Background and Objectives: The 2011 Alliance for Clinical Education panel recommended the development of a specialty-specific curriculum for all subinternships (sub-Is). A 2019 CERA survey found that 58% of family medicine clerkship directors agreed that a standardized curriculum would be helpful. The goal of this study was to explore attitudes and preferences regarding a national family medicine sub-I curriculum among a broad set of stakeholders.
Methods: Focus groups were conducted with medical students, residents, residency faculty, and undergraduate medical education faculty at the 2020 STFM Conference on Medical Student Education. Focus groups were transcribed, and a qualitative analysis was conducted with participants’ responses about the benefits and characteristics of a family medicine sub-I, recommendations for core sub-I skills/objectives, likelihood of using a national curriculum, and preferred student and program evaluation methods.
Results: There were four focus groups with a total of 24 participants. The following main themes emerged: the family medicine sub-I has distinctive characteristics from other sub-Is and provides unique benefits for students and residency programs, a standardized curriculum should allow for adaptability and flexibility, and the sub-I evaluation for the students and program should be specific and experience-focused. These themes were classified into specific subthemes.
Conclusions: The stakeholder emphasis on themes of uniqueness, adaptability, and specificity within evaluation will help educators structure a comprehensive framework for national recommendations for the sub-I curriculum. A well-designed family medicine sub-I may provide rigorous educational training for students and may also encourage career commitment to the discipline.
A 2011 Alliance for Clinical Education panel recommended that all specialties develop specific curriculum for subinternship (sub-I) experiences during the fourth year of medical school.1 National standards and resources can help individual schools by providing an already-constructed core curriculum designed to prepare students well for residency training, and help residency programs more accurately predict the baseline competence of their interns. The Association of Program Directors and Clerkship Directors in Internal Medicine, the Council on Medical Student Education in Pediatrics, and the Association of Pediatric Program Directors developed sub-I guidelines for internal medicine and pediatrics, respectively.2,3 The Society of Teachers of Family Medicine (STFM) has developed multiple iterations of a National Clerkship Curriculum—a renewable, web-based, peer-reviewed resource for the third-year core clerkship—but there is not yet a national standard for the sub-I rotation.4
In previous studies, residents and faculty identified the sub-I as one of the most important rotations to prepare a student for internship.2,5-6 Specifically, the family medicine sub-I would prepare students to be interns by fostering progressive responsibility for patient care, solidify career choice and provide networking opportunities, integrate medical school and residency program outcome measures, and emphasize the values, principles, and unique aspects of family medicine. A national curriculum for the family medicine sub-I would enable the specialty to achieve parity with and rigor equivalent to other disciplines while also ensuring resources comparable to those available for the core clerkship experience.
In 2019, STFM convened a task force to develop national curricular recommendations for the family medicine sub-I. Task force members included a broad constituency, with representation of student and resident learners as well as undergraduate (UME) and graduate medical education (GME) faculty. Representing the first publication on this issue, the task force’s 2019 CERA survey of family medicine clerkship directors found that 84% of responding schools required a sub-I in any discipline—including but not limited to family medicine. Furthermore, 58% of clerkship directors felt that national guidance and standards for the family medicine sub-I would be helpful.7 While the CERA study provided useful background information, it was limited only to an assessment of clerkship directors’ attitudes and constrained by its 10-item, closed-ended item survey format. Thus, the task force planned and conducted a set of focus groups consisting of UME and GME educators, residents, and students at the 2020 STFM Conference on Medical Student Education. The resulting qualitative analysis, presented here, allowed for a more in-depth understanding of this broad set of stakeholders’ attitudes and preferences regarding a national family medicine sub-I curriculum.
Setting and Participants
Authors conducted semistructured focus groups with medical students, residents, GME faculty, and UME faculty at the 2020 STFM Conference on Medical Student Education. The Family Medicine Sub-I Task Force invited participants to the focus groups through an email posted to the STFM MSE Collaborative listserv. One focus group was conducted over a breakfast session and included students, UME and GME educators. The remaining three focus group included a group each of students, UME educators, and GME educators. All focus groups were 60 minutes long. Participation was voluntary, and no compensation was provided. All participants gave verbal informed consent prior to starting the focus group. The Human Subjects Division at the University of Washington reviewed this study and determined it exempt (IRB ID: STUDY00009181).
Data Collection
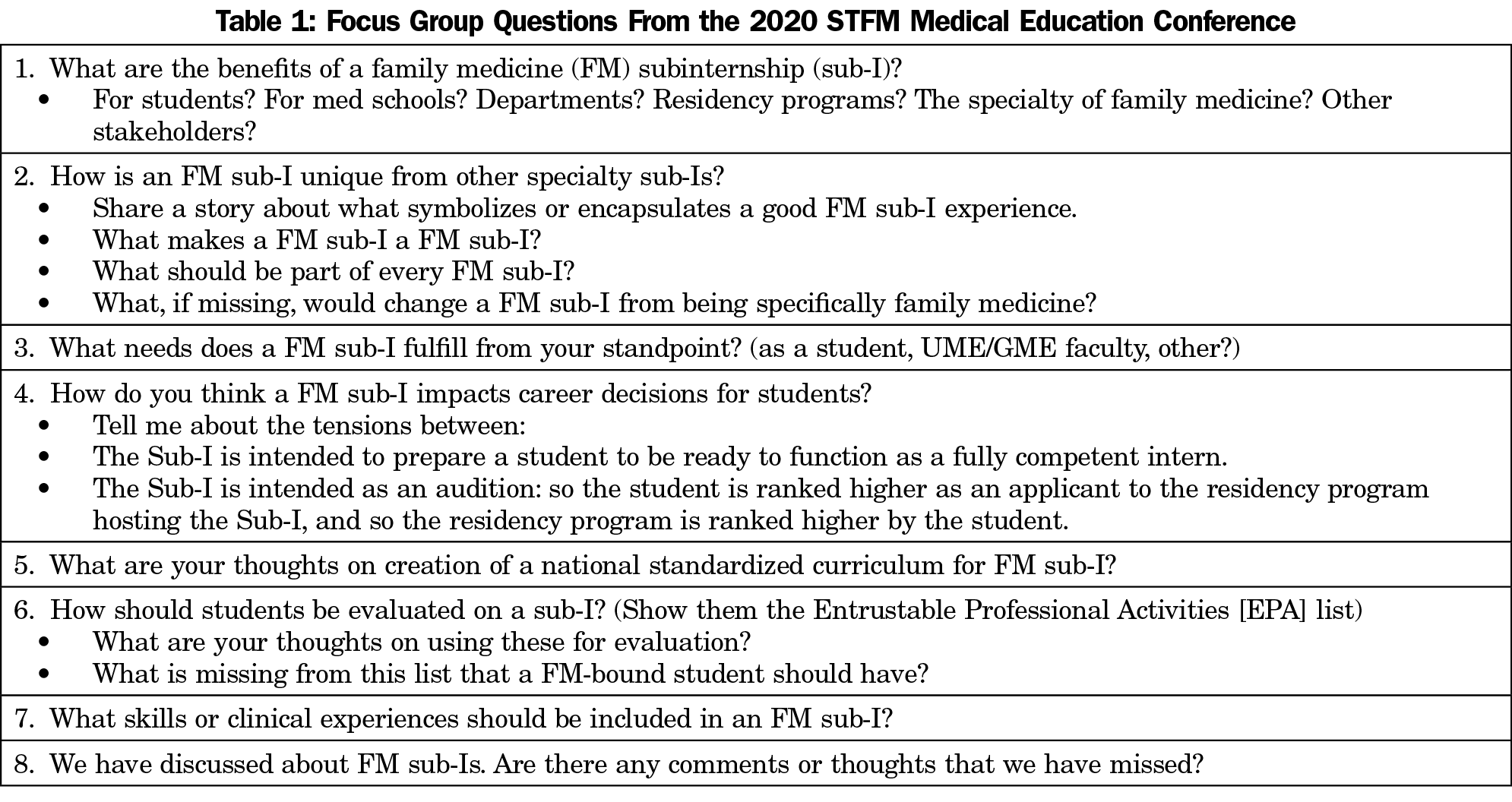
Two task force members facilitated each focus group: one faculty member and one student, to minimize bias. Facilitator pairs and participants were combined to ensure that there was no preexisting relationship. For preparation, facilitators used a guide with facilitator tips and standard questions (Table 1) developed by consensus. Questions explored the benefits and characteristics of existing and ideal family medicine sub-Is, recommendations for core goals and objectives in a standardized national curriculum, likelihood of using a standardized national sub-I curriculum, and preferred evaluation methods of both students and the sub-I curriculum.
Data Analysis
A commercial transcription service transcribed the individually-recorded focus group sessions. Each focus group facilitator pair-reviewed transcripts to confirm accuracy. All members of the authorship team were assigned to each review one transcript, independently identify emerging themes, and count theme frequency. One author (M.D.) used a content analysis approach8 to create an initial codebook based on the consistency of themes across groups. An authorship subgroup (M.D., T.S., D.B.) met via Zoom three times to revise the coding scheme and finalize four main themes, which were broken down into subthemes. Transcripts were reread independently to compare codes on an ongoing basis, add new codes where necessary, and discuss codes until there was universal consensus. All data management, coding, and analysis was done manually.
Participant Characteristics
There were a total of 24 participants in four focus groups: six GME educators in the GME group, five UME educators in the UME group, five students in the student group, and eight in the breakfast session with a variety of participants (one GME faculty, three UME faculty, two sub-I administrative staff, two students).
Perspectives on a Family Medicine Sub-I Among Multiple Stakeholder Groups
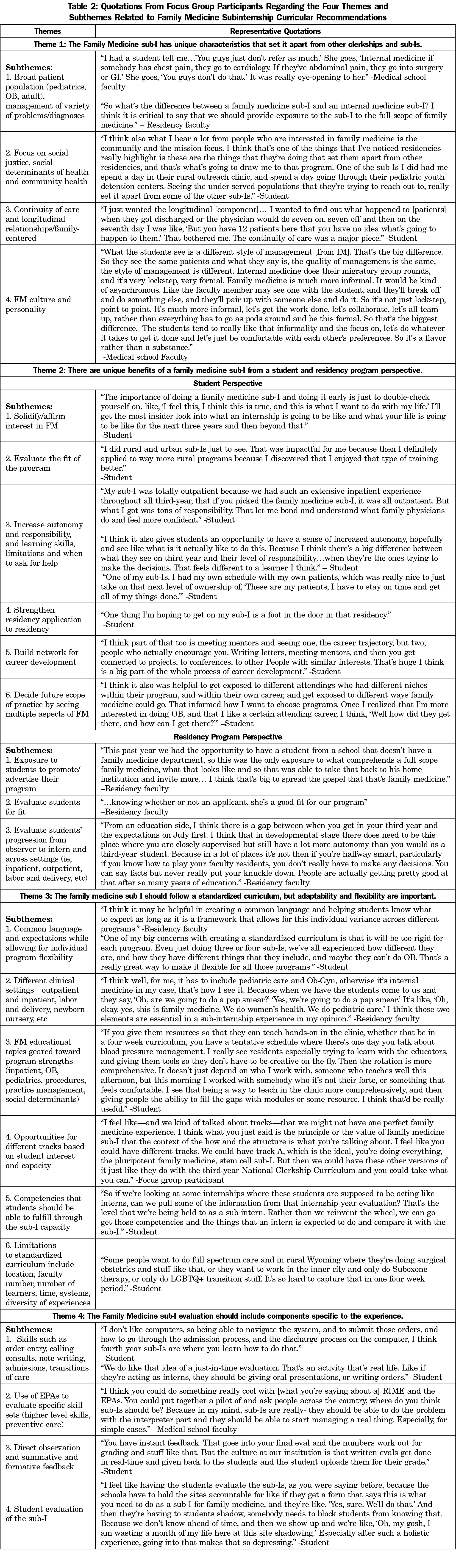
Four main themes emerged during the focus groups. Each theme identified core characteristics, benefits, and evaluation preferences of a family medicine sub-I, which then would inform the content of a standardized national sub-I curriculum. Each of these themes had subthemes, with representative quotations supporting them (Table 2).
Theme 1: The Family Medicine sub-I Has Unique Characteristics That Set It Apart From Other Clerkships and Subinternships. Many of the focus group participants identified that it is valuable for the family medicine sub-I to expose students to a broad patient population (ie, children, pregnant women, adults, older adults) while also teaching the diagnosis and management of a variety of problems and diagnoses. This is a key distinguishing feature of the family medicine sub-I from other sub-Is. The participants observed that their family medicine attendings on the sub-I placed an emphasis on social justice, the social determinants of health, and community medicine, which was distinctive from their experiences on non-family medicine rotations. Participants also witnessed the continuity of care and family-centered longitudinal relationships through the provider-patient relationships of attendings and residents, while on the family medicine sub-I. Additionally, focus group members remarked on the culture and personality of family physicians who teach on the sub-I, which contributed to the distinctive experience. By exposing students on the FM sub-I to the specialty’s unique characteristics, this could help not only solidify their career choices but also build the skills and knowledge that they would need to be future family physicians. From a curriculum development standpoint, it is important to ensure that these unique characteristics are represented in a national FM sub-I curriculum.
Theme 2: There Are Unique Benefits of a Family Medicine Sub-I From a Student and Residency Program Perspective. From a student standpoint, completion of a family medicine sub-I affirmed a student’s interest in the specialty and helped to evaluate the potential fit of a residency program. Participants described this rotation as a critical opportunity for students to gain autonomy and responsibility, learn their skills’ limitations, and identify when to ask for help. A family medicine sub-I helped students with their residency application, provided an opportunity for a letter of recommendation, and helped them to build a network for career development. Students also felt that the family medicine sub-I helped them to explore future scope of practice by seeing multiple aspects of the field, such as inpatient, outpatient, pediatrics, women’s health/obstetrics, procedures, sports medicine, etc. This broad exposure set the family medicine sub-I apart from sub-Is in other disciplines.
From a residency program perspective, a sub-I promoted and advertised the residency program and gave the program an opportunity to evaluate future applicants for fit. Residency faculty participants described the importance of the sub-I in allowing for the evaluation of students’ progression from observer to intern across a variety of settings (ie, inpatient, outpatient, labor and delivery, newborn nursery). A standardized curriculum would provide a framework for skill development and assessment of the sub-I learners as they progress during the rotation and across these multiple settings.
Theme 3: The Family Medicine Sub-I Should Follow a Standardized Curriculum, but Adaptability and Flexibility are Important. The majority of the focus group participants felt that the family medicine sub-I curriculum should not only foster common, specialty-specific language and expectations but also allow for individual program flexibility. While the sub-I should expose students to as many different clinical settings as possible, the educational focus of the family medicine sub-I should draw upon a program’s strengths, including inpatient, obstetrics, pediatrics, procedures, practice management, or community health. A couple of participants suggested that the sub-I curriculum could provide different tracks based on the strengths and capacity of the program, as well as student interest.
While there should be a standardized set of competencies that students can demonstrate after completion of a family medicine sub-I, participants recognized that the ability to teach these competencies may be influenced by the specifics of program location/region, number of faculty and learners, time, health system characteristics, resources, and/or diversity of clinical experiences. A few participants suggested that educational modules may assist students in supplementing their learning with topics that they did not have direct clinical exposure to during the sub-I.
Theme 4: The Family Medicine Sub-I Assessment Should Include Components Specific to the Experience. Participants expressed that the family medicine sub-I assessment of students should include tasks such as order entry, calling consults, patient documentation, admissions, transitions of care, and discharge planning. These core skills should be evaluated for an individual sub-I learner, and this evaluation should be included as part of a standardized FM sub-I curriculum. Furthermore, the AAMC’s Entrustable Professional Activities (EPAs)9 could be used to evaluate specific higher-level skill sets by facilitating direct observation and for providing summative and formative feedback. Focus group members also recommended that the standardized sub-I curriculum include a programmatic evaluation, which would be completed by students at its conclusion and provide questions specifically related to experiences necessary to achieve the course’s core competencies. This evaluation of the family medicine sub-I would help the task force to refine and revise the content and structure of a national family medicine sub-I curriculum in the future.
The identified themes from the focus groups convened at the 2020 STFM Conference on Medical Student Education provided robust information regarding defining and essential characteristics of the family medicine sub-I, as well as suggestions for a national curriculum. A national family medicine sub-I curriculum would embrace the field’s unique characteristics and principles, allowing students not only to reaffirm their interest in the specialty but also imagine their ideal, future scope of care. In a previous study,7 higher match rates in family medicine were positively associated with a sub-I requirement and with having a family medicine sub-I at a residency site. This association argues for the importance of having a family medicine sub-I, particularly at a residency site, to help reach the American Academy of Family Physicians’ goal of 25% of medical school seniors selecting family medicine as their specialty by 2030.10
Previous studies identified the skills of time management and prioritization, effective communication, and knowing when to ask for help as the most important on a sub-I; each of these is highlighted as a key focus of the pediatrics and internal medicine national sub-I curricula.2,3,6,11 While our focus group participants agreed that recognizing limitations and when to ask for assistance are important skills, they emphasized that the principle of student autonomy should be reflected in a standardized sub-I curriculum. It is essential that students take ownership of patient care responsibilities so that they can build the clinical and communication skills necessary for patient management. If a sub-I is considered one of the best preparatory courses for internship,2,5,6 then students need to practice the skills of prioritization, organization, and communication independently in a safe and supportive environment. A sub-I is the ideal rotation to give the student the independence to place orders and write prescriptions, write notes/discharge summaries, talk with and educate patients, communicate with consultants, and discuss care with the interprofessional team, while still under the direct supervision of residents and attendings. A standardized sub-I curriculum should include these core skills for residency preparation as well as place an emphasis on autonomy.
Similarly to the internal medicine and pediatrics curricula, a national family medicine sub-I curriculum should incorporate direct assessment of these higher-order sub-I skills.2,3 Our study participants supported direct observation as integral to student feedback, which has been shown in prior studies to allow for identification of educational deficiencies.12,13 Focus group participants also felt that the Entrustable Professional Activities (EPAs)9 may provide a framework for these higher-order sub-I skills assessments, which are also incorporated into the internal medicine sub-I curricula.2 A national family medicine subinternship curriculum will present a useable assessment framework and rubrics for the individual learner and the sub-I course, based on the EPAs, that can be adapted to a variety of patient care settings.
A standardized national sub-I curriculum with resources would benefit medical schools by providing an existing framework for a core curriculum designed to prepare students for residency; this core curriculum could also help residency programs more accurately assess their interns’ baseline competency. A national family medicine sub-I curriculum should include broad course objectives and experiences, which are focused on the core principles and skills of family medicine and may be easily adapted based on specific program resources. As such, the sub-I curriculum must highlight that the course should be taught by family physicians who embrace the core principles of the specialty, including social justice, the social determinants of health, and longitudinal and continuity of care. While all family medicine sub-Is should be built on the core principles central to the STFM National Clerkship Curriculum, our study supports the idea that a national curriculum should allow for flexibility in the specifics of its clinical structure and focus, as family medicine is practiced very differently across the country. Ideally, the sub-I should include exposure to at least two different clinical settings, such as outpatient clinics, inpatient wards, labor and delivery, and newborn nursery, whenever possible. However, these opportunities may be limited depending on the specific program. Therefore, interactive modules or cases may be used to fill any educational gaps.
There are several limitations to this study. First, as the analysis was conducted at a family medicine conference, focus group participants were more likely to be highly motivated educators and students likely to pursue family medicine. Selection bias may have influenced our results and could limit the generalizability of our findings. Additionally, while the identified themes provide a context and general framework for the specific competencies, learning objectives and assessment tools were not reviewed. While we discussed the importance for consistency between focus group leads, slight differences in interviewing styles may have influenced participants’ responses. Also, since medical educators could be difficult to identify, our recruitment through known communities of educators at each institution may have affected our sample of participants, thus resulting in sampling bias.
In conclusion, our findings revealed helpful recommendations for the development of a national family medicine subinternship curriculum. From the viewpoint of important stakeholders, these results aim to create a comprehensive framework for a standardized curriculum. The establishment of a family medicine sub-I curriculum is an opportunity to provide rigorous educational training for students, and at the same time, may support and encourage the growth of family medicine as a specialty.
Acknowledgments
Funding Statement: This project received financial support from the Society of Teachers of Family Medicine.
References
- Reddy ST, Chao J, Carter JL, et al. Alliance for clinical education perspective paper: recommendations for redesigning the “final year” of medical school. Teach Learn Med. 2014;26(4):420-427. doi:10.1080/10401334.2014.945027
- Vu TR, Angus SV, Aronowitz PB, et al; CDIM-APDIM Committee on Transitions to Internship (CACTI) Group. The internal medicine subinternship—now more important than ever: a joint CDIM-APDIM position paper. J Gen Intern Med. 2015;30(9):1369-1375. doi:10.1007/s11606-015-3261-2
- The Council on Medical Student Education in Pediatrics and Association of Pediatric Program Directors. Pediatric Subinternship Curriculum. 2009. Accessed November 2, 2020. https://media.comsep.org/wp-content/uploads/2019/01/30172802/COMSEP-APPDF.pdf
- National Clerkship Curriculum, 2nd ed. Society of Teachers of Family Medicine. 2018. Accessed November 2, 2020. https://www.stfm.org/teachingresources/curriculum/nationalclerkshipcurriculum/overview/
- Lyss-Lerman P, Teherani A, Aagaard E, Loeser H, Cooke M, Harper GM. What training is needed in the fourth year of medical school? Views of residency program directors. Acad Med. 2009;84(7):823-829. doi:10.1097/ACM.0b013e3181a82426
- Pereira AG, Harrell HE, Weissman A, Smith CD, Dupras D, Kane GC. Important skills for internship and the fourth-year medical school courses to acquire them: a national survey of internal medicine residents. Acad Med. 2016;91(6):821-826. doi:10.1097/ACM.0000000000001134
- Sairenji T, Stumbar SE, Garba NA, et al. Moving toward a standardized national family medicine subinternship curriculum: results from a CERA Clerkship Directors Survey. Fam Med. 2020;52(7):523-527. doi:10.22454/FamMed.2020.209444
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277-1288. doi:10.1177/1049732305276687
- The Core Entrustable Professional Activities (EPAs) for Entering Residency. Association of American Medical Colleges. Accessed November 2, 2020. https://www.aamc.org/what-we-do/mission-areas/medical-education/cbme/core-epas.
- Porter S. AAFP Hosts Launch of 25 x 2030 Student Choice Collaborative. 2018. Accessed January 30, 2019. https://www.aafp.org/news/education-professional-development/20180905twentyfiveby2030.html
- Angus S, Vu T, Halvorsen AJ, et al. What skills should new internal medicine interns have in July? A national survey of internal medicine residency program directors. Acad Med. 2014;89:432-435.
- Cydulka RK, Emerman CL, Jouriles NJ; The Council on Medical Student Education in Pediatrics and Association of Pediatric Program Directors. Pediatric Subinternship Curriculum. 2009Cydulka RK, Emerman CL,Jouriles NJ. Evaluation of resident performance and intensive bedside teaching during direct observation. Acad Emerg Med. 1996;3(4):345-351. doi:10.1111/j.1553-2712.1996.tb03448.x
- Li JT. Assessment of basic physical examination skills of internal medicine residents. Acad Med. 1994;69(4):296-299. doi:10.1097/00001888-199404000-00013



There are no comments for this article.