Video-based discharge instructions in the inpatient,1 adult and pediatric emergency room,2-6 and outpatient settings7 increase both retention of information and overall patient satisfaction. However, little is known about patient perceptions and acceptance of video tools to provide newborn care instructions to new parents.8 We sought to assess mothers’ postpartum sense of preparedness in caring for their newborn and overall satisfaction after receiving either video-based neonatal discharge instructions or equivalent instructions face to face by a resident physician.
BRIEF REPORTS
Use of Tablet Video for Delivery of Neonatal Discharge Instructions to First-Time Parents
Kristine L. Cece, MD, PhD | Jane E. Chargot, MD | Micheleen Hashikawa, MD | Melissa A. Plegue, MA | Katherine J. Gold, MD, MSW, MS
Fam Med. 2021;53(2):145-147.
DOI: 10.22454/FamMed.2021.551065
Background and Objectives: While video discharge instructions have been shown to improve retention of information and patient satisfaction, data are limited regarding patient perceptions of video tools.
Methods: We conducted a randomized controlled trial to assess self-rated comprehension and overall satisfaction with video versus face-to-face neonatal discharge instructions in first-time mothers.
Results: Video instructions were no different from face-to-face instructions, though there was a nonsignificant increase in confidence in caring for their newborn in the video group.
Conclusions: Broader use of technology may allow for a more standardized approach to patient education and improve efficiency for clinicians, without compromising patient satisfaction and confidence in caring for themselves and their dependents.
This was a randomized controlled, nonblinded trial of mothers delivering at a large academic hospital. Inclusion criteria were medically-stable postpartum primiparous, English-speaking women aged 17 years and older, on the low-risk family medicine delivery service. From February through June 2016, all patients who met inclusion criteria were approached, and if agreeable to participate, consented prior to randomization. Participants were subsequently randomized to receive face-to-face (control) or video discharge instructions (intervention) by choosing a sealed envelope opened by the resident physician on service on the day of patient discharge. The discharge instructions review feeding, normal urination and stooling, safe sleep, recognizing illness and jaundice, and postpartum depression. Intervention mothers viewed a prerecorded video that includes both auditory instructions and visual aids (ie, photographs) on a tablet computer at the bedside, while the control group received verbal face-to-face instructions by a resident physician. Both groups had the opportunity to ask questions of the resident in person after the instructions were given and received the same written pamphlet of discharge information.
After discharge presentations, participants completed an anonymous postintervention survey that identified to the investigators only whether they received video or face-to-face instructions based on the color of the paper on which the survey was printed (yellow: video; face-to-face: white). Participants were not aware of whether they were part of the control or the intervention group. The survey included demographics, and used a 5-point Likert scale to assess maternal self-confidence in caring for their newborn, satisfaction with discharge method, and level of understanding of the discharge instructions. The resident or nursing staff collected the surveys and returned them to the investigators without patient identifiers. Participants received a $5 gift card for their participation. We analyzed data using independent samples t tests and χ2 tests with patient satisfaction and patient self-rated preparedness in caring for their newborn as the outcomes of interest. The University of Michigan Institutional Review Board deemed this study exempt.
We randomized 57 participants to receive face to face discharge instructions (control, n=29) vs video discharge instructions (intervention, n=28). Eighteen control group surveys and 26 intervention group surveys were completed and returned. A total of 13 surveys (23% of those distributed) were not returned.
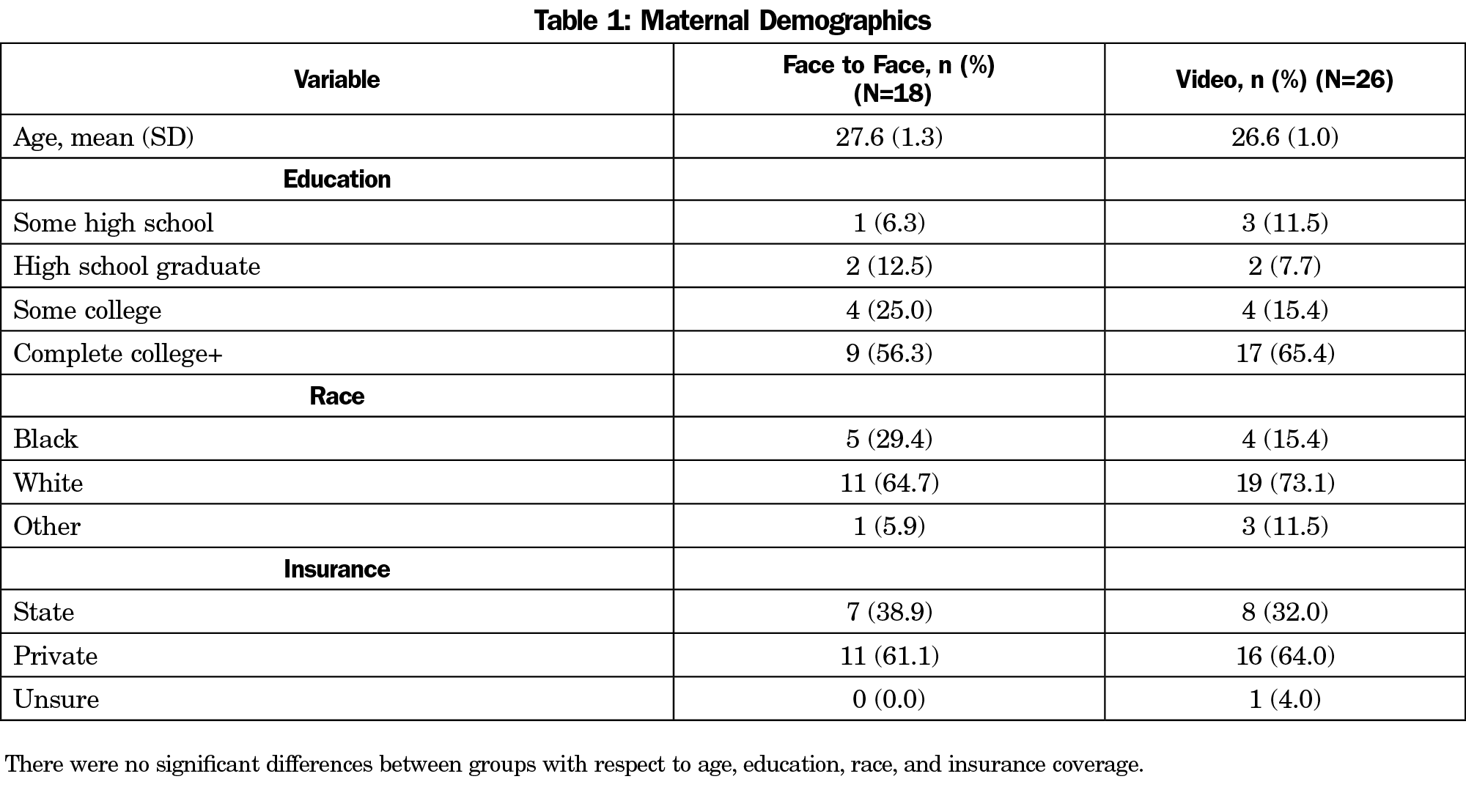
There were no differences between the control and intervention groups with respect to maternal age, education, race, and insurance type (Table 1).
There were no significant differences between groups in terms of overall satisfaction with the discharge method. Notably there were no patients who reported dissatisfaction with either method (control: 18% neutral, 18% satisfied, 64% completely satisfied; intervention: 4% somewhat satisfied, 31% satisfied, 65% completely satisfied; P=.11).
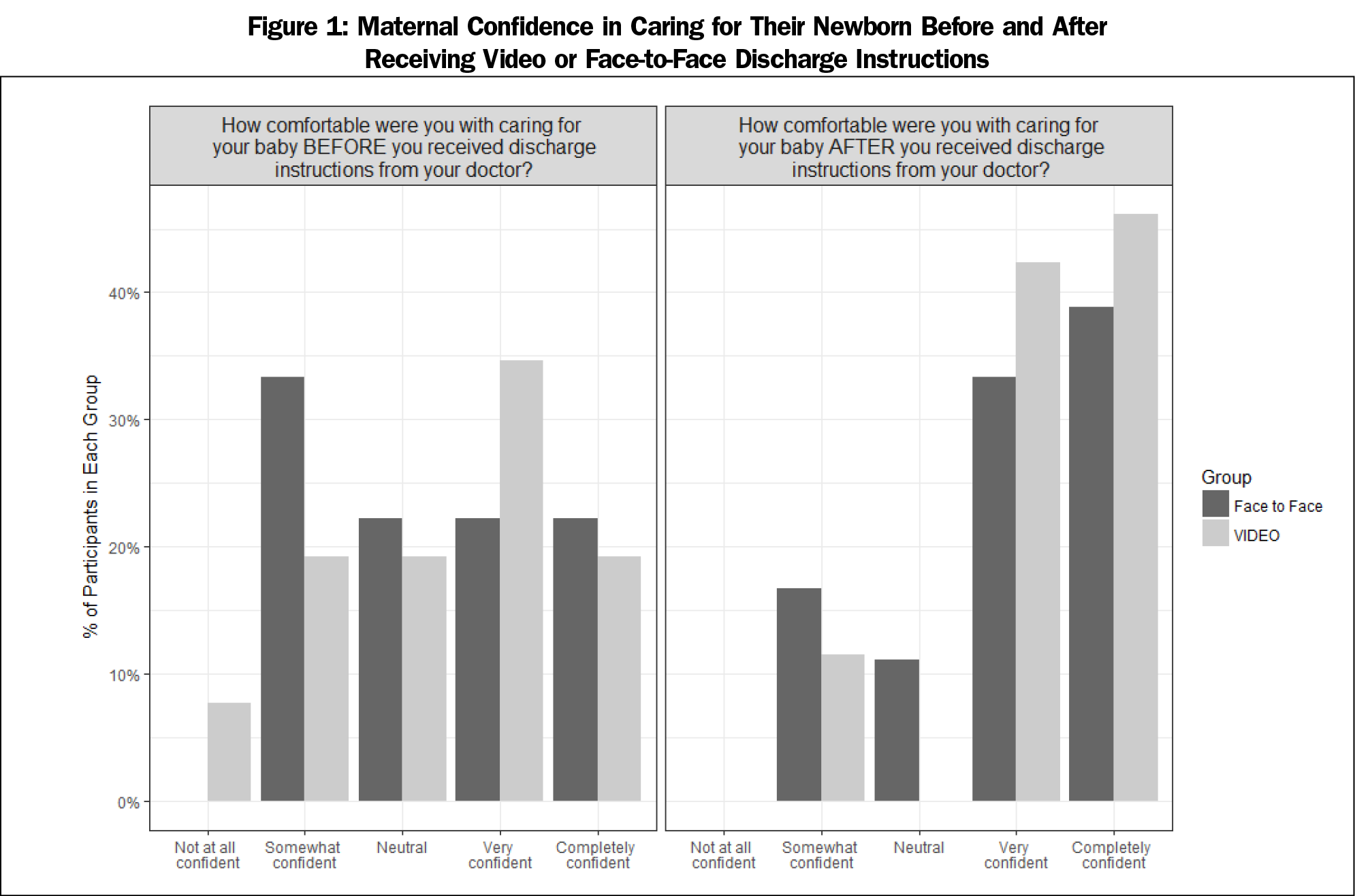
Both groups reported increased confidence in caring for their newborn after receiving discharge instructions (control before/after instructions given: 22%/11% neutral, 22%/33% somewhat confident, 22%/39% extremely confident; intervention before/after instructions given: 19%/0% neutral, 35%/42% somewhat confident, 19%/46% extremely confident). In the intervention group, women reported a greater increase in confidence, though not significant (P=.41, Figure 1).
There were no differences between the groups in terms of understanding the discharge instructions. In the face-to-face group, 12% of women were neutral, 12% understood most of the information, and 76% felt the instructions were completely understandable. In the video discharge group, 12% understood most of the information, and 88% felt the instructions were completely understandable (P=.27).
Our study is the first to show that use of video discharge instructions is equivalent to face-to-face instructions given by a resident physician with respect to maternal satisfaction and self-rated comprehension. Given the expansion of online access to parenting information and the time-saving potential of video instructions, these are important findings. Videos could substantially benefit residents and faculty in terms of increasing efficiency and providing consistent patient education. Our residents universally commented that they liked using the video instructions as the talks can be repetitive and time-consuming with a busy service.
The primary limitations in the study were a small sample size, the number of surveys not returned, and a lack of pre- vs postintervention data. The rate of nonreturn was much higher in the control group vs the intervention group, perhaps due to a lower level of engagement in those receiving face-to-face instructions. The study was also conducted in a relatively young cohort of mothers who may be more familiar with technology and more accepting of video instructions than the general population of childbearing women. Additionally, subjects were only surveyed after they received their discharge instructions rather than assessing their comfort in caring for their newborn before instructions were given, and again after the intervention. The retrospective nature of our survey could have led to recall bias. However, the results are encouraging in that they demonstrate that standardized patient education materials using technology such as videos are equivalent to face-to-face instructions for the outcomes studied, and have the added benefit of maximizing efficiency for the care team. The videos have been translated into multiple languages and have been expanded to all patients on the labor and delivery unit due to positive reception by both providers and patients. There is also potential for these videos to be available via internet link after discharge for patients to reference at home. Additional research on how implementing video instructions might change resident knowledge and comfort with newborn discharge care would be a useful addition to the field given the infiltration of digital patient education resources in primary care.
Acknowledgments
The authors thank the residents and nursing staff who assisted in acquiring survey data throughout the study period.
Financial Support: Incentive gift cards and a tablet computer were purchased by the Department of Family Medicine at the University of Michigan. No additional funding was received for this study.
Prior Presentation: This study was presented at the 2016 Society of Teachers in Family Medicine Annual Spring Conference in Minneapolis, Minnesota.
References
- Steinberg TG, Diercks MJ, Millspaugh J. An evaluation of the effectiveness of a videotape for discharge teaching of organ transplant recipients. J Transpl Coord. 1996;6(2):59-63. doi:10.7182/prtr.1.6.2.e720443244wxv3p1
- Chakravarthy B, Somasundaram S, Mogi J, et al. Randomized pilot trial measuring knowledge acquisition of opioid education in emergency department patients using a novel media platform. Subst Abus. 2018;39(1):27-31. doi:10.1080/08897077.2017.1375061
- Ismail S, McIntosh M, Kalynych C, et al. Impact of video discharge instructions for pediatric fever and closed head injury from the emergency department. J Emerg Med. 2016;50(3):e177-e183. doi:10.1016/j.jemermed.2015.10.006
- Saidinejad M, Zorc J. Mobile and web-based education: delivering emergency department discharge and aftercare instructions. Pediatr Emerg Care. 2014;30(3):211-216. doi:10.1097/PEC.0000000000000097
- Bloch SA, Bloch AJ. Using video discharge instructions as an adjunct to standard written instructions improved caregivers’ understanding of their child’s emergency department visit, plan, and follow-up: a randomized controlled trial. Pediatr Emerg Care. 2013;29(6):699-704. doi:10.1097/PEC.0b013e3182955480
- Choi S, Ahn J, Lee D, Jung Y. The effectiveness of mobile discharge instruction videos (MDIVs) in communicating discharge instructions to patients with lacerations or sprains. South Med J. 2009;102(3):239-247. doi:10.1097/SMJ.0b013e318197f319
- Schooley B, San Nicolas-Rocca T, Burkhard R. Patient-provider communications in outpatient clinic settings: a clinic-based evaluation of mobile device and multimedia mediated communications for patient education. JMIR Mhealth Uhealth. 2015;3(1):e2. doi:10.2196/mhealth.3732
- Logsdon MC, Davis D, Eckert D, et al. Feasibility of two educational methods for teaching new mothers: A pilot study. Interact J Med Res. 2015;4(4):e20. doi:10.2196/ijmr.4583
Lead Author
Kristine L. Cece, MD, PhD
Affiliations: Department of Family Medicine St. Joseph Mercy Health System, Brighton, MI
Co-Authors
Jane E. Chargot, MD - Department of Family Medicine, University of Michigan, Ann Arbor, MI
Micheleen Hashikawa, MD - Department of Family Medicine, University of Michigan, Ann Arbor, MI
Melissa A. Plegue, MA - Department of Family Medicine, University of Michigan, Ann Arbor, MI
Katherine J. Gold, MD, MSW, MS - Department of Obstetrics and Gynecology, University of Michigan, Ann Arbor, MI
Corresponding Author
Kristine L. Cece, MD, PhD
Correspondence: Department of Family Medicine, St. Joseph Mercy Health System, 7575 Grand River Ave, Suite 208, Brighton, MI 48114. 810-844-7950. Fax: 810-844-7955.
Email: Kristine_Cece@ihacares.com
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.