Background and Objectives: Although burnout in medicine—particularly medical education—represents an ongoing problem, relatively few studies have established longitudinal connections between burnout and risk factors. Establishment of specific causal links and risk factors will determine important curriculum changes to reduce the risk of burnout in medical learners. Our study aimed to explore links between emotion regulation skill (strategies individuals use to regulate emotional experiences and responses to stress) and vulnerability to burnout using a longitudinal design in one family medicine residency program.
Methods: Family medicine residents completed the Difficulties with Emotion Regulation Scale (DERS) and the Copenhagen Burnout Inventory (CBI) at the beginning of each year (July/August). The residency program collected data over the course of 5 years. All residents consented to participate. We used linear regression analyses to examine postgraduate year-1 DERS scores as a predictor of postgraduate year-2 burnout and postgraduate year-3 burnout.
Results: In this sample of residents, higher scores on the DERS at the first year of residency predicted personal and work-related burnout on the Copenhagen Burnout Inventory (CBI) at the beginning of the second and third years.
Conclusions: Difficulties with emotion regulation predicted personal burnout in this small sample. This finding dovetails with cross-sectional data in the literature. Although further mechanisms contributing to burnout should be explored, this finding suggests that direct instruction in adaptive emotion regulation strategies delivered early in medical education could provide significant downstream benefits for family medicine residents.
Medical training presents a culture that leaves many learners vulnerable to burnout.1 Although medical education and health care systems play a role, individual difference factors may explain variability in vulnerability to burnout. Resident physicians remain at elevated risk for burnout, substance use, and depression.2,3 Efficacy of existing resiliency curriculum is unclear, and it is difficult to assess how curriculum adjustments impact resident well-being.4,5 The literature describes correlates of burnout, but few studies have employed longitudinal designs that could clarify underlying mechanisms.6
Emotion regulation skills could be one such mechanism underpinning burnout. Emotion regulation skills are the cognitive and behavioral strategies individuals use to regulate their emotional experience and response to stressors.1,7,8 Emotion regulation skills include awareness of one’s emotions, willingness to accept one’s emotional experience, access to coping strategies, and proficiencies to delay impulsive responding.7
Residents with fewer or less flexible emotion regulation skills likely experience increased vulnerability to personal burnout, professional burnout, and burnout with patients.7 We designed this longitudinal study to understand whether difficulties with emotion regulation predicted burnout over the course of residency.
Data collection occurred annually from July 2015 to July 2019. Residents completed informed consent annually. Participants did not receive compensation. Participants completed questionnaires in July or August of each year of residency. Participants completed forms during dedicated sessions in the didactic curriculum and returned the forms confidentially. Demographics and psychological questionnaires were separate. Participant numbers were the only identifiers on psychological questionnaires. To maximize anonymity of data, demographics questionnaires did not include participant numbers and were stored separately. Questionnaire data were stored off-site. Research assistants without knowledge of the residency program entered data.
The Copenhagen Burnout Inventory (CBI) contains 19 Likert-type items measuring three dimensions of burnout: personal burnout (eg, How often are you emotionally exhausted?), work-related burnout (eg, Are you exhausted in the morning at the thought of another day at work?), and patient-related burnout (eg, Are you tired of working with patients?). The CBI, a public domain measure, is based on a definition of burnout as exhaustion attributed to work. It has been shown to have high internal reliability and construct validity.9 The Difficulties in Emotion Regulation Scale (DERS) contains 36 Likert-type items assessing emotion regulation (eg, lack of emotional awareness, nonacceptance of emotional responses, impulse control difficulties, limited access to emotion regulation strategies).10
We analyzed data using IBM SPSS Statistics for Windows, Version 26.0 (IBM Corp, Armonk, NY). We used linear regression analyses to examine postgraduate year-1 (PGY-1) DERS score as a predictor of each of the three types of burnout, both concurrently (eg, PGY-1 DERS as a predictor of PGY-1 personal burnout) and longitudinally (eg, PGY-1 DERS as a predictor of PGY-2 personal burnout). Three cohorts of residents completed data for all 3 years of their residencies. The Ethics Committee at Northeast Iowa Medical Education Foundation approved this study in July, 2015.
Over 5 years of the study, 29 individuals had complete data for PGY1, 19 had data for both PGY1 and PGY2, and 12 had data for both PGY1 and PGY3. Demographic data represent all 48 residents who participated during the study. Mean age was 30.88 years (SD=3.47 years) and 56.47% identified as female. No participants identified as transgender. More than half of the sample (55.56%) were US citizens. Participants could mark multiple race and ethnicity categories; 58.82% marked White, 25.88% Asian/Asian-American/Pacific Islander, 9.41% Black/African-American, 5.88% Hispanic, and 9.41% categorized themselves as “other” and specified additional categories (eg, mixed race, Pakistani, Arabic, Indian).
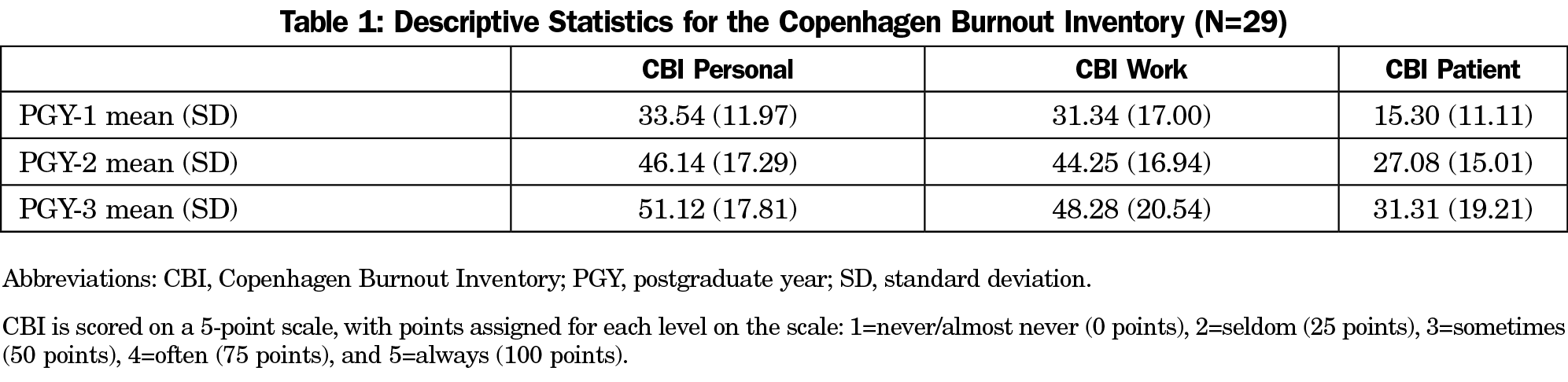
Table 1 includes descriptive statistics for the CBI for the sample (N=29). For PGY-1 DERS (used as a predictor in regression analyses), the mean was 71.76 (SD=15.50), which is comparable to results from an undergraduate sample (M=78.65, SD=20.25).10
PGY-1 DERS was significantly associated with PGY-1 personal, work, and patient burnout (P values <.05). PGY-1 DERS significantly predicted personal and work-related burnout at PGY2 and PGY3. PGY-1 DERS scores explained over 56% of the variance in PGY-3 personal burnout (P<.01). Table 2 shows regression results.
Difficulties with emotion regulation measured during the first year of residency correlated positively with personal, work-related, and patient-related burnout. Difficulties with emotion regulation during the first year of residency predicted personal and work-related burnout in subsequent years and appeared to be a stronger predictor of subsequent burnout than concurrent burnout, especially for personal burnout. Few studies examine burnout longitudinally, and fewer still have identified potential predictors or mechanisms of burnout prospectively. Emotion regulation skills can be augmented or enhanced under the right conditions and with a robust curriculum. Skill-based enhancement of emotion regulation can be integrated into curriculum for residency education.11,12 These findings are consistent with research indicating that emotion regulation plays a significant role in resiliency.7
Difficulties with emotion regulation did not predict patient-related burnout. This could indicate that emotion regulation does not influence the development of burnout in all domains. Many residents develop durable communication skills with carefully-rehearsed strategies for handling challenging patient encounters; these skills could protect against patient-related burnout. Alternatively, the absence of a correlation between PGY-1 difficulties in emotion regulation and subsequent patient-related burnout could be because residents do not want to admit when they are frustrated in their work with patients.
The results of this study could be unique to this sample. Larger scale longitudinal studies across programs could advance knowledge of the relationship between emotion regulation and burnout. However, these results suggest that building emotion regulation skills should be a focus of medical education.4,13 For example, including emotion regulation skill building such as mindfulness-based cognitive training within the curriculum and dedicating curricular time for reflection could yield reduced vulnerability to burnout over the course of residency for those willing to participate.11,12 This study suggests that measurement of emotion regulation and intervention to bolster emotion regulation skill could bear fruit for both residency programs and residents.
References
- Weilenmann S, Schnyder U, Parkinson B, Corda C, von Känel R, Pfaltz MC. Emotion transfer, emotion regulation, and empathy-related processes in physician-patient interactions and their association with physician well-being: A theoretical model. Front Psychiatry. 2018;9(AUG):389. doi:10.3389/fpsyt.2018.00389
- McManus IC, Winder BC, Gordon D. The causal links between stress and burnout in a longitudinal study of UK doctors. Lancet. 2002;359(9323):2089-2090. doi:10.1016/S0140-6736(02)08915-8
- Eckleberry-Hunt J, Kirkpatrick H, Taku K, Hunt R, Vasappa R. Relation between physicians’ work lives and happiness. South Med J. 2016;109(4):207-212. doi:10.14423/SMJ.0000000000000437
- Hategan A, Riddell T. Bridging the gap: responding to resident burnout and restoring well-being. Perspect Med Educ. 2020;9(2):117-122. doi:10.1007/s40037-020-00567-3
- Lin DT, Liebert CA, Tran J, Lau JN, Salles A. Emotional Intelligence as a Predictor of Resident Well-Being. In: Journal of the American College of Surgeons. Vol 223. Elsevier Inc; 2016:352-358, doi:10.1016/j.jamcollsurg.2016.04.044
- Ricker M, Maizes V, Brooks AJ, Lindberg C, Cook P, Lebensohn P. A longitudinal study of burnout and well-being in family medicine resident physicians. Fam Med. 2020;52(10):716-723. doi:10.22454/FamMed.2020.179585
- Jackson-Koku G, Grime P. Emotion regulation and burnout in doctors: a systematic review. Occup Med (Lond). 2019;69(1):9-21. doi:10.1093/occmed/kqz004
- Aggarwal R, Deutsch JK, Medina J, Kothari N. Resident wellness: An intervention to decrease burnout and increase resiliency and happiness. MedEdPORTAL. 2017;13(1):10651. doi:10.15766/mep_2374-8265.10651
- Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work Stress. 2005;19(3):192-207. doi:10.1080/02678370500297720
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 26(1), 41–54. doi: 10.1023/B:JOBA.0000007455.08539.94
- Lebares CC, Guvva EV, Olaru M, et al. Efficacy of mindfulness-based cognitive training in surgery: additional analysis of the Mindful Surgeon Pilot Randomized Clinical Trial. JAMA Netw Open. 2019;2(5):e194108. doi:10.1001/jamanetworkopen.2019.4108
- Minichiello V, Hayer S, Gillespie B, Goss M, Barrett B. Developing a mindfulness skills-based training program for resident physicians. Fam Med. 2020;52(1):48-52. doi:10.22454/FamMed.2020.461348
- Bursch B, Mulligan C, Keener AM, et al. Education Research: evaluation of curriculum to teach resilience skills to neurology residents. Neurology. 2019;92(11):538-541. doi:10.1212/WNL.0000000000007100
- Philibert I, Konopasek L. The WIT and the WES: tools for categorizing and evaluating physician well-being programs. J Grad Med Educ. 2020;12(1):14-18. doi:10.4300/JGME-D-19-00450.1



There are no comments for this article.