Background and Objectives: Patients with severe mental illness often lack care coordination between primary care and mental health providers which can negatively impact patient outcomes. Team-based care is integral in the effective management of patients with multiple comorbidities, with the family physician central in coordinating holistic care. Family medicine residency programs must provide models of effective interprofessional collaboration and mental health treatment to prepare residents to navigate an evolving health care landscape. The objective of this study was to evaluate family medicine residents’ learning about providing holistic care with an interprofessional team and medication safety monitoring from the interprofessional cross-organizational care conference experience.
Methods: To bridge care and cultivate the necessary skills, a family medicine clinic and mental health clinic implemented monthly interprofessional care conferences to coordinate care for their shared patients during 2019. Residents who participated in the care conference each (n=11) completed a retrospective pre/postsurvey (11/11=100% response rate) to gather perceptions of what they learned from the interprofessional care conference experience.
Results: After participating in the care conference, all residents agreed they understood the elements that must be considered to provide holistic patient care, were confident conducting medication safety monitoring for their patients taking second-generation antipsychotics (eg, lipids, A1C, ECG), and agreed the care conference helped them develop a more comprehensive patient-centered care plan. Additionally, they all intend to work collaboratively across professions in the future.
Conclusions: Interprofessional and cross-organizational care conferences create an authentic learning environment that enhances family medicine residents’ understanding and confidence in providing collaborative and holistic care for patients with severe and persistent mental illness.
Increased suicide rates, comorbid psychiatric and medical conditions, psychiatric medication adverse reactions, and diminishing access to mental health services are some of the challenges facing today’s primary care physicians.1-4 This is particularly concerning in rural communities where disparities in access to mental health services exist.5 Treatment of severe mental illness (SMI) requires collaboration between mental health and primary care, which is challenging when these services are delivered across separate organizations. Integrated care coordination is an opportunity to address and prevent serious medical and/or medication-related consequences.4,6-11
Family medicine residencies must cultivate effective interprofessional collaboration and mental health treatment skills to prepare residents for practice. Family medicine residents and other learners can develop and practice these skills through interprofessional care conferences,12-14 which have been shown to improve patient care.15,16 The purpose of this study was to evaluate the residents’ learning about treatment of SMI from the care conference experience.
Care Conference
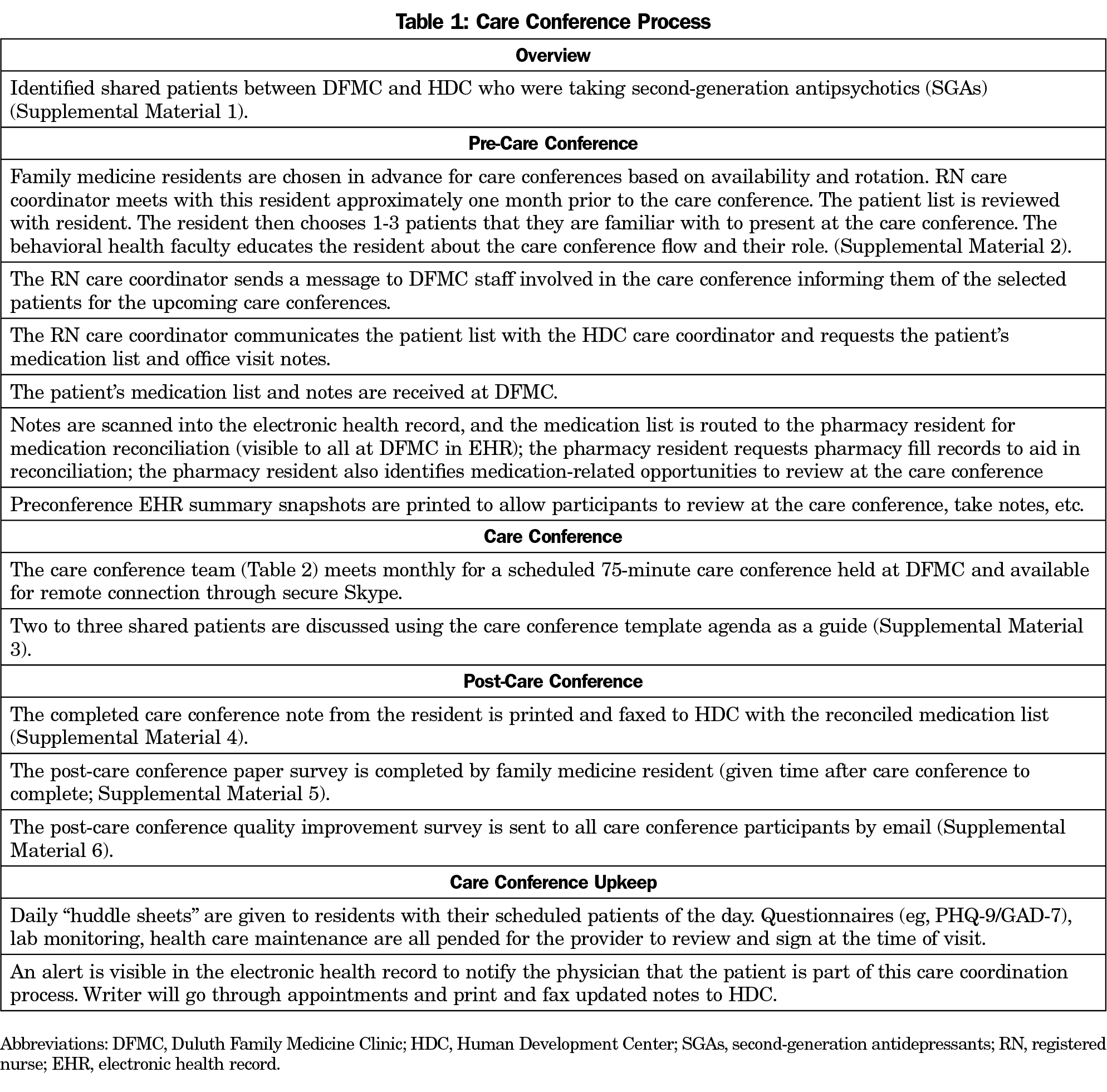
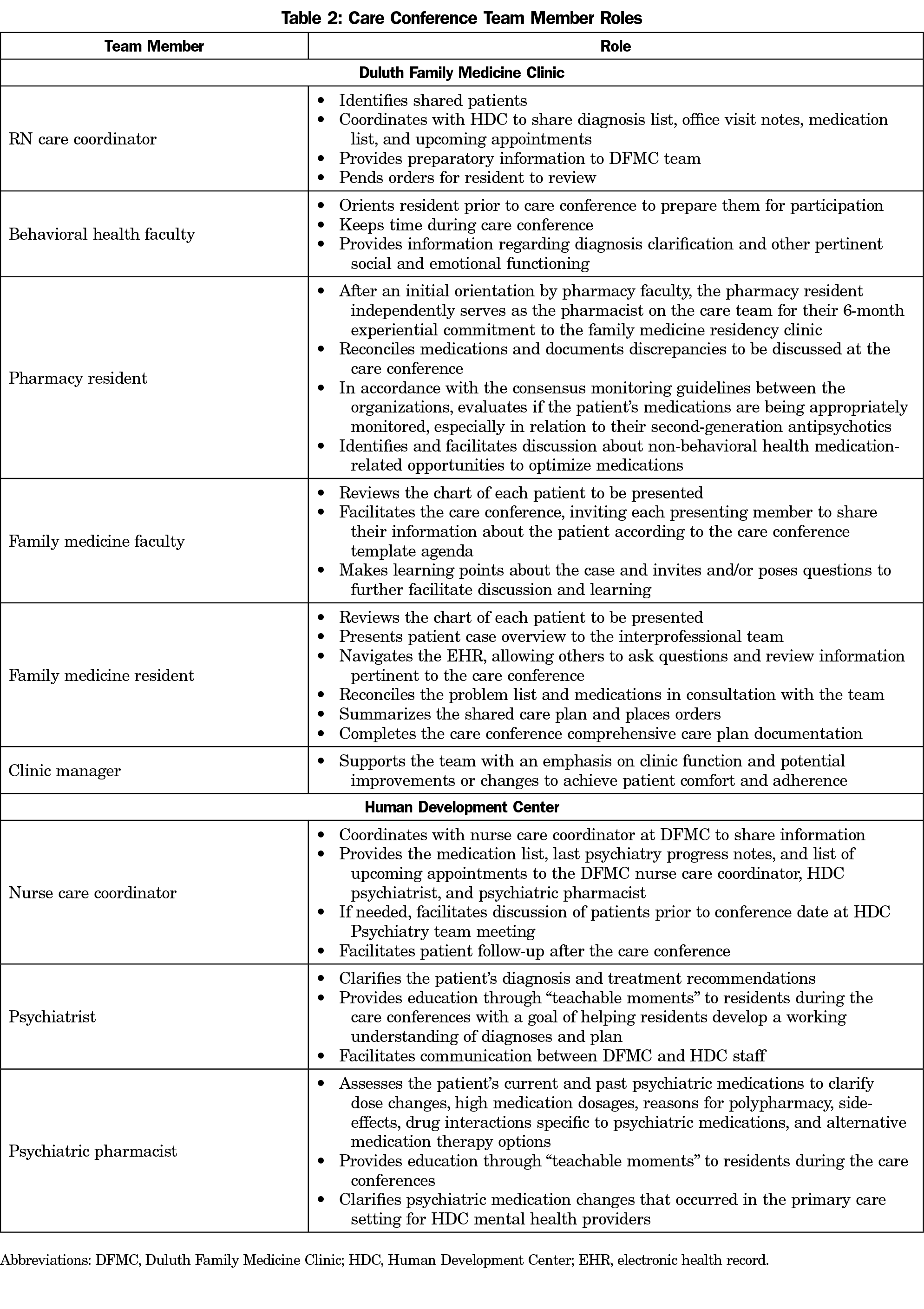
Beginning in 2019, monthly 75-minute interprofessional care conferences between family medicine and mental health were hosted at the family medicine residency training clinic. The care conference model was adapted from the EFECT (Elicit the narrative of illness, Facilitate a group meeting, Evidence-based gap analysis, Care plan, Track changes) framework for interprofessional education in the patient-centered medical home12 and the Veterans Affairs Patient-Aligned Care Team Interprofessional Care Update (PACT-ICU) model.13,14 The care conference process is described in detail in Tables 1 and 2, including care team members and their roles.
Evaluation
We used a paper-based retrospective pre/postsurvey to gather perceptions of what was learned from the care conference experience (Supplemental Material 5). We designed the retrospective pre/postsurvey to save time and reduce response-shift bias compared with a traditional pre/postsurvey. Although many experts would recommend including both measures—a traditional pre/post self-evaluation as well as the retrospective pre/post self-evaluation—to truly assess any response shift, we were unable to do so. The survey was designed to ascertain the residents’ understanding of providing holistic care, confidence in medication safety monitoring of second-generation antipsychotics (SGAs), developing comprehensive patient-centered care plans, understanding of interprofessional roles, and future plans for interprofessional collaboration. Statistical analyses were not planned given small sample size of nonnormal data. The University of Minnesota Institutional Review Board deemed the study exempt from review.
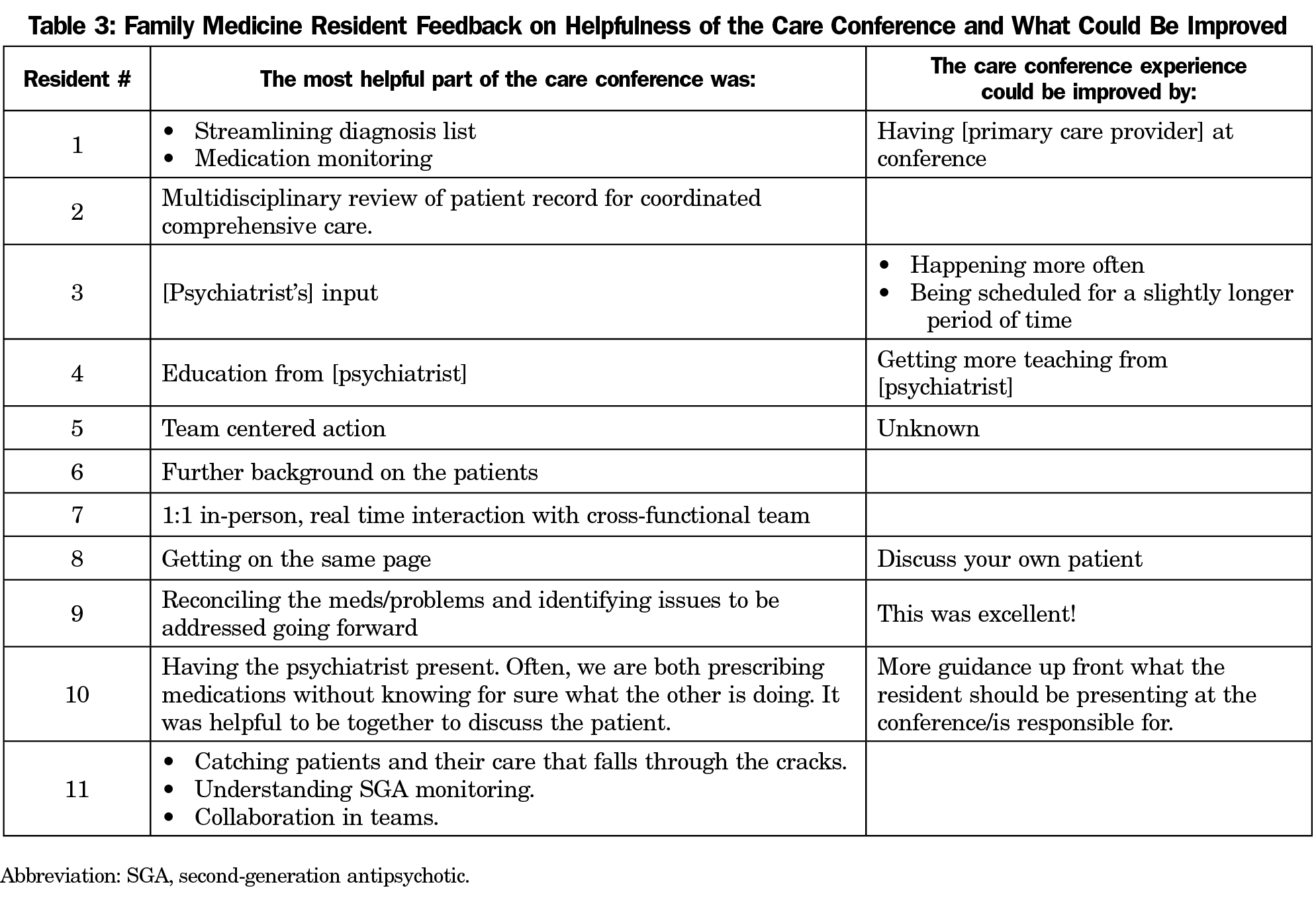
During 2019, a total of 11 second- and third-year residents participated in one of the 11 monthly care conferences (five PGY-2 and six PGY-3 residents), and all completed the postcare conference survey (100% response rate). When asked how well they understood all of the elements (biological, psychological, social) that must be considered to provide holistic patient care, residents reported an average baseline rating of 3.68 prior to the care conference, that increased to 4.32 following the care conference (scale=1 [not at all] to 5 [completely]). Confidence in conducting medication safety monitoring for patients taking SGAs increased from an average of 3.45 to 4.18 pre/postcare conference. Understanding of team members’ roles in care of complex patients increased from an average of 3.45 to 4.27 pre/post on a scale of 1 (minimal) to 5 (excellent). All residents agreed the care conference helped them develop a more comprehensive patient-centered care plan (average rating=4.82/5), and residents identified all care conference participants as contributing to the development of the treatment plan. All residents agree they plan to engage with an interprofessional team in the future care of patients (average rating=4.73/5). A list of what residents found most helpful and areas for improvement of the care conference experience are detailed in Table 3.
Resident feedback indicates the care conferences were useful for enhancing their knowledge and confidence in caring for patients with mental illness taking SGAs. There was strong agreement that the residents plan to engage with an interprofessional team in the future care of patients. These findings align with the PACT-ICU evaluation where 100% of trainees reported the care conferences were helpful or very helpful, and expressed satisfaction with the PACT-ICU conference.13 Compared with the PACT-ICU evaluation, our residents reported a higher mean baseline understanding of team members’ roles in care of complex patients and the elements that must be considered to provide holistic patient care.14
Care conferences facilitated shared decision making across psychiatry and primary care. The majority of residents reported the most helpful part of the care conference was the comprehensive multidisciplinary review, which consisted of reconciliation of diagnoses and medications. Face-to-face conversation with the psychiatrist also appeared to bolster resident confidence in leading the management of metabolic monitoring of the patient moving forward.
Cultural and resource considerations need to be evaluated should one choose to incorporate interprofessional care conferences across organizations. An interprofessional collaborative culture already existed at this residency clinic. Residents participate in collaborative education and patient care throughout their training beginning with an interprofessional orientation and shadowing activity. They spend time engaging with other interprofessional colleagues in practice on their rotations and participate in interprofessional didactic conferences. Because it is a residency training program, faculty have dedicated time for precepting and teaching that may not be available in a typical family medicine clinic. Using the 2015 Institute of Medicine conceptual framework for measuring the impact of interprofessional education,17 we determined the professional and institutional culture, workforce and financial policies in this residency program were enabling rather than interfering factors for success. A key to the infrastructure necessary for interprofessional collaborative care conferences is having engaged and committed health-system partners. Details about logistics are included in Tables 1 and 2, and Supplemental Materials 1-6.
Our survey measured resident learning outcomes at the reactions/attitudes/perceptions level,18 but we anticipate the ongoing education and collaboration will result in benefits to patients. In an ongoing study we are measuring higher level educational outcomes, including the pre/postchange in appropriate SGA monitoring for patients discussed at the care conference. The care conference team continues to meet monthly to discuss shared patients, including follow-up check-ins for shared patients that have previously been discussed who are not meeting goals.
Limitations
This study was limited to one family medicine residency training program over 1 year with a small sample size, and there is a lack of validation data for the survey items used. Only subjective measures were used for evaluation, and there was no follow-up evaluation for persisting value, nor was there objective assessment of knowledge or behavior change.
Although the importance of effective interprofessional collaboration is understood, its advancement is mired by limited clinical training sites that model authentic interprofessional team-based care.13,19 These monthly care conferences provided an educational opportunity for modeling of authentic interprofessional team-based care to experientially achieve milestones of interprofessional education and collaboration.
Acknowledgments
Financial Support: Financial support for this project was provided by Minnesota Department of Health Rural Family Medicine Residency Grant SWIFT Contract Number 201096.
Presentations: The data in this study were presented in a poster at the College of Psychiatric and Neurologic Pharmacists Annual Meeting, April 2020; the American College of Clinical Pharmacy Virtual Poster Symposium (encore) May 2020; and the Nexus Summit August 2020 (encore).
The authors acknowledge the following individuals for their contributions to this study:
Interprofessional Education and Practice Development Collaborative.
John Wood, MD – University of Minnesota Duluth Family Medicine Residency Program Director
Lisa Prusak, MD – University of Minnesota Duluth Family Medicine Residency Associate Program Director
Jason Wall, MD – University of Minnesota Duluth Family Medicine Residency Faculty
Rebekka Schrecengost, PharmD – Essentia Health Pharmacy Services and initial pharmacy resident involved with the care conferences
Anna Hanson, PharmD – Essentia Health Pharmacy Services and subsequent pharmacy resident involved with the care conferences
Megan Tapp, PharmD – Essentia Health Pharmacy Services and subsequent pharmacy resident involved with the care conferences
Steve Bauer, MD – Human Development Center Medical Director
Nicol Erdmann, RN – Human Development Center Nurse Care Coordinator.
References
- Watson LC, Amick HR, Gaynes BN, et al. Practice-based interventions addressing concomitant depression and chronic medical conditions in the primary care setting: a systematic review and meta-analysis. J Prim Care Community Health. 2013;4(4):294-306. doi:10.1177/2150131913484040
- Ahmedani BK, Simon GE, Stewart C, et al. Health care contacts in the year before suicide death. J Gen Intern Med. 2014;29(6):870-877. doi:10.1007/s11606-014-2767-3
- Institute for Health Metrics and Evaluation. The State of US Health: Innovations, Insights, and Recommendations from the Global Burden of Disease Study. Seattle, WA: IHME; 2013.
- Lerch S. The Role State Mental Health Authorities Can Play in Delivery of Integrated Primary and Behavioral Health Care for People with Serious Mental Illness, Including Those with Co-Occurring Substance Use Disorders. Alexandria, VA: Natl Assoc State Ment Heal Progr Dir; 2017:1-14.
- Levin A. Report details national shortage of psychiatrists and possible solutions. Psychiatr News. 2017;52(8):6,13. doi:10.1176/appi.pn.2017.4b24
- McGovern M, Dent K, Kessler R. A Unified model of behavioral health integration in primary care. Acad Psychiatry. 2018;42(2):265-268. doi:10.1007/s40596-018-0887-5
- Parks JJ. Implementing practice guidelines: lessons from public mental health settings. J Clin Psychiatry. 2007;68(suppl 4):45-48. doi:10.4088/JCP.0607e16
- Kates N, Arroll B, Currie E, et al. Improving collaboration between primary care and mental health services. World J Biol Psychiatry. 2019;20(10):748-765. doi:10.1080/15622975.2018.1471218
- Grøn AO, Dalsgaard E-M, Ribe AR, et al. Improving diabetes care among patients with severe mental illness: A systematic review of the effect of interventions. Prim Care Diabetes. 2018;12(4):289-304. doi:10.1016/j.pcd.2018.03.008
- Abegaze H; State Advisory Council on Mental Health and Subcommittee on Children’s Mental Health. 2016 Report to the Governor and Legislature. St. Paul, MN: Minnesota Department of Human Services; 2016.
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):629-640. doi:10.1001/archpsyc.62.6.629
- Bitton A, Pereira AG, Smith CS, Babbott SF, Bowen JL; Society of General Internal Medicine Patient-Centered Medical Home Education Summit. The EFECT framework for interprofessional education in the patient centered medical home. Healthc (Amst). 2013;1(3-4):63-68. doi:10.1016/j.hjdsi.2013.08.003
- Gardner AL, Weppner WG, Willis J, Bernotski J. PACT ICU Model: interprofessional case conferences for high-risk/high-need patients. Fed Pract. 2018;35(12):34-41.
- Weppner WG, Davis K, Sordahl J, et al. Interprofessional care conferences for high-risk primary care patients. Acad Med. 2016;91(6):798-802. doi:10.1097/ACM.0000000000001151
- Garber C, Bernadino M, Tomaskek J, Nelson KJ. The development and implementation of a patient continuity conference in a psychiatry residency program. Acad Psychiatry. 2018;42(2):233-236. doi:10.1007/s40596-017-0749-6
- Sordahl J, King IC, Davis K, et al. Interprofessional case conference: impact on learner outcomes. Transl Behav Med. 2018;8(6):927-931. doi:10.1093/tbm/ibx018
- Institute of Medicine. Measuring the Impact of Interprofessional Education on Collaborative Practice and Patient Outcomes. Washington, DC: The National Academies Press; 2015. doi:10.17226/21726
- Reeves S, Boet S, Zierler B, Kitto S. Interprofessional education and practice guide No. 3: evaluating interprofessional education. J Interprof Care. 2015;29(4):305-312. doi:10.3109/13561820.2014.1003637
- Mohaupt J, van Soeren M, Andrusyszyn M-A, Macmillan K, Devlin-Cop S, Reeves S. Understanding interprofessional relationships by the use of contact theory. J Interprof Care. 2012;26(5):370-375. doi:10.3109/13561820.2012.673512



There are no comments for this article.