Background and Objectives: Many United States military personnel are not full-time service members. Because of their part-time service, these veterans may not self-report their military service during medical visits. Consequently, past military service can be overlooked when taking a social history. We developed a case to provide preclinical medical students patient interview experience wherein the diagnosis relied on identifying past military service. Our objective was to determine if medical record write-ups included social history details about occupational information after this innovation.
Methods: We conducted this case discussion in small groups during year 1 of medical school. We analyzed clinical skills examination write-ups before and after the case discussion to determine if the social history included occupational issues.
Results: Initial results showed increased occupational issues as potential diagnoses or contributing factors.
Conclusions: This case methodology specifically raised awareness of health issues related to military service and generally increased students’ likelihood of identifying occupational risk factors when conducting the social history. The template for this military case will allow us to develop additional cases focusing on different occupational health issues to complement other organ systems blocks.
For 2 decades, the United States military has been involved with conflicts around the world. Many military personnel are part-time service members, consisting of Reserve or National Guard forces.1 These veterans may not identify as part of military culture,2,3 their service may not be brought up as a normal part of the medical history. Additionally, the growing number of women serving is also overlooked.4
Connecting aspects of service to a medical condition facilitates appropriate care.5,6 For many US medical students, clinical rotations at a Veterans Administration Medical Center (VAMC) exposes them to these conditions. However, not all veterans access care at a VAMC and not all medical schools are affiliated with a VAMC. With the increasing numbers of veterans, medical schools need to prepare students for veteran care.2
Military history is part of an extensive social history. Therefore, course leaders introduced the expanded social history in our preclinical beginning doctoring course.7,8 The expanded social history challenges providers to incorporate more elements of a patient’s social context including an awareness of military history.
Military medicine educational modules have been developed;9-11 however, they primarily focus on mental health issues. Therefore, we developed a patient case wherein the diagnosis relied on identifying past military service. Our objective was to determine if medical student write-ups following a standardized patient encounter included a more extensive social history on the Objective Structured Clinical Exam (OSCE).
Curriculum
Our Patient Centered Care course teaches preclinical medical students essential clinical skills in small groups of seven or eight students with a practicing physician (tutor). Groups meet for 3 hours every week the first 3 semesters (18 months) of medical school. Each session introduces a new skill students practice along with case-based clinical reasoning, which is coached by tutors. At the end of each semester, a comprehensive OSCE utilizing standardized patients is given to students.
Military Case
Medical students and faculty members from the military medicine interest group partnered with course leaders to write a case of a soldier suffering from chronic cough between deployments. Members of the military medicine interest group were all veterans. The case was constructed to provide thorough, realistic detail of the soldier’s experience including work duties that led to environmental exposure.
Small Group Sessions
Tutors were trained on the military case and had the opportunity to clarify relevant details during their weekly meeting. In small groups, medical students interviewed their tutors, who were portraying the veteran. Students constructed a differential diagnosis. After discussion of their diagnosis, tutors provided the case details to identify missed elements. As a group, they were able to identify key details important for their reasoning and clinical decision-making.
Assessment
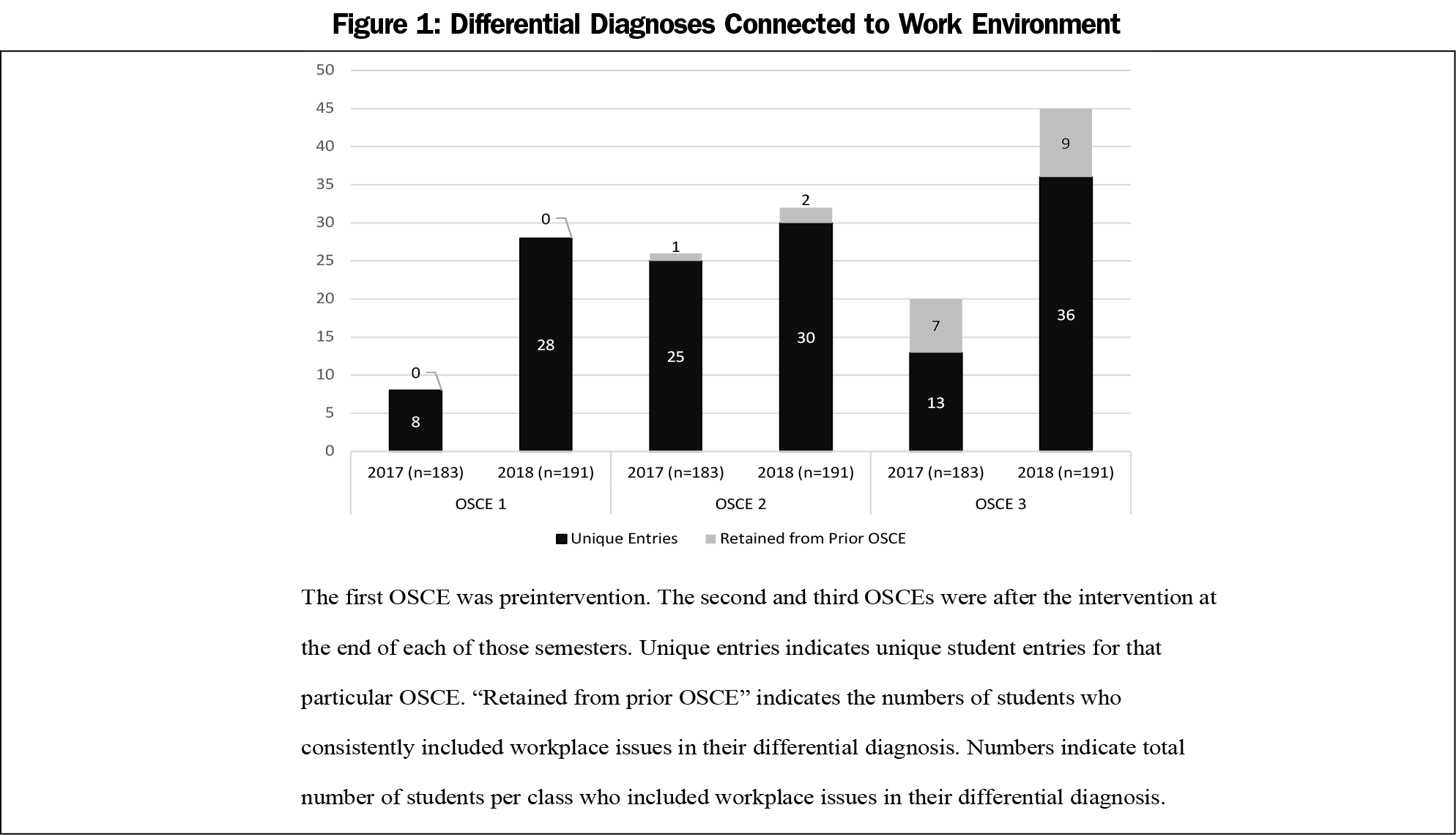
Students participated in three OSCEs. One was conducted before the students experienced the military history case. Two OSCEs were conducted after the military history case (3 months later and 9 months later).
During these OSCEs, students interviewed standardized patients, then wrote a three-item differential diagnosis with three items of supporting evidence for each diagnosis. One of the authors (Z.M., who was the course manager) analyzed supporting evidence to identify if students connected their differential diagnosis to any occupational hazards. For each student on each OSCE, frequency of occupational environments in supporting evidence was recorded. Connection to the occupational hazard required direct connection. For example, stating the patient may have inhaled a substance was insufficient while stating the patient inhaled a substance while working would be recorded. Unique entries were defined as at least one item of supporting evidence connected to the patient’s occupation. Retained entries were defined as students who linked the patient’s diagnosis to their occupation on subsequent OSCEs.
We conducted independent t tests to compare results between OSCEs. We conducted analysis using IBM SPSS v 26 (Armonk, NY). Our institutional review board deemed this study exempt.
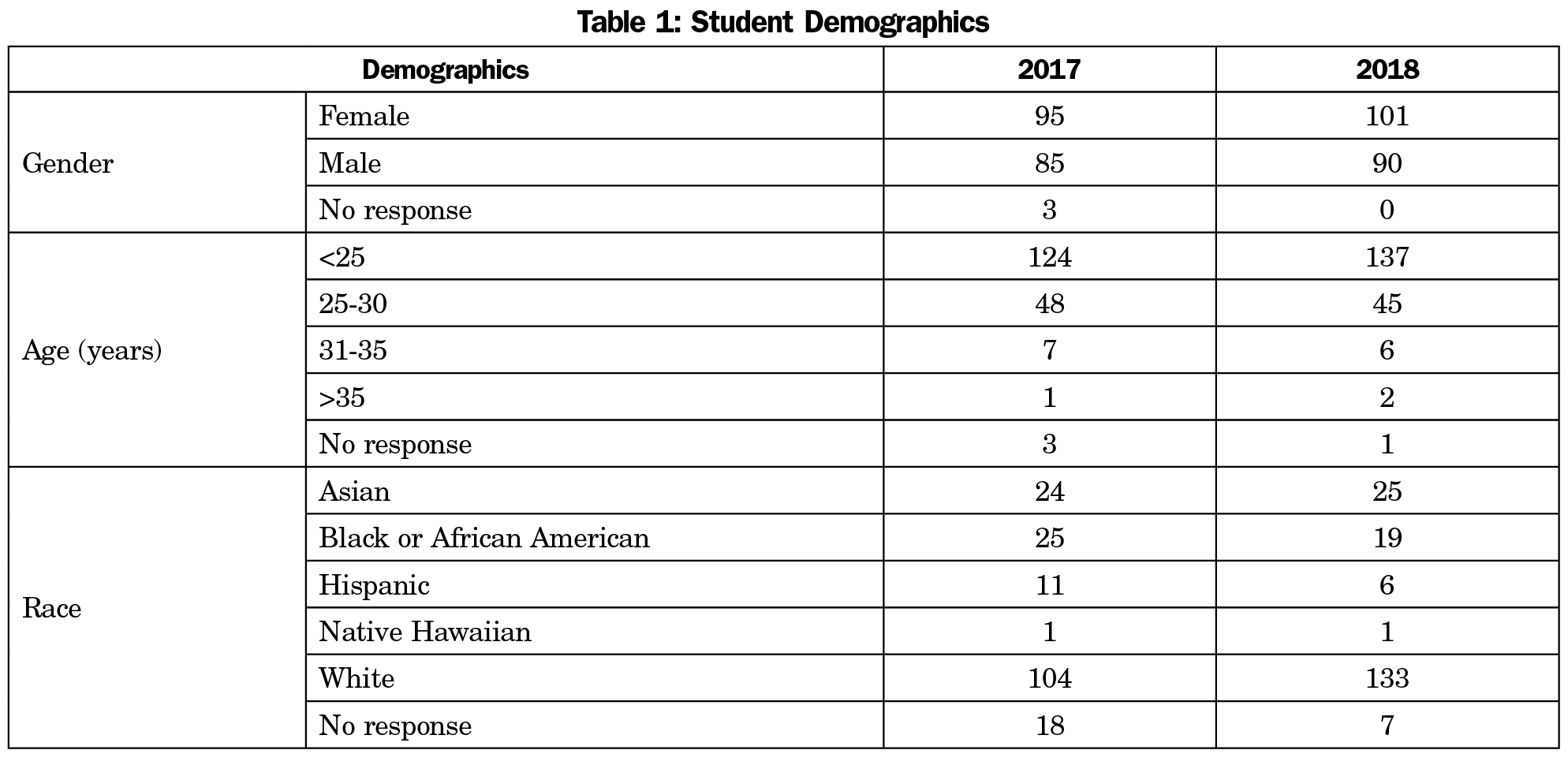
Demographic data from two cohorts of first-year medical students from 2017 (n=183) and 2018 (n=191) are detailed in Table 1.
In 2017, occupational health concerns documented in the students’ clinic note preintervention was weak (8 of 183). There was a significant improvement in the next OSCE after the introduction of the military case (t= -3.23, P=.001, Figure 1). On the final OSCE, documented occupational health concerns declined (t=.95, P=.033).
During 2018, the preintervention OSCE was improved (28 of 191). Only two students from the first OSCE included occupational connections postintervention, but there were more unique entries across each succeeding OSCE (Figure 1).
Although both cohorts had fewer documented occupational health concerns in the third OSCE, both groups showed improvement postintervention. In comparing the first OSCE to the final, the cohort in 2017 was significantly improved (t=2.79, P=.006).
Our innovation successfully introduced how military experiences impact veterans’ health. Results from 2 years of OSCEs indicate modest improvements in citing occupational factors as potential causes of patient’s symptoms.12
We had hoped to see continuity from OSCEs two and three after the intervention. However, that did not occur. We can only speculate that the students focus solely on topics they learn during the semester, which may have resulted in a decline in the 2017 cohort. As additional case discussions in the preclinical material are introduced, we need to be more deliberate practicing good interviewing habits for every case, which would include asking expanded social history questions.13
To our surprise, students in the 2018 cohort included occupational concerns at a much higher level for each OSCE. This may be in part that there were new facilitators for small groups in 2018 who emphasized the social history during small groups. Additionally, the 2017 cohort may have influenced the 2018 students with informal advising.
Although this is a single institution study, our subject matter experts (medical student and faculty veterans) helped write a thorough case that exposed students to not only a thorough medical history but also occupational exposures. Although not equivalent to military service, we used occupational exposure as a proxy in the expanded social history, which was the higher-order goal for this session. Additional military cases could be developed by other institutions, particularly if a veterans’ hospital is not readily accessible.
In the future, an OSCE is being developed that more deliberately includes military health issues could provide a more accurate evaluation of the ability of students to connect military history with diagnoses. We can also collect student impressions of these cases.
This study demonstrates the importance of teaching medical learners to include military service when taking a social history. This military case-based discussion provides an effective mechanism for medical students to broaden their understanding of the social history and make connections between occupation and health.
References
- Chretien J-P, Chretien KC. Coming home from war. J Gen Intern Med. 2013;28(7):953-956. doi:10.1007/s11606-013-2359-7
- Ross PT, Lypson ML. Veteran-centred content in medical education. Clin Teach. 2019;16(1):53-57. doi:10.1111/tct.12775
- Meyer EG, Writer BW, Brim W. The importance of military cultural competence. Curr Psychiatry Rep. 2016;18(3):26. doi:10.1007/s11920-016-0662-9
- Muirhead L, Hall P, Jones-Taylor C, Clifford GD, Felton-Williams T, Williams K. Critical questions: advancing the health of female Veterans. J Am Assoc Nurse Pract. 2017;29(10):571-580. doi:10.1002/2327-6924.12490
- Gleeson TD, Hemmer PA. Providing care to military personnel and their families: how we can all contribute. Acad Med. 2014;89(9):1201-1203. doi:10.1097/ACM.0000000000000368
- Rudert JB, Chapman HJ. Evaluating service-connected occupational exposure. Clin Teach. 2019;16(1):85-86. doi:10.1111/tct.12981
- Behforouz HL, Drain PK, Rhatigan JJ. Rethinking the social history. N Engl J Med. 2014;371(14):1277-1279. doi:10.1056/NEJMp1404846
- Adler NE, Stead WW. Patients in context—EHR capture of social and behavioral determinants of health. N Engl J Med. 2015;372(8):698-701. doi:10.1056/NEJMp1413945
- Lypson ML, Ravindranath D, Ross PT, et al. Veteran interactive cases to reinforce service (VICTORS): standardized patient assessment of veteran-centered care. MedEdPORTAL. 2016;12(1):10326. doi:10.15766/mep_2374-8265.10326
- Fabrizio J, DeNardi K, Boland M, Suffoletto JA. Use of a standardized patient in teaching medical students to asses for PTSD in military veteran patients. MedEdPORTAL. 2017;13(1):10608. doi:10.15766/mep_2374-8265.10608
- Terrigino CA, Like RC, Steptoe RJ, et al. Patient-centered care for warriors, veterans, and their families: an interprofessional modular curriculum. MedEdPORTAL. 2016;12(1):10389. doi:10.15766/mep_2374-8265.10389
- Smidt A, Balandin S, Sigafoos J, Reed VA. The Kirkpatrick model: A useful tool for evaluating training outcomes. J Intellect Dev Disabil. 2009;34(3):266-274. doi:10.1080/13668250903093125
- Ericsson KA, Krampe RT, Tesch‐Romer C. The role of deliberate practice in the acquisition of expert performance. Psychol Rev. 1993;100(3):363-406. doi:10.1037/0033-295X.100.3.363



There are no comments for this article.