Background and Objectives: Gender-affirming hormone therapy (GAHT) is a key component in the primary care of transgender and gender-nonconforming (TGNC) people. However, physicians are hesitant to initiate GAHT, citing a lack of knowledge. We developed an educational program for medical students and sought to investigate whether medical students’ comfort and familiarity with GAHT could increase after a short interactive program.
Methods: Second-year medical students (N=54) at the University of Minnesota were recruited to attend an hour long interactive lecture on GAHT. We calculated mean change in pre- and postintervention 5-point Likert scale scores from a survey assessing comfort and familiarity with key concepts of GAHT to assess the effectiveness of the intervention.
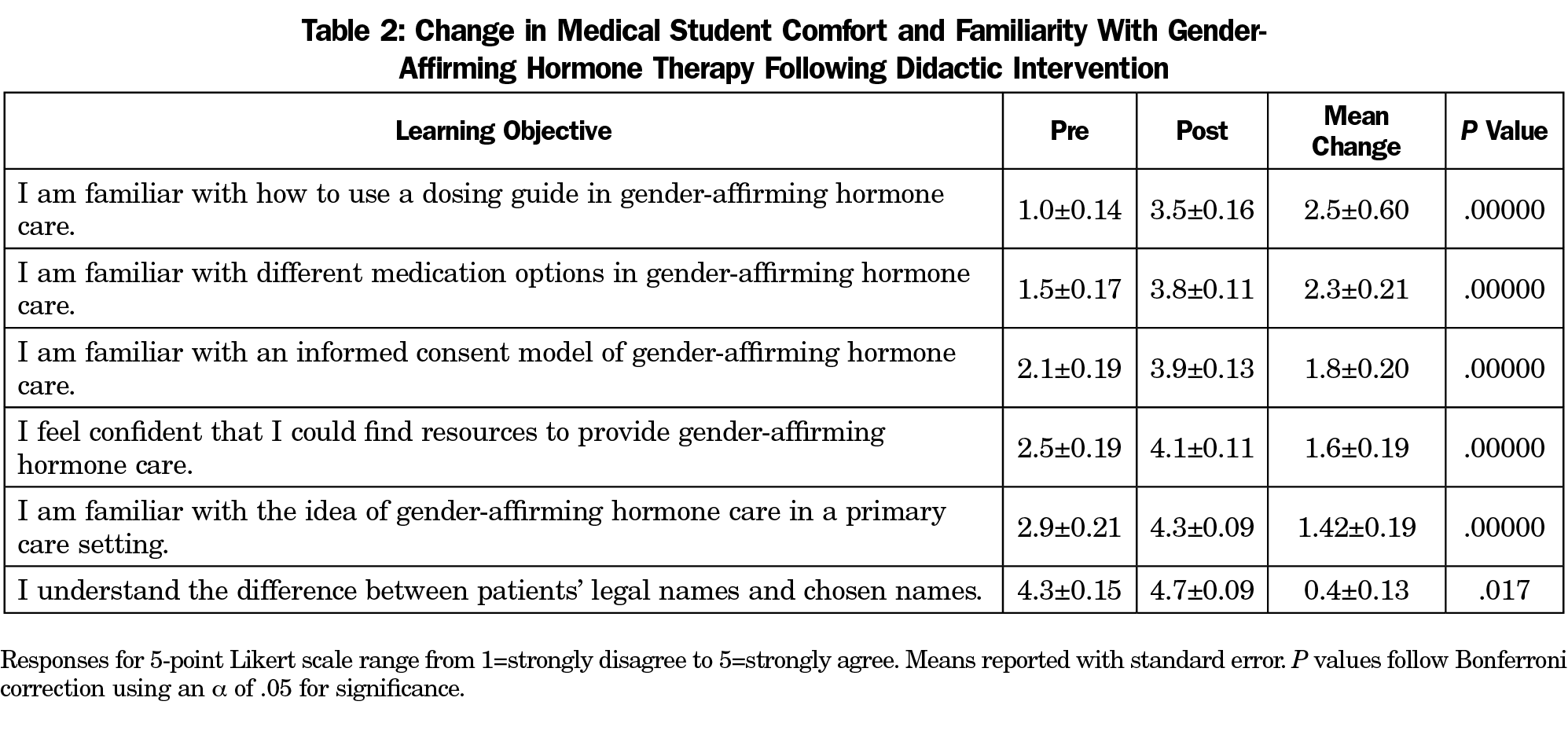
Results: Mean response score change increased significantly after the intervention around the use of chosen names (0.4±0.13, P<.017), the use of informed consent to initiate GAHT (1.8±0.20, P<.001), initiating and managing GAHT in the primary care setting (1.4±0.19, P<.001), medications used in GAHT (2.3±0.21, P<.001), and dosing (2.5±0.60, P<.001).
Conclusions: GAHT can be initiated and managed in a primary care setting. There is a push to introduce GAHT in the preclinical years. After participating in a short interactive lecture on GAHT, second-year medical students reported increased comfort and familiarity with GAHT. Inclusion of GAHT in the preclinical curriculum does not require significant teaching time and is important knowledge for all future physicians.
An estimated 1 million American adults identify as transgender and/or gender nonconforming (TGNC), representing 0.4% to 0.6% of the US population.1 Gender-affirming hormone therapy (GAHT) uses hormones to align secondary sex characteristics and gender identity. GAHT is a basic intervention sought by TGNC patients and is well within primary care providers’ scope of care.2 Primary care physicians can offer TGNC patients GAHT after informed consent in the outpatient setting without need for psychiatric or endocrine referral.4 However, physicians have been found to be reluctant to initiate or manage GAHT due to a lack of medical knowledge and training.3
Medications used in GAHT are commonly prescribed in the outpatient setting for other indications. Physicians first encounter these medications in the preclinical years. To effectively manage GAHT, physicians must receive adequate education on providing competent hormone care. Numerous studies have demonstrated preclinical training on the socially competent care of TGNC leads to better student understanding and comfort with TGNC patients.4-6 However, few studies have examined the effectiveness of educational interventions aimed at improving medical students’ comfort and familiarity with GAHT. In this study, we examined whether a 1-hour didactic and interactive lecture on GAHT could improve medical student comfort and familiarity with providing GAHT.
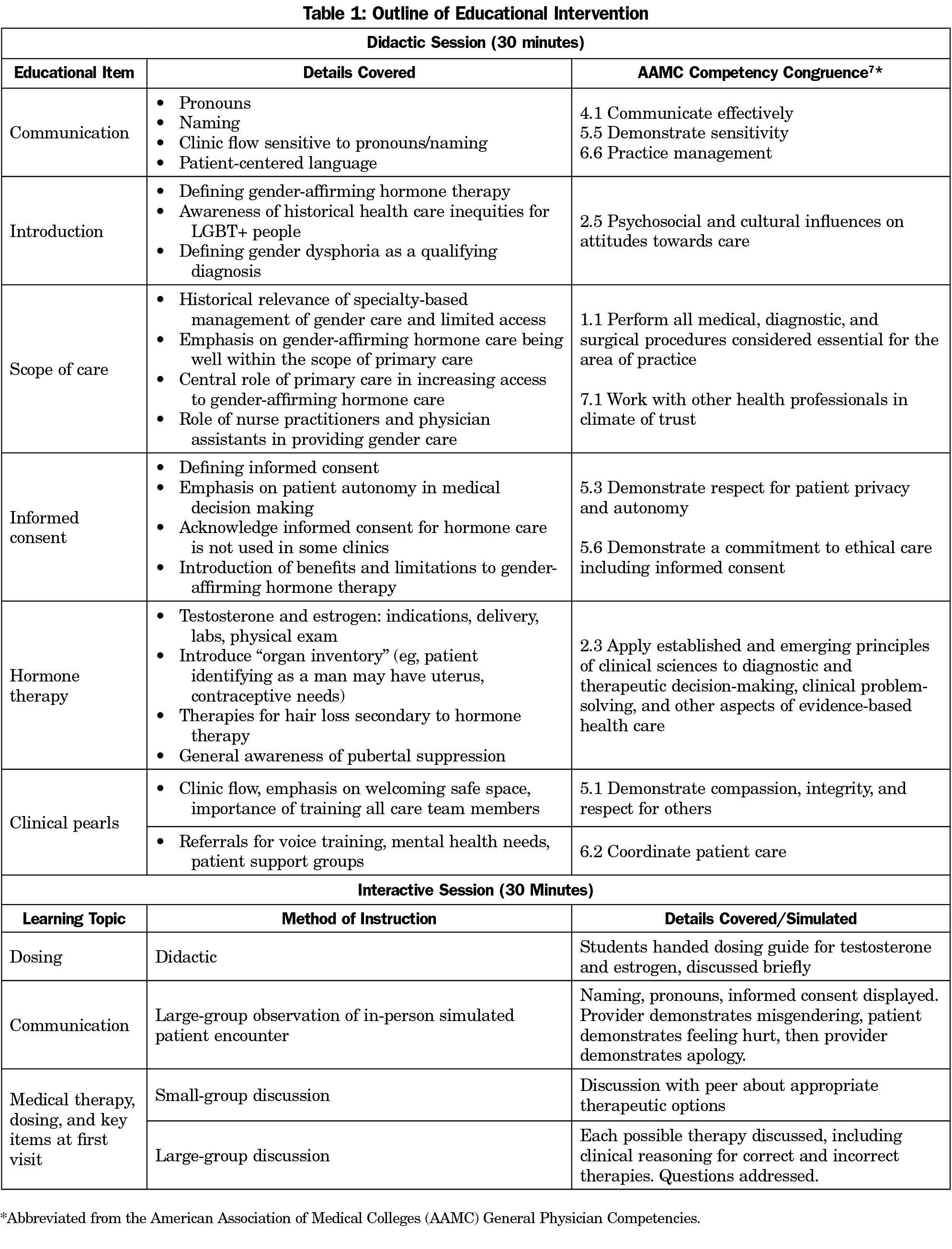
The University of Minnesota Institutional Review Board deemed this study exempt. We developed a 1-hour didactic and interactive lecture on GAHT (Appendix 1). The didactic portion of the lecture focused on the following objectives: (a) the scope of practice required to provide gender-affirming hormone therapy; (b) an informed consent model of care; and (c) the medical management of masculinizing and feminizing hormone therapy, including dosing of relevant medications (Table 1). The interactive portion of the lecture consisted of actors role-playing an office visit in which a physician initiated GAHT. The interactive lecture was designed to be stopped periodically so that audience members could be tested on concepts introduced, emulating real-time clinical decision-making.
One week prior to the optional lecture, an email announcement was sent to all second-year medical students at the University of Minnesota. Participants were given identical surveys that addressed self-perceived preparedness and comfort with learning objectives using a 5-point Likert scale (Appendix 2). The surveys were anonymous. We calculated pre- and postintervention mean scores and standard error for each survey item and then used a 2-tailed paired t test to determine significant differences between pre- and postintervention mean scores. To account for the multiple testing of the six survey items, a Bonferroni correction procedure was applied and P values were multiplied by six. We used an a of 0.05 to determine statistical significance.
Among 263 second-year medical students, all 54 (20.5%) who attended the lecture completed surveys. None of the surveys were omitted due to missing data or nonresponse. Comparing pre- and posttest survey responses, participants reported a significant increase in familiarity with GAHT dosing (mean change in response score=2.5±0.60, P<.001), common medications used in GAHT (2.3±0.21, P<.001), the use of informed consent in clinic to initiate GAHT (1.8±.20, P<.001), their confidence in finding resources to provide GAHT (1.6±.19, P<.001), providing GAHT in the primary care setting (1.4±.19, P<.001) and the difference between a legal and chosen name (0.4±.13, P<.017) after the intervention (Table 2).
Our single-institution study found that a didactic and interactive lecture on GAHT for second-year medical students resulted in significant increases in student comfort and familiarity with GAHT, including chosen names, the concept of GAHT in a primary care setting, use of informed consent to start GAHT, and the use and dosing of common medications used in GAHT. Topics discussed during the lecture, particularly the use of certain medications including spironolactone, testosterone, and GnRH agonists, were well-aligned with concepts introduced in existing endocrinology and renal curriculum and required only 1 hour of teaching time.
Our findings align with previous studies demonstrating increased trainee comfort with providing care to TGNC patients after an educational intervention.4-6 However, this study uniquely demonstrates increased trainee familiarity with GAHT, a basic element in the medical care of TGNC patients.
Participants reported significant growth surrounding their comfort with the use of medications used in GAHT and their dosing, suggesting participants were not aware which medications are used in GAHT but felt familiar after the intervention. Dosing is not routinely covered during preclinical years. However, students reported understanding the concept of dosing after the intervention. Participants felt comfortable with the difference between chosen and legal names before the intervention but there was still a significant increase in understanding after the intervention. Relatively high participant familiarity with naming could be attributed to prior education and exposure.
Our study had several limitations. This was a single-institution study with a small sample size, which limits the validity of our results. The study is likely subject to selection bias, as the lecture was optional and participants may have differences in baseline knowledge and motivation to learn about GAHT compared with nonparticipants. Further studies are needed to investigate the impact of educational interventions on actual trainee clinical performance using standardized measures and appropriate control groups.
Changes to medical school curricula are difficult given limited time for didactics in the preclinical years. We find that a 1-hour interactive lecture on GAHT increases medical students’ perceived familiarity and comfort with gender-affirming care in the primary care setting, use of informed consent to initiate GAHT, pharmacological management of GAHT, and chosen names. The elements of our curriculum could be introduced within an endocrinology unit or integrated into a more comprehensive LGBT+ curriculum. While the curriculum was designed for second-year medical students, certain elements may be adaptable for other trainees. Our findings demonstrate the feasibility of integrating GAHT into preclinical curriculum and can be used by other programs to build a holistic preclinical curriculum.
Acknowledgments
The authors thank Rachel Rudeen and Mary Tate for their support with the event, and Dr Anne Pereira, Dr Robert Englander, Lisa Skarbakka, and Tobias Donlon for their guidance and support in making changes to the curriculum.
Funding Statement: Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health Award Number UL1-TR002494. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Edmiston EK, Donald CA, Sattler AR, Peebles JK, Ehrenfeld JM, Eckstrand KL. Opportunities and gaps in primary care preventative health services for transgender patients: a systematic review. Transgend Health. 2016;1(1):216-230. doi:10.1089/trgh.2016.0019
- Deutsch MB, Feldman JL. Updated recommendations from the world professional association for transgender health standards of care. Am Fam Physician. 2013;87(2):89-93.
- Hashemi L, Weinreb J, Weimer AK, Weiss RL. Transgender care in the primary care setting: a review of guidelines and literature. Fed Pract. 2018;35(7):30-37.
- Cherabie J, Nilsen K, Houssayni S. Transgender health medical education intervention and its effects on beliefs, attitudes, comfort, and knowledge. Kans J Med. 2018;11(4):106-109. doi:10.17161/kjm.v11i4.8707
- Park JA, Safer JD. Clinical exposure to transgender medicine improves students’ preparedness above levels seen with didactic teaching alone: a key addition to the Boston University model for teaching transgender healthcare. Transgend Health. 2018;3(1):10-16. doi:10.1089/trgh.2017.0047
- Grosz AM, Gutierrez D, Lui AA, Chang JJ, Cole-Kelly K, Ng H. A student-led introduction to lesbian, gay, bisexual, and transgender health for first-year medical students. Fam Med. 2017;49(1):52-56.
- Englander R, Cameron T, Ballard AJ, Dodge J, Bull J, Aschenbrener CA. Toward a common taxonomy of competency domains for the health professions and competencies for physicians. Acad Med. 2013;88(8):1088-1094. doi:10.1097/ACM.0b013e31829a3b2b



There are no comments for this article.