17 duplicate patients that showed up in both time frames. Only those patients who had the necessary SCr lab result (75 patients, 64.1%) and BP measurement data (102 patients, 87.2%) from before and after the identified start date of chronic NSAID orders were included for secondary analyses. Both SCr and systolic BP significantly increased after initiating chronic NSAIDs: +0.049 mg/dL (P=.0011), +5.17 mmHg (P=.0001), respectively. For a complete breakdown for the medical profiles of the patients in the inappropriate prescribed group, see Table 4.
The primary outcome’s statistically significant reduction in inappropriate NSAID prescribing rates after provider education by a pharmacist demonstrates the significant influence that just one educational session can have on minimizing inappropriate prescribing patterns for high-risk patients in the family medicine setting.
The secondary outcomes of the study mirrored our expectation that prolonged NSAID use can lead to statistically significant elevations in SCr and systolic BP. Although not statistically significant, diastolic BP did increase in the majority of patients (55.9%). These outcomes stress the necessity to stay up to date with clinical practice guidelines to ensure best delivery of patient care, especially to high-risk patient populations.
Compared to the overall study group, the inappropriate subgroup had a larger percentage of patient profiles with documented polypharmacy in addition to a higher number of average medications on the profile. It is reasonable to postulate that with increasing polypharmacy comes increasing difficulty for providers to thoroughly assess appropriateness of every medication on the list at each visit. This highlights another role that pharmacists could play in the family medicine setting via opportunities like comprehensive medication review and reconciliation.
This study has multiple limitations. First, calculation of power was unable to be performed due to lack of prior applicable literature. Second, the retrospective review was performed using two different EMRs with the ease of data gathering varying greatly. Third, this pre/postintervention study did not include a control group (no educational intervention) over the same time period for comparative analysis of the primary outcome. This confounds the ability to control for increased levels of available didactic materials related to NSAID prescribing/deprescribing. A fourth, and perhaps most important limitation, is the possible reporting bias. NSAIDs are available over the counter and their use is likely underreported by patients. In particular, our secondary outcome analysis is especially affected by the underreporting as well as other potential confounders such as the timing of measurement in relation to NSAID start date. Similarly, underreporting of CKD in the EMR is quite probable, as Barnes and colleagues19 in 2014 found that 65% of the patient profiles evaluated did not have active CKD identified as a medical problem. These two limitations could further underestimate the rate of inappropriate NSAID use in high-risk populations.
Another limitation is that occasionally providers write for 90-day supplies because it is cheaper through insurance, although the patient may not necessarily take it every day. During our chart review we sought to account for that and confirm chronic use by looking at refill history before and after the NSAID order presented on our report.
Our study evaluated prescribing habits for a 3-month time period posteducation but did not assess the lasting effects of this change. The study period was not long enough to fully account for the patient-oriented success of the providers’ deprescribing attempts such as the positive effect on blood pressure for hypertensive patients weighed against their success of pain relief with the alternative therapy.
Lastly, our study was conducted in Ohio in the midst of the opioid epidemic and there was pressure upon primary care providers (PCPs) to seek appropriate alternatives to long-term opioids for chronic pain. The limitation is that although this push could have increased rates of PCP prescribing of NSAIDs as an alternative to opioids, on the other hand it could also have triggered more attention by PCPs to appropriate NSAID use.
The retrospective nature of this study and utilization of four data collectors helped minimize investigator bias. Selection bias was minimized as the EMR reporting software was used to generate lists of charts for the filtration process. Additionally, this study had a respectable sample size and what appears to be great provider buy-in. Despite the limitations, this study can be a potential starting point for future research, including the expansion of NSAID education, its patient-oriented impact beyond 3-months posteducation, and to compare the effects of different durations of NSAID use on SCr and BP.
In summary, pharmacist-led education intervention on inappropriate NSAID use in high-risk patient populations in a family medicine outpatient setting had a significant impact on minimizing inappropriate prescribing patterns.
Acknowledgments
The authors thank Dr Janee Whitner for her help in reviewing the manuscript and Roberta Redfern for providing biostatistical support.
Presentations: This study was presented at the Ohio Pharmacy Residency Conference, on May 19, 2017 in Ada, Ohio.
References
- Williams AW, Dwyer AC, Eddy AA, et al; American Society of Nephrology Quality, and Patient Safety Task Force. Critical and honest conversations: the evidence behind the “Choosing Wisely” campaign recommendations by the American Society of Nephrology. Clin J Am Soc Nephrol. 2012;7(10):1664-1672. https://doi.org/10.2215/CJN.04970512
- American College of Rheumatology. Information for patients about NSAIDs. Updated March 2019. Available at: http://www.rheumatology.org/I-Am-A/Patient-Caregiver/Treatments/NSAIDs. Accessed February 19, 2020.
- Nash DM, Markle-Reid M, Brimble KS, et al. Nonsteroidal anti-inflammatory drug use and risk of acute kidney injury and hyperkalemia in older adults: a population-based study. Nephrol Dial Transplant. 2019;34(7):1145-1154. https://doi.org/10.1093/ndt/gfz062
- National Kidney Foundation. Kidney Disease Improving Global Outcomes (KDIGO): clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2012;3(1):1-163.
- Ungprasert P, Cheungpasitporn W, Crowson CS, Matteson EL. Individual non-steroidal anti-inflammatory drugs and risk of acute kidney injury: A systematic review and meta-analysis of observational studies. Eur J Intern Med. 2015;26(4):285-291. https://doi.org/10.1016/j.ejim.2015.03.008
- Lapi F, Azoulay L, Yin H, Nessim SJ, Suissa S. Concurrent use of diuretics, angiotensin converting enzyme inhibitors, and angiotensin receptor blockers with non-steroidal anti-inflammatory drugs and risk of acute kidney injury: nested case-control study. BMJ. 2013;346(jan08 12):e8525. https://doi.org/10.1136/bmj.e8525
- Hwang AY, Dave CV, Smith SM. Use of prescription medications that potentially interfere with blood pressure control in new-onset hypertension and treatment-resistant hypertension. Am J Hypertens. 2018;31(12):1324-1331. https://doi.org/10.1093/ajh/hpy118
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/ AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol. 2018;71(19):e127-e248. https://doi.org/10.1016/j.jacc.2017.11.006
- Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32(1):3-15. https://doi.org/10.1097/HJH.0000000000000065
- National Heart, Lung, and Blood Institute, U.S. Department of Health and Human Services. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure (JNC 7). 2007. http://www.nhlbi.nih.gov/health-pro/guidelines/current/hypertension-jnc-7. Accessed October 1, 2016.
- Antman EM, Bennett JS, Daugherty A; American Heart Association. Use of nonsteroidal anti-inflammatory drugs: an update for clinicians: a scientific statement from the American Heart Association. Circulation. 2007;115(12):1634-1642. https://doi.org/10.1161/CIRCULATIONAHA.106.181424
- Fournier JP, Sommet A, Bourrel R, et al. Non-steroidal anti-inflammatory drugs (NSAIDs) and hypertension treatment intensification: a population-based cohort study. [published online ahead of print April 15, 2012]. Eur J Clin Pharmacol. 2012;68(11):1533-1540. https://doi.org/10.1007/s00228-012-1283-9
- Chuang SY, Yu Y, Sheu WHH, et al. Association of short-term use of nonsteroidal anti-inflammatory drugs with stroke in patients with hypertension. Stroke. 2015;46(4):996-1003. https://doi.org/10.1161/STROKEAHA.114.007932
- Atherton JJ, Sindone A, De Pasquale CG; NHFA CSANZ Heart Failure Guidelines Working Group. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: 2018 Guidelines for the prevention, detection, and management of heart failure in Australia. Heart Lung Circ. 2018;27(10):1123-1208. https://doi.org/10.1016/j.hlc.2018.06.1042
- Yancy CW, Jessup M, Bozkurt B, et al; WRITING COMMITTEE MEMBERS; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128(16):e240-e327.
- Scottish Intercollegiate Guidelines Network (SIGN). Management of chronic heart failure: a national clinical guideline. SIGN publication no. 14. Edinburgh:Healthcare Improvement Scotland; March 2016 https://www.sign.ac.uk/assets/sign147.pdf
- Arfè A, Scotti L, Varas-Lorenzo C, et al; Safety of Non-steroidal Anti-inflammatory Drugs (SOS) Project Consortium. Non-steroidal anti-inflammatory drugs and risk of heart failure in four European countries: nested case-control study. BMJ. 2016;354:i4857. https://doi.org/10.1136/bmj.i4857
- Feenstra J, Heerdink ER, Grobbee DE, Stricker BH. Association of nonsteroidal anti-inflammatory drugs with first occurrence of heart failure and with relapsing heart failure: the Rotterdam Study. Arch Intern Med. 2002;162(3):265-270. https://doi.org/10.1001/archinte.162.3.265
- Barnes KD, Tayal NH, Lehman AM, Beatty SJ. Pharmacist-driven renal medication dosing intervention in a primary care patient-centered medical home. Pharmacotherapy. 2014;34(12):1330-1335. https://doi.org/10.1002/phar.1508
Lead Author
Jangus B. Whitner, PharmD
Affiliations: PrimaryOne Health, Columbus, OH
Co-Authors
Nicole A. Fabiili, PharmD - Beaumont Hospital, Troy, MI
Jordan Siewart, DO - ProMedica Physicians, Adult Medicine, Toledo, OH
Karen Akasaka, DO - St Luke’s Hospital Family Medicine Residency, Perrysburg, OH
Anna Nelson, MD, MS - St Luke’s Hospital Family Medicine Residency, Perrysburg, OH
Corresponding Author
Jangus B. Whitner, PharmD
Correspondence: PrimaryOne Health, 2780 Airport Drive, Suite 100, Columbus, OH 43219. 614-859-1887. Fax: 614-645-5517.
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.