Background and Objectives: The patient panels of graduating residents must be reassigned by the end of residency. This process affects over 1 million patients annually within the specialty of family medicine. The purpose of this project was to implement a structured, year-end reassignment system in a family medicine residency program.
Methods: Our structured reassignment process took place from December 2017 through June 2020. Panel lists of current, active patients were generated and residents were responsible for reassigning their own panels during a panel reassignment night. We created a tip sheet that addressed patient complexity and continuity, a risk stratification algorithm based on patients’ medical and social complexity, and a tool that tracked the number of patients assigned to each future provider. Outcome measures included a resident satisfaction survey administered in 2018-2020 and patient-provider continuity measured with a run chart from December 2016 through August 2020.
Results: The resident survey response rate was 75%. Seventy-three percent felt the panel reassignment night was very helpful; 87% thought the reassignment timeline was extremely reasonable, and 87% indicated that they had the necessary information to reassign their patients. Residents also felt confident that their patients were reassigned appropriately (33% extremely confident, 67% somewhat confident). Patient continuity improved with a 13-point run above the median, indicating nonrandom variation. Patient continuity remained above the median until the impact of COVID-19 in April 2020.
Conclusion: Our structured reassignment process was received positively by residents and resulted in improved patient continuity.
Patient empanelment can be defined as “linking each patient to a primary care provider and ideally, to a stable team.”1 It is a foundational building block of high-functioning practices2 and plays an important role in patient continuity,3 patient access, and residency education.4,5
At the end of residency, the patient panels of graduating residents must be reassigned but there is little consensus regarding best practices and, in one study, only 46% of Med/Peds programs had a structured reassignment process.6 Based on 2017 family medicine Match data,7 approximately 1 million patients will experience a transfer of care within the specialty of family medicine. This can be a particularly challenging and risky time to both patients8-10 and remaining residents.11 Creating a structured year-end sign-out process improves patient follow-up12 and positively affects both patient continuity and quality of care.13
Prior to implementing this quality improvement (QI) project, our residency program’s year-end reassignment process was not standardized, there was limited understanding of patient panels, there was no process to ensure that the new provider was noted in the patient’s record, and the process for residents was cumbersome and last minute. The purpose of this QI project was to establish and implement a structured, year-end reassignment system in a family medicine residency program.
Program
The family medicine residency program matches eight residents per year and is a 3-year program in a suburban setting. Continuity data were collected in reference to the department’s primary residency continuity teaching site.
Panel Reassignment Process
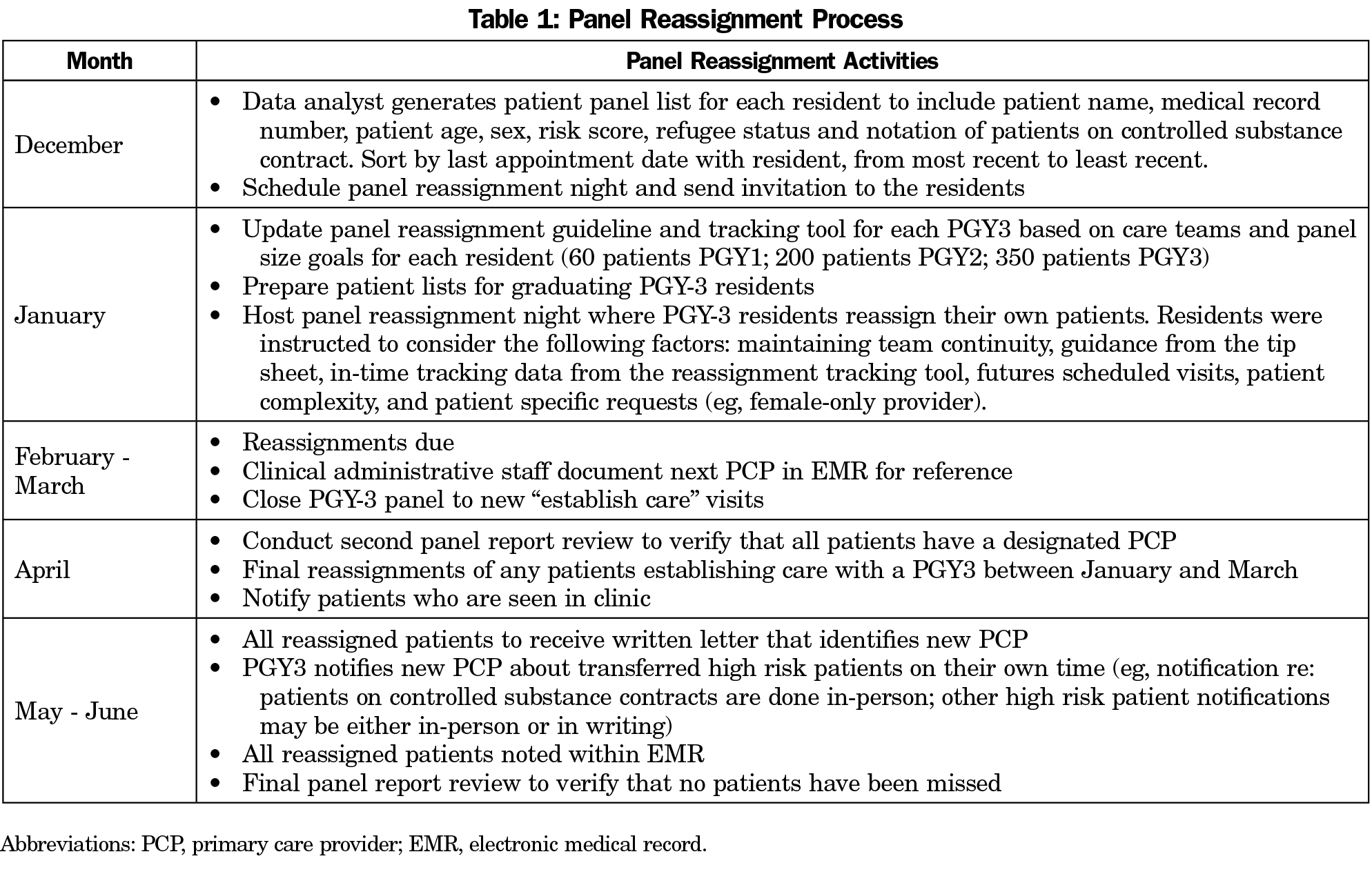
From December 2016 to June 2017, we collected baseline continuity data from our primary teaching practice. We generated panel reports for patient reassignment from the electronic medical record (EPIC) that included patient name, medical record number, age, risk score, date of last office visit in our department, date of last office visit with current primary care provider (PCP), and future scheduled visit provider name, if applicable. From 2017 to 2020, we followed the timeline outlined in Table 1 on an annual basis.
Patients who had not completed an office visit in the last 3 years were excluded from the reassignment process and designated as inactive. Within the list of active patients, residents were only asked to reassign patients they had personally seen.
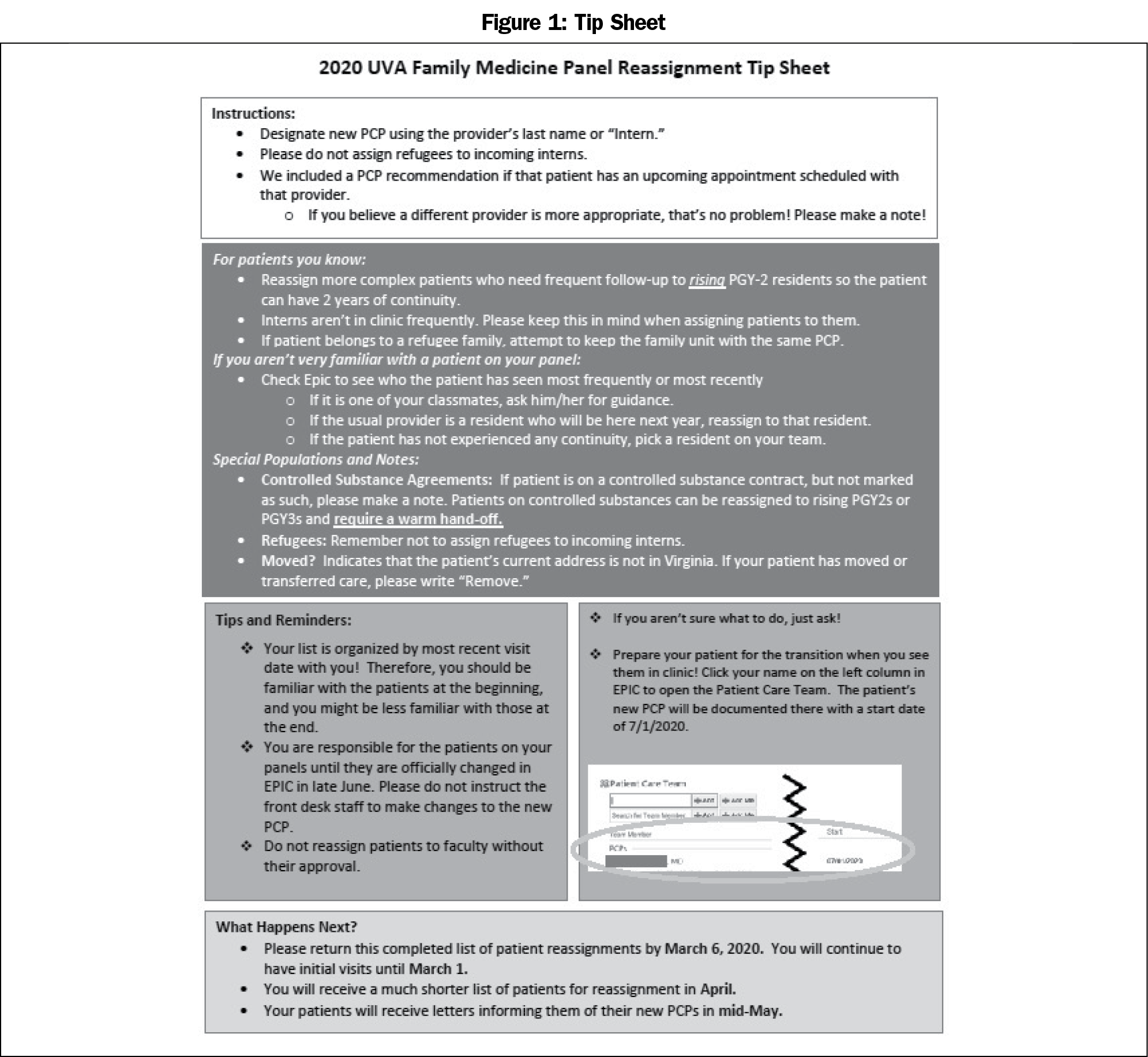
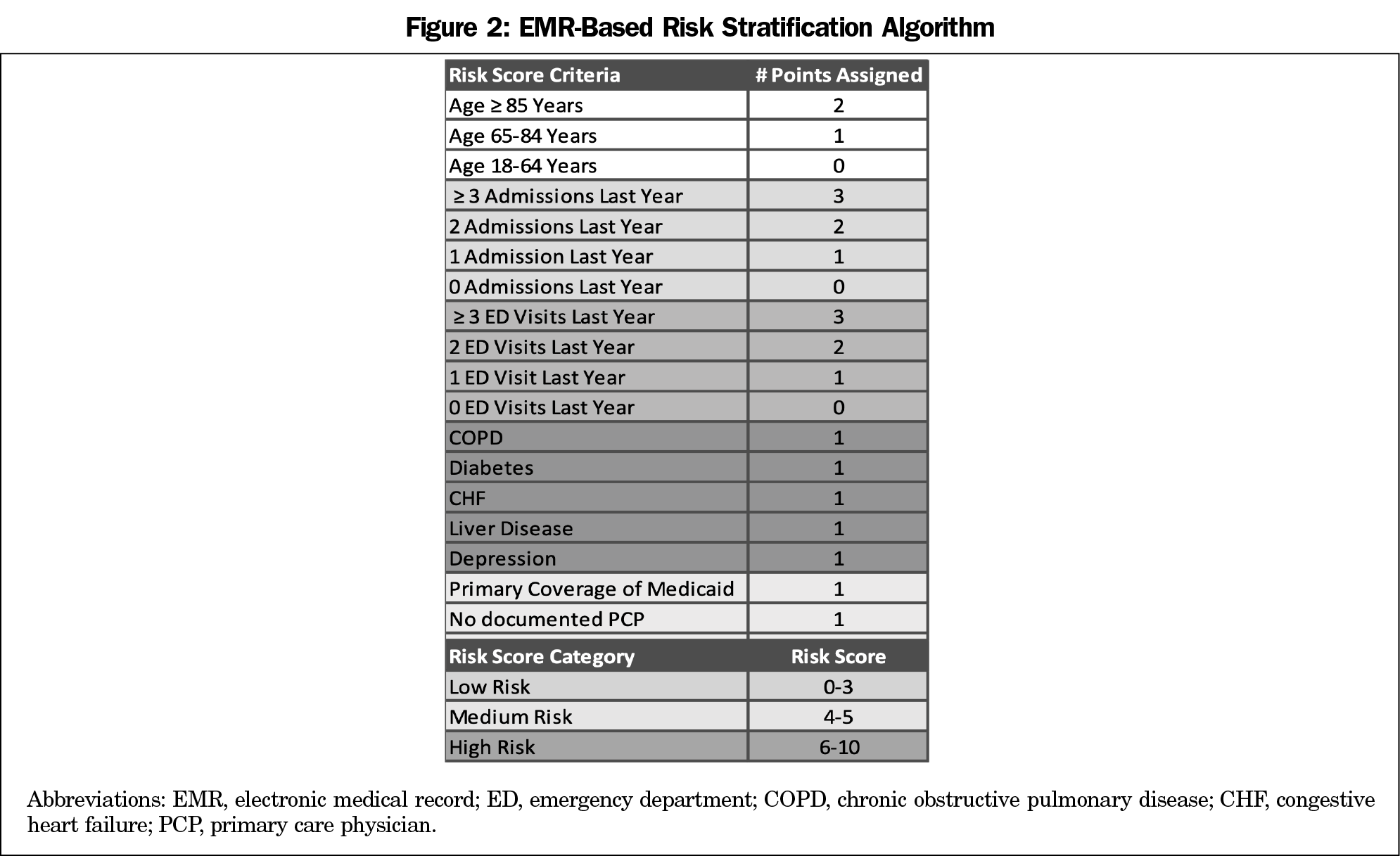
We created a tip sheet to help residents reassign patients based on complexity and continuity while prioritizing assignment to resident providers on their care team (Figure 1). If the patient was most recently seen by a different resident provider, we attempted to maintain functional continuity with that resident provider. The tip sheet also included a risk stratification algorithm to assign a score to each patient based on their medical and social complexity (Figure 2). This algorithm was developed by EPIC’s clinical team using evidence-based research and has an Area Under the Curve score ranging from 0.63 to 0.67. It compares to other models (eg, LACE and MELD) and indicates the patient’s risk of experiencing an adverse health event in the next year. In addition, we created a tracking tool in Microsoft Excel that was prepopulated with each resident’s patient list and reassignment guideline. As the resident documented each patient’s new PCP, the tool tracked the number of patients assigned to each future PCP and the number of patients each future PCP could still accept. While all residents were able to receive patients from graduating residents, higher-risk patients were assigned to rising PGY2s to enhance continuity. Upon entry, incoming interns were assigned lower-risk patients as part of their assigned patient panels. Patients were rarely reassigned to faculty. Our institutional review board determined that the project did not require full review.
Outcome Measures
Resident Satisfaction. In June of 2018, 2019, and 2020, after the panel reassignment process, the graduating PGY3s who were leaving the health system were surveyed via an online survey utilizing Qualtrics software. Questions were predominantly closed ended and addressed the reassignment timeline, availability of needed information, and level of confidence that their patients were appropriately reassigned. Residents were also able to provide additional comments.
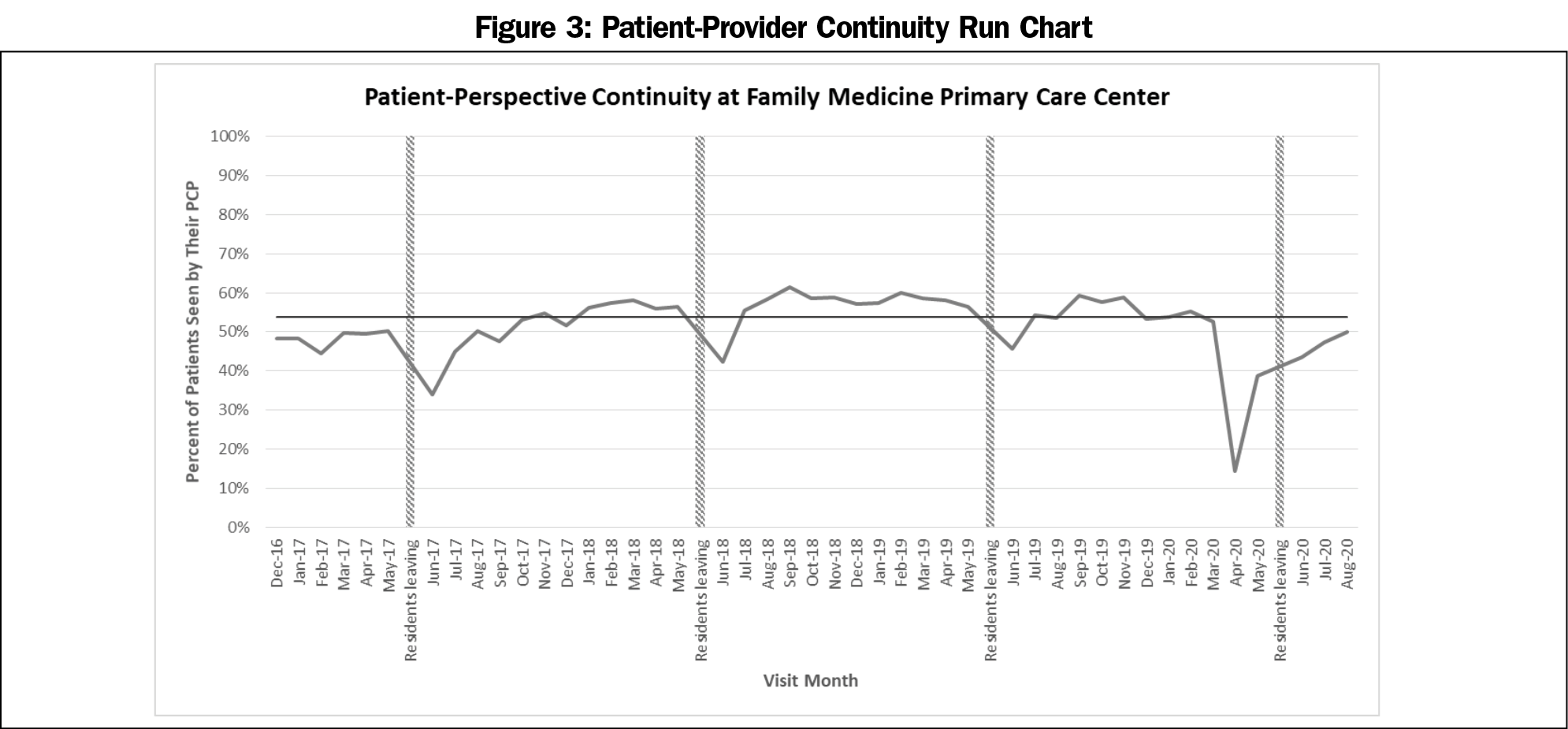
Patient-Provider Continuity. We tracked patient-perspective continuity data with a run chart reflecting the percentage of patients seen by their designated PCP.14 Baseline data are reflected from December 2016 to June 2017.
Resident Panels
The average panel size per PGY-3 residents was 320. The average number of patients each PGY-3 resident was asked to reassign (patients seen) was 188. The average number of patients per PGY-3 resident who required in-person handoffs due to controlled substance agreements was three.
Resident Survey. The survey response rate across the study period was 75% (15/20; four residents remained for fellowship during the study period and were not surveyed). Results are shown in Table 2.
Continuity Data
The patient continuity run chart is shown in Figure 3. The number of runs about the median is 13, which is below the expected lower limit of 17, reflecting nonrandom variation. The longest run about the median is 11, which is present twice, initially below the median and secondarily above the median. In addition, there are three shifts as well as one clear outlier in April 2020, at the outset of our clinics shutting down due to COVID-19.
The published literature includes a number of recommendations to improve the reassignment process, including identifying patient complexity, identifying the necessary clinical information to be transferred, utilizing a structured system, and communicating effectively with patients.10,15 Through this QI project, we moved from a tedious, unstandardized reassignment to an organized and well-received process that reflected an improvement in patient continuity. Our structured process, with designated time for the residents to complete their panel reassignment, enabled residents to receive in-person education and guidance from the QI director and data analyst. The risk stratification algorithm prompted residents to consider patient complexity and to more effectively distribute high-acuity patients among the successive residents. This acuity-based score also helped bring attention to patients who would benefit from an in-depth hand off to ensure attention to active or outstanding issues. By acknowledging the crucial role our residents play in the reassignment process, we were able to take advantage of resident knowledge of their patients and create a system that promotes resident ownership of their patient panels.
A variety of project limitations should be noted. This project took place in one residency program and may have limited generalizability to other health systems. Primary care providers in the EPIC electronic medical record were reassigned manually when PGY-3 residents graduated in June. This was time consuming and a likely explanation for the annual June dip observed in continuity, as patients’ documented PCPs may have been inaccurate at the time of their visit. A number of providers were away from the department for various periods of time during the study period, negatively affecting patient continuity. Finally, the COVID-19 pandemic profoundly impacted access to care, most significantly in April 2020. However, continuity data has steadily improved as we have reopened our clinics and enhanced our telemedicine access.
Future Directions
We have identified two primary areas that will require additional work: (1) linking patients to their family groups in an effort to maintain continuity of family-based care, and (2) expanding, optimizing, and structuring our warm hand-off process for high-acuity patients. We are encouraged by our results and plan to utilize continuous quality improvement to further enhance our year-end reassignment process.
Acknowledgments
Presentations: Dalrymple S, Sebring A, Compton R. There’s a Checklist for Everything Else: Developing a Standardized Process for Panel Reassignment. Lecture Discussion Presentation at the Society of Teachers of Family Medicine Annual Spring Conference. April, 2019, Toronto, ON, Canada.
References
- Toolkit for Empanelment in Teaching Clinics. UCSF Center for Excellence in Primary Care; 2018. https://cepc.ucsf.edu/sites/cepc.ucsf.edu/files/Toolkit%20_Empanelment%2018-0829.pdf. Accessed August 2020.
- Bodenheimer T, Ghorob A, Willard-Grace R, Grumbach K. The 10 building blocks of high-performing primary care. Ann Fam Med. 2014;12(2):166-171. doi:10.1370/afm.1616
- Chen EH, Bodenheimer T. Improving population health through team-based panel management: comment on “Electronic medical record reminders and panel management to improve primary care of elderly patients”. Arch Intern Med. 2011;171(17):1558-1559. doi:10.1001/archinternmed.2011.395
- Wajnberg A, Fishman M, Hernandez CR, Kweon SY, Coyle A. Empanelment in a Resident Teaching Practice: A cornerstone to improving resident outpatient education and patient care. J Grad Med Educ. 2019;11(2):202-206. doi:10.4300/JGME-D-18-00423.3
- Bennett K, Baxley E, Carter C, Stanek M. Organized continuity panel reassignment. J Grad Med Educ. 2011;3(3):404-407. doi:10.4300/JGME-03-03-28
- Donnelly MJ, Clauser JM, Tractenberg RE. Current Practice in End-of-Residency Handoffs: A survey of internal medicine-pediatrics program directors. J Grad Med Educ. 2013;5(1):93-97. doi:10.4300/JGME-D-12-00183.1
- American Academy of Family Physicians and American Family Physician News Staff. New Family Medicine Record in 2017 Match. Am Fam Physician.2017 Apr 15;95(8):478. https://www.aafp.org/afp/2017/0415/p478.html. Accessed March, 2020.
- Pincavage AT, Ratner S, Prochaska ML, et al. Outcomes for resident-identified high-risk patients and resident perspectives of year-end continuity clinic handoffs. J Gen Intern Med. 2012;27(11):1438-1444. doi:10.1007/s11606-012-2100-y
- Pincavage AT, Lee WW, Beiting KJ, Arora VM. What do patients think about year-end resident continuity clinic handoffs? A qualitative study. J Gen Intern Med. 2013;28(8):999-1007. doi:10.1007/s11606-013-2395-3
- Young JQ, Wachter RM. Academic year-end transfers of outpatients from outgoing to incoming residents: an unaddressed patient safety issue. JAMA. 2009;302(12):1327-1329. doi:10.1001/jama.2009.1399
- Lerner CF, Hamilton LJ, Klitzner TS. Improving year-end transfers of care in academic ambulatory clinics: a survey of pediatric resident physician perceptions. Med Ed Online, 17:1, 17815. Doi: doi:10.3402/meo.v17i0.17815
- Garment AR, Lee WW, Harris C, Phillips-Caesar E. Development of a structured year-end sign-out program in an outpatient continuity practice. J Gen Intern Med. 2013;28(1):114-120. doi:10.1007/s11606-012-2206-2
- Christiansen E, Hampton MD, Sullivan M. Patient empanelment: A strategy to improve continuity and quality of patient care. J Am Assoc Nurse Pract. 2016;28(8):423-428. doi:10.1002/2327-6924.12341
- Perla RJ, Provost LP, Murray SK. The run chart: a simple analytical tool for learning from variation in healthcare processes. BMJ Qual Saf. 2011;20(1):46-51. doi:10.1136/bmjqs.2009.037895
- Pincavage AT, Donnelly MJ, Young JQ, Arora VM. Year-End Resident Clinic Handoffs: narrative review and recommendations for improvement. Jt Comm J Qual Patient Saf. 2017;43(2):71-79. doi:10.1016/j.jcjq.2016.11.006




There are no comments for this article.