Background and Objectives: Maternity care training is a standard requirement for all family medicine residents, and family physicians play a critical role in the US maternity care workforce. In 2014, the Accreditation Council for Graduate Medical Education (ACGME) updated the required obstetrical experience during family medicine residency training from a volume-based to a competency-based requirement of 200 hours (2 months rotation). This study aimed to determine if family medicine resident maternity care training experience differed after this change in requirements.
Methods: A nationwide survey of family medicine program directors was conducted as part of the 2019 Council of Academic Family Medicine Educational Research Alliance (CERA) survey, replicating a 2013 CERA survey to determine if there was a change in family medicine resident maternity care experience after the ACGME requirements update.
Results: The priority programs place on residents’ continuity deliveries and family medicine faculty attending deliveries decreased between 2013 and 2019. The reported number of continuity deliveries and vaginal deliveries performed by residents also decreased significantly between 2013 and 2019, yet the program directors’ estimate of the number of graduates going on to provide obstetric deliveries or pursue a maternity care fellowship did not change significantly. Programs reporting more than 25% of graduates continuing to conduct vaginal deliveries have reported similar numbers of vaginal deliveries per resident as in 2013.
Conclusions: The majority of family medicine residents are graduating with less delivery experience, and residency programs are placing less priority on continuity deliveries and modeling by family physician faculty following the 2014 ACGME Family Medicine Requirements update. This trend may have major implications on the comprehensive nature of our specialty and further widen gaps in the maternity care workforce. Further studies are needed to determine the impact on the competency of graduating family medicine residents in providing maternity care and for the long-term effects on the maternity care workforce.
The decline in the proportion of family physician in the United States who provide maternity care since 2000 has been well documented, with recent data showing fewer than 10% of family physicians currently practice maternity care.1-4 Some regions have very few family physicians who provide maternity care due in part to privileging constraints and malpractice rates.1,2,5 Family physicians also report that lifestyle considerations and difficulty finding jobs that include maternity care prevent them from providing maternity care in practice.3,6,7 These barriers may help explain the gap between the percentage of family medicine graduates intending to perform vaginal deliveries (23%) and the percentage of practicing family physicians currently performing deliveries (fewer than 10%).8 With a projected shortage of 9,000 obstetrician-gynecologists by 2030, family physicians can help fill a critical need in providing maternity care in the United States,9,10 particularly in rural and underserved communities.11 High-quality maternity care training is an important component to ensure that family physicians are prepared to provide maternity care in practice.
Maternity care training is a standard requirement for all family medicine residents,12,13 yet there continues to be debate regarding how much training should be required in family medicine residency,14-18 and programs provide varying levels of maternity care training.19-21 A study on Preparing the Personal Physician for Practice (P4) and length of training innovations suggests that expanded training may impact the scope of practice of family physicians.22 P4 graduates were more likely to perform vaginal deliveries than a national comparison group (19% vs 9%).22 In 2014, the Accreditation Council for Graduate Medical Education (ACGME) updated the family medicine residency training requirements in maternity care, shifting from a volume-based to a competency-based experience, with the intent of providing flexibility and promoting innovation.23 Prior to 2014, residents were required to perform a minimum of 40 deliveries, at least 30 of which were required to be vaginal, and at least 10 deliveries including continuity of antenatal and postnatal care. A previous study of maternity care training in family medicine residencies found that in 2013, 85.6% of programs reported that trainees graduated with more than 40 vaginal deliveries.24 Rather than performing a minimum number of vaginal deliveries, residents must now have at least 200 hours (or 2 months) of maternity care experience with some element of continuity of antenatal/postnatal care.
While many factors impact trends in residency education, this study sought to identify if there was a change in the maternity care training experience in family medicine residency programs following the updated 2014 ACGME requirements. To understand if these requirement changes impacted the family physician workforce’s contribution to maternity care, we also explored whether the change in requirements affected the number of graduates who go on to conduct routine vaginal deliveries and/or pursue fellowships in maternity care.
The national survey of family medicine residency program directors conducted by the Council of Academic Family Medicine Educational Research Alliance (CERA) provided the opportunity to replicate an earlier CERA survey about maternity care training24 to assess the potential impact of the 2014 requirement changes (see Appendix at https://journals.stfm.org/media/3850/fashner-appendix-cera-ob-comparison.pdf for the list of maternity care training questions).
The 2019 CERA steering committee evaluated questions for consistency with the overall subproject aim, readability, and existing evidence of reliability and validity. Pretesting was done on family medicine educators who were not part of the target population. The American Academy of Family Physicians Institutional Review Board approved this project in May 2019. The Lee Health Institutional Review Committee, the Florida State University Institutional Review Board, and the Healthcare Corporation of America Institutional Review Board also approved this project.
For the 2019 CERA program directors survey, all ACGME-accredited US family medicine residency program directors, as identified by the Association of Family Medicine Residency Directors (AFMRD), were eligible to participate. Email invitations including a link to the online SurveyMonkey survey were delivered to all program directors. Seven follow-up emails to encourage nonrespondents to participate were sent after the initial email invitation. There were 655 program directors at the time of the 2019 survey; 39 had previously opted out or blocked SurveyMonkey surveys. Therefore, the survey was emailed to 616 individuals. The overall survey response rate was 42.4% (261/616). Data were collected from May 2019 to July 2019.
The 2013 CERA survey protocol applied the same sampling and recruitment approach as 2019, except the survey invitations were sent out a total of three times. Data were collected from August 2013 to September 2013 and achieved a response rate of 56% (251/441).24
We analyzed data from the 251 surveys in 2013 and compared it to the 261 surveys completed in 2019 (both the 2013 and 2019 surveys contained unanswered items from the demographic or maternity care training questions). Descriptive analyses included three general program demographics questions (type of program, region, and community size) and eight maternity care-specific questions (six regarding curricular characteristics and two outcome measures). The outcome variables included the program directors’ self-reported estimations for the percent of graduates in the last 5 years who conduct routine vaginal deliveries in practice and the number of graduates who enter a maternity care fellowship (see Appendix for survey questions). We hypothesized that the number of deliveries per resident would be fewer in 2019 than in 2013. Since we believed deliveries would be lower, we also expected that the number of residents continuing deliveries after graduation would decrease over the same time period. We used χ2 tests to determine statistically significant differences between the categorical variables. We combined categories as in the 2013 study24 for some of the analyses. We completed statistical analysis using STATA 14.25
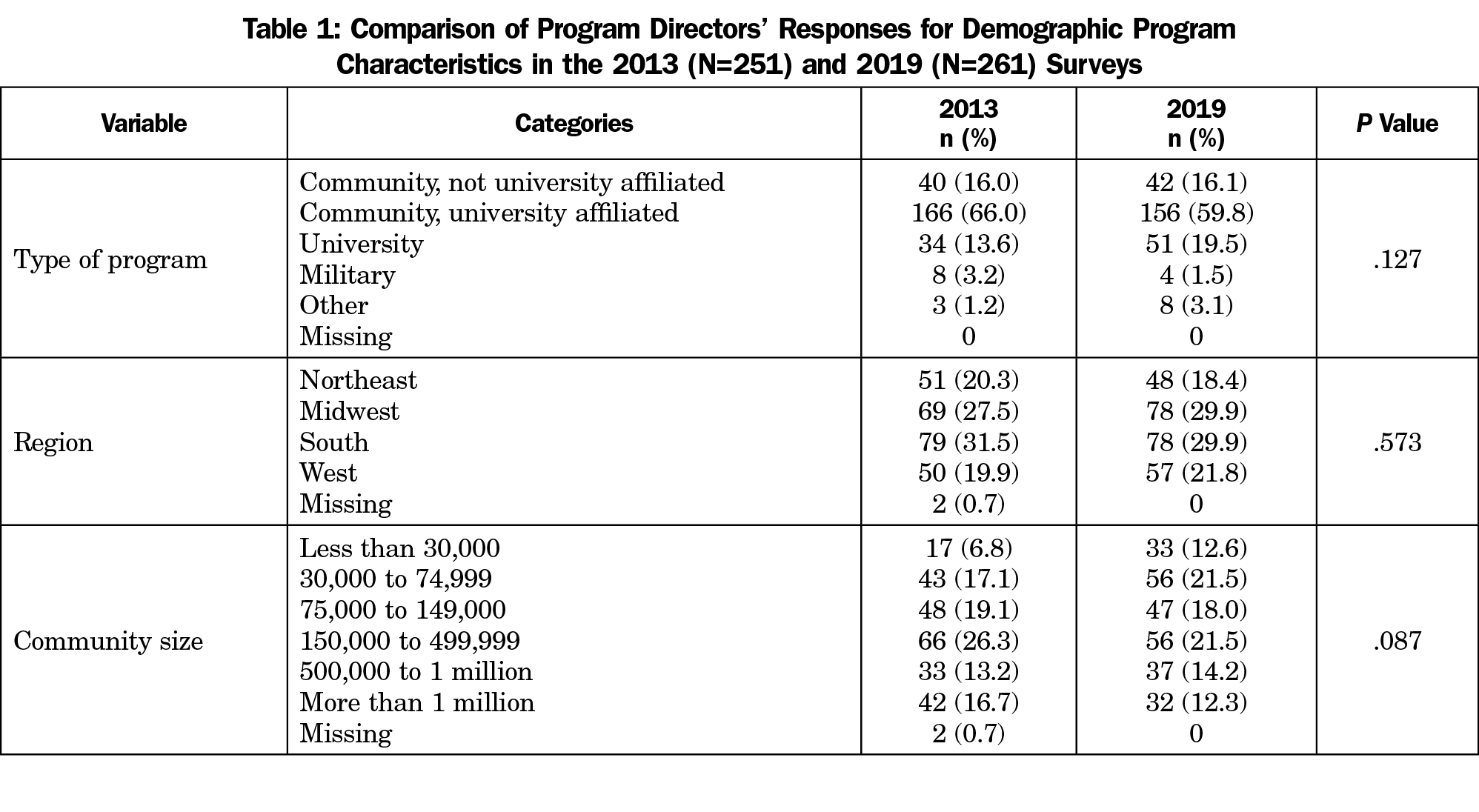
Comparison of the 2013 and 2019 surveys found that the demographic program characteristics reported by the program director respondents were similar in terms of type of program, region, and community size (Table 1).
We found no significant differences between 2013 and 2019 in the program directors’ estimate of the independence expected of residents on maternity care rotation or in whether a fellowship in maternity care was offered at the program (Table 2). However, as we hypothesized, the program directors’ estimation of the volume of both continuity and vaginal deliveries performed by residents significantly declined (each P<.001). In 2013, program directors estimated that 86.5% of programs’ trainees completed 10 or more continuity deliveries and 86.5% completed more than 40 vaginal deliveries; in 2019, this had dropped to 41.0% and 57.5%, respectively. The proportion of deliveries attended by a family physician and the priority given to continuity deliveries as rated by the program directors also decreased.
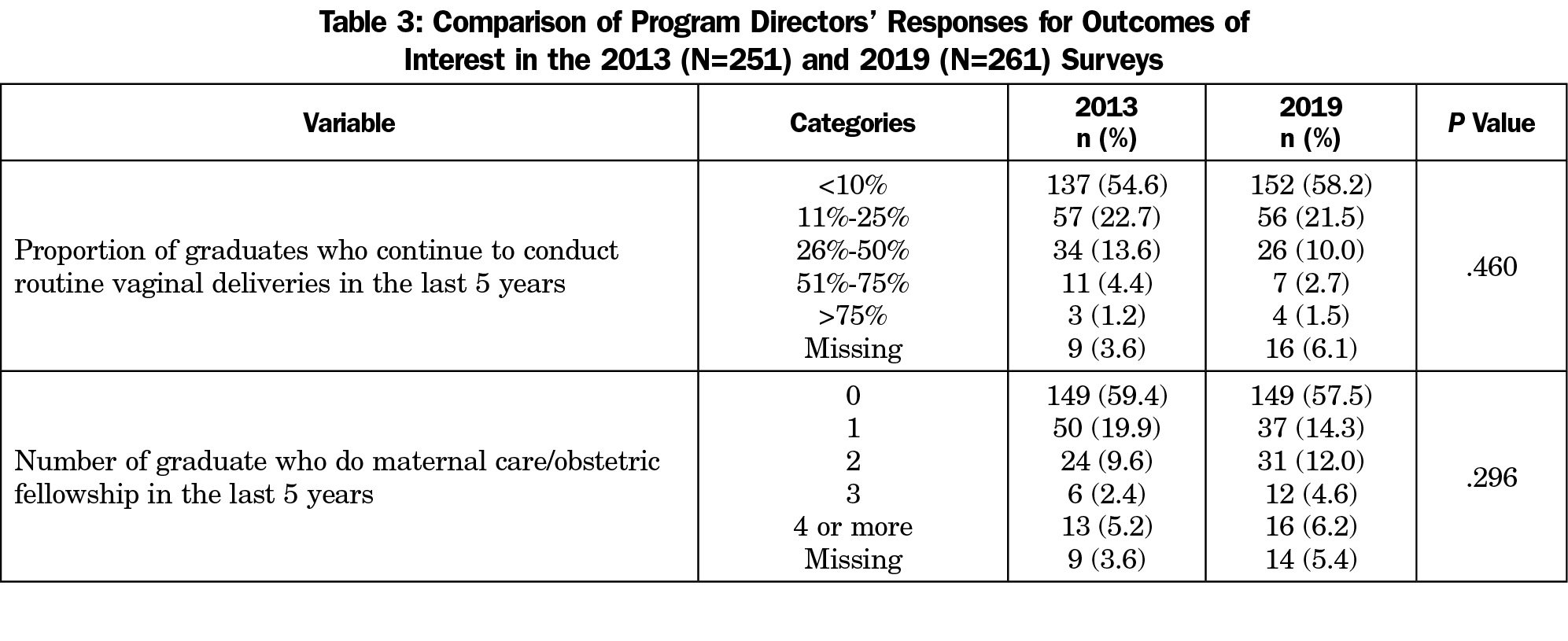
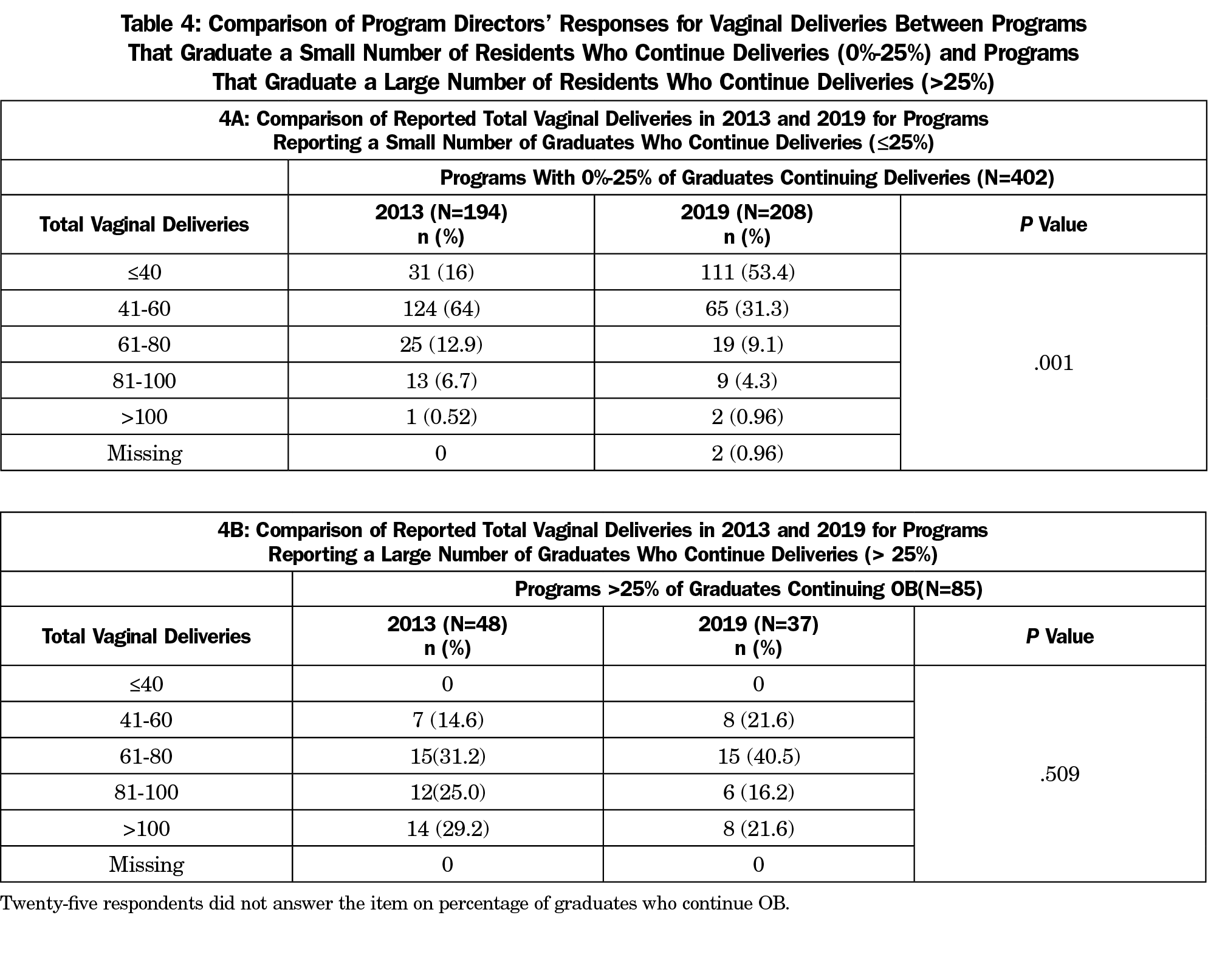
Overall, the outcomes of interest (proportion of graduates who were reported to have gone on to conduct routine vaginal deliveries in the last 5 years and the reported number of graduates who did a maternity care fellowship in the last 5 years) did not change significantly between 2013 and 2019 (Table 3). A subsequent analysis to investigate this unexpected outcome revealed that programs reporting more than 25% of graduates continuing to conduct routine deliveries reported no significant change in volume of vaginal deliveries per resident, while programs reporting fewer than 25% of graduates continuing to conduct routine deliveries reported a significant decrease in vaginal delivery volume per resident (Table 4). However, the proportion of program directors responding with a large number of graduates who continue to conduct routine vaginal deliveries (more than 25%) decreased from 19.2% (48 of 251) in 2013 to 14.2% (37 of 261) in 2019.
Training family physicians adequately in maternity care is important for the specialty to retain its full scope and comprehensive nature, as well as ensure access to maternity care amidst a growing obstetrician-gynecologist shortage. While the reported proportion of graduates who go on to routinely conduct deliveries or pursue a maternity care fellowship has not changed from 2013 to 2019, residency programs are placing less priority on resident involvement in continuity deliveries and in most programs, residents are graduating with less delivery experience. This trend could have major implications on the maternity care workforce and whether family medicine continues to include delivery care as a core part of our identity.
While this study did not ask what changes residency programs implemented in their program policies and expectations following the updated 2014 ACGME maternity care requirements, it appears that many programs have relaxed internal expectations regarding continuity delivery attendance and delivery volumes. Programs may find it challenging to support higher maternity care training volume for the same reasons fewer family physicians include maternity care in their practice.1-3,5-7 With fewer graduates practicing maternity care, programs have difficulty finding family medicine faculty actively providing maternity care in order to have them supervise residents. Some programs must balance resident bandwidth for covering all service obligations (ambulatory clinic, inpatient medicine, inpatient pediatrics and maternity care). In these programs, we may see relaxed internal maternity care training requirements because the burden of higher expectations was too great. Mentoring residents to consider a career as an academic family physician with maternity care and identifying advocacy efforts that will support residency programs’ maternity care training could allow programs facing these challenges to increase training volume.
While the updated ACGME requirements specify a need for competency-based goals for all educational areas, competency in maternity care is not explicitly defined. More research is needed to evaluate how programs define and evaluate for competency. It is plausible that programs with historically fewer graduates practicing maternity care require competency for only a basic level of maternity care, while programs with more graduates practicing maternity care define competency at an advanced level. A three-tiered system of maternity care training requirements has been proposed by the Council of Academic Family Medicine to achieve competency in increasing complexity of maternity care: ambulatory, comprehensive, and advanced maternity care.17 A residency program may offer one or multiple training tiers based on the training experience available at their site. If such a system were adopted by all family medicine residency programs, the transparency in maternity care training may offer a better guide for students motivated to include comprehensive maternity care in their future practice. Because this study does not have paired data from 2013 and 2019 surveys, we were unable to determine directly if programs with less graduates continuing maternity care decreased the maternity care experience in their program.
The number of family physicians practicing maternity care has been declining over the past several decades, and graduates have reported their intention to provide maternity care at higher rates than they report doing so in practice.8,26,27 Despite the decline in deliveries being performed by residents as reported by the program directors in this survey, the number of family medicine graduates in the last 5 years who went on to conduct routine vaginal deliveries in practice remained unchanged over the same time period. Medical students with a strong interest in providing maternity care may self-select into residency programs with high volume maternity care experience. Indeed, there are lists circulating on the internet to guide medical students in finding residency programs with strong maternity care training.28 Our finding that the reported percentage of graduates entering a maternity care fellowship did not change between the two survey years may indicate that residents believe their training is adequate, or the majority of those intending to continue maternity care in practice pursue fellowships. This raises the additional question of whether residents pursue fellowships in maternal care because they feel they did not receive sufficient training experience for the level of maternity care they wish to provide or to meet privileging requirements for future jobs. While previous studies identified privileging constraints as a barrier to practicing maternity care in family medicine,5 training volume requirements for obstetrical privileges are quite variable by institution.
Limitations
A limitation of this study includes sampling issues. Not all programs responded to the survey (less than 60% response rate) and different programs may have responded in 2013 compared with 2019. Although we can report general trends, we cannot determine if certain programs maintained high volume training between those years. Another limitation is that this data is based entirely on program director recall which may be unreliable in some areas (proportion of family medicine attendings at delivery, percent of graduates continuing to perform deliveries, etc). In addition, turnover in program director positions might impact the quality of the responses and constrain our ability to make comparisons over time. The other limitation of this survey type is that we do not capture resident maternity care experience directly, rather relying on the perception of the program director.
Family medicine is a comprehensive specialty founded on continuity of care.29 The family medicine maternity care model is valued by patients and their families,30 and protecting this option for patients while filling a growing gap in the maternity care workforce is an important strategy for our nation’s health. The findings in this study suggest family medicine residency training is losing emphasis on continuity maternity care, the modeling of maternity care by family physician attendings, and that many residents are graduating with less delivery experience. These graduates with less delivery experience may find it more difficulty to secure privileges for obstetrics,7 even if they would like to provide maternity care. Our findings raise important questions to determine the best way forward for maternity care training in family medicine: whether more family medicine maternity care fellowships are needed and/or if programs require additional advocacy and support for maternity care training. Institutionalizing the three-tiered scope of maternity care practice17 in the standardized competency assessments in family medicine training may be one way to substantiate advocacy efforts for universal family medicine obstetrics core privileges and remove barriers for competently trained family physicians who wish to provide family-oriented maternity care.
Acknowledgments
Disclaimer: This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare-affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
References
- Tong ST, Makaroff LA, Xierali IM, Puffer JC, Newton WP, Bazemore AW. Family physicians in the maternity care workforce: factors influencing declining trends. Matern Child Health J. 2013;17(9):1576-1581. https://doi.org/10.1007/s10995-012-1159-8
- Rayburn WF, Petterson SM, Phillips RL. Trends in family physicians performing deliveries, 2003-2010. Birth. 2014;41(1):26-32. https://doi.org/10.1111/birt.12086
- Barreto TW, Eden AR, Hansen ER, Peterson LE. Barriers faced by family medicine graduates interested in performing obstetric deliveries. J Am Board Fam Med. 2018;31(3):332-333. https://doi.org/10.3122/jabfm.2018.03.170427
- Barreto T, Peterson LE, Petterson S, Bazemore AW. Family physicians practicing high-volume obstetric care have recently dropped by one-half. Am Fam Physician. 2017;95(12):762.
- Goldstein JT, Hartman SG, Meunier MR, et al. Supporting family physician maternity care providers. Fam Med. 2018;50(9):662-671. https://doi.org/10.22454/FamMed.2018.325322
- Barreto TW, Eden A, Hansen ER, Peterson LE. Opportunities and barriers for family physician contribution to the maternity care workforce. Fam Med. 2019;51(5):383-388. https://doi.org/10.22454/FamMed.2019.845581
- Eden AR, Barreto T, Hansen ER. Experiences of new family physicians finding jobs with obstetrical care in the USA. Fam Med Community Health. 2019;7(3):e000063. https://doi.org/10.1136/fmch-2018-000063
- Barreto TW, Eden AR, Petterson S, Bazemore AW, Peterson LE. Intention versus reality: family medicine residency graduates’ intention to practice obstetrics. J Am Board Fam Med. 2017;30(4):405-406. https://doi.org/10.3122/jabfm.2017.04.170120
- Barreto T, Eden AR, Bazemore A, Peterson LE. Re: The numbers quandary in family medicine obstetrics. J Am Board Fam Med. 2018;31(1):168. https://doi.org/10.3122/jabfm.2018.01.170410
- Rayburn W. Who will deliver the babies? Identifying and addressing barriers. J Am Board Fam Med. 2017;30(4):402-404. https://doi.org/10.3122/jabfm.2017.04.170197
- Young RA. Maternity care services provided by family physicians in rural hospitals. J Am Board Fam Med. 2017;30(1):71-77. https://doi.org/10.3122/jabfm.2017.01.160072
- 12. Accreditation Council for Graduate Medcial Education. ACGME program requirements for graduate medical education in family medicine. https://acgme.org/Portals/0/PFAssets/ProgramRequirements/120_FamilyMedicine_2019.pdf?ver=2019-06-13-073936-407. Published 2019. Accessed February 17, 2020.
- Peterson LE, Fang B, Puffer JC, Bazemore AW. Wide gap between preparation and scope of practice of early career family physicians. J Am Board Fam Med. 2018;31(2):181-182. https://doi.org/10.3122/jabfm.2018.02.170359
- Worth A. The numbers quandary in family medicine obstetrics. J Am Board Fam Med. 2018;31(1):167-168. https://doi.org/10.3122/jabfm.2018.01.170378
- Young RA, Sundermeyer RL. Family medicine and obstetrics: let’s stop pretending. J Am Board Fam Med. 2018;31(3):328-331. https://doi.org/10.3122/jabfm.2018.03.180087
- Avery DM Jr, Reed MD, Skinner CA. Re: Family medicine and obstetrics: let’s stop pretending. J Am Board Fam Med. 2019;32(2):279. https://doi.org/10.3122/jabfm.2019.02.180329
- Magee SR, Eidson-Ton WS, Leeman L, et al. Family medicine maternity care call to action: moving toward national standards for training and competency assessment. Fam Med. 2017;49(3):211-217.
- Chen FM, Huntington J, Kim S, Phillips WR, Stevens NG. Prepared but not practicing: declining pregnancy care among recent family medicine residency graduates. Fam Med. 2006;38(6):423-426.
- Eden AR, Peterson LE. Challenges faced by family physicians providing advanced maternity care. Matern Child Health J. 2018;22(6):932-940. https://doi.org/10.1007/s10995-018-2469-2
- Hansen ER, Eden AR, Peterson LE. A qualitative study of trainee experiences in family medicine-obstetrics fellowships. Birth. 2019;46(1):90-96. https://doi.org/10.1111/birt.12388
- Ratcliffe SD, Newman SR, Stone MB, Sakornbut E, Wolkomir M, Thiese SM. Obstetric care in family practice residencies: a 5-year follow-up survey. J Am Board Fam Pract. 2002;15(1):20-24.
- Eiff MP, Hollander-Rodriguez J, Skariah J, et al. Scope of practice among recent family medicine residency graduates. Fam Med. 2017;49(8):607-617.
- Accreditation Council for Graduate Medical Education. ACGME Program requirements for graduate medical in family medicine: reasons behind the July 2014 revisions. https://www.acgme.org/Portals/0/PFAssets/ProgramResources/120_Reasons_that_Guided_the_Revisions.pdf?ver=2015-11-06-120653-853. Published 2015. Accessed February 17, 2020.
- Sutter MB, Prasad R, Roberts MB, Magee SR. Teaching maternity care in family medicine residencies: what factors predict graduate continuation of obstetrics? A 2013 CERA program directors study. Fam Med. 2015;47(6):459-465.
- Stata Statistical Software: Release 14 [computer program]. College Station, TX: StataCorp LP; 2015.
- Coutinho AJ, Cochrane A, Stelter K, Phillips RL Jr, Peterson LE. Comparison of intended scope of practice for family medicine residents with reported scope of practice among practicing family physicians. JAMA. 2015;314(22):2364-2372. https://doi.org/10.1001/jama.2015.13734
- Tong ST, Hochheimer CJ, Barr WB, et al. Characteristics of graduating family medicine residents who intend to practice maternity care. Fam Med. 2018;50(5):345-352. https://doi.org/10.22454/FamMed.2018.631796
- Stringfield S. 2018 update for "The List". Advancedfamilymedicine. https://advancedfamilymedicine.wordpress.com/2018/07/31/2018-update-for-the-list/. Published 2018. Accessed February 17, 2020.
- Saultz JW, Albedaiwi W. Interpersonal continuity of care and patient satisfaction: a critical review. Ann Fam Med. 2004;2(5):445-451. https://doi.org/10.1370/afm.91
- Price D, Howard M, Shaw E, Zazulak J, Waters H, Chan D. Family medicine obstetrics. Collaborative interdisciplinary program for a declining resource. Can Fam Physician. 2005;51(1):68-74.




There are no comments for this article.