The opioid epidemic resulted in alarming rates of death over the last two decades.1–3 More than half of primary care physicians report discomfort managing chronic pain and rate their residency training in chronic pain management as insufficient.4–6 In recent years, many residency programs developed and implemented chronic pain curricula, dedicated pain clinics, and/or standardized patient encounters.7–10 These measures resulted in decreased physician stress, improved attitudes toward patients with chronic pain, and improved knowledge of pain assessment and treatment.7–10 The creation of multidisciplinary or interprofessional teams tasked with implementing clinic or system-based opioid prescribing protocols with regular review of opioid prescribing practices is associated with a reduction in morphine equivalent dosing (MED) and/or improved adherence to clinical guidelines.11–16 We hypothesized that a resident-focused opioid prescribing curriculum, coupled with an interprofessional committee to protocolize and review opioid prescribing practices in training, could address the educational gap and prescriber discomfort in chronic pain management. We also hypothesized that this curriculum and committee would standardize opioid prescribing practice to align with evidence-based, best practice guidelines for chronic pain management.17 Here, we describe the development, implementation, and outcomes of a novel, long-standing interprofessional safe prescribing committee (SPC) and resulting policy, protocol, and longitudinal curriculum to address patient care and educational gaps in chronic pain management for residents in training.
BRIEF REPORTS
An Interprofessional Approach to Chronic Pain Management and Education
Nida S. Awadallah, MD | Vanessa Rollins, PhD | Alvin B. Oung, PharmD | Miriam Dickinson, PhD | Dionisia de la Cerda, MPA | Susan Calcaterra, MD, MPH | Jeremy Orr, MD, MPH | Marc Grushan, MD
Fam Med. 2022;54(1):47-53.
DOI: 10.22454/FamMed.2022.753618
Background and Objectives: The opioid epidemic highlights the importance of evidence-based practices in the management of chronic pain and the need for improved resident education focused on chronic pain treatment and controlled substance use. We present the development, implementation, and outcomes of a novel, long-standing interprofessional safe prescribing committee (SPC) and resulting policy, protocol, and longitudinal curriculum to address patient care and educational gaps in chronic pain management for residents in training.
Methods: The SPC developed and implemented an opioid prescribing policy, protocol, and longitudinal curriculum in a single, community-based residency program. We conducted a postcurriculum survey for resident graduates to assess impact of knowledge gained. We conducted a retrospective chart review for patients on chronic opioid therapy to assess change in morphine equivalent dosing (MED) and pain scores pre- and postintervention.
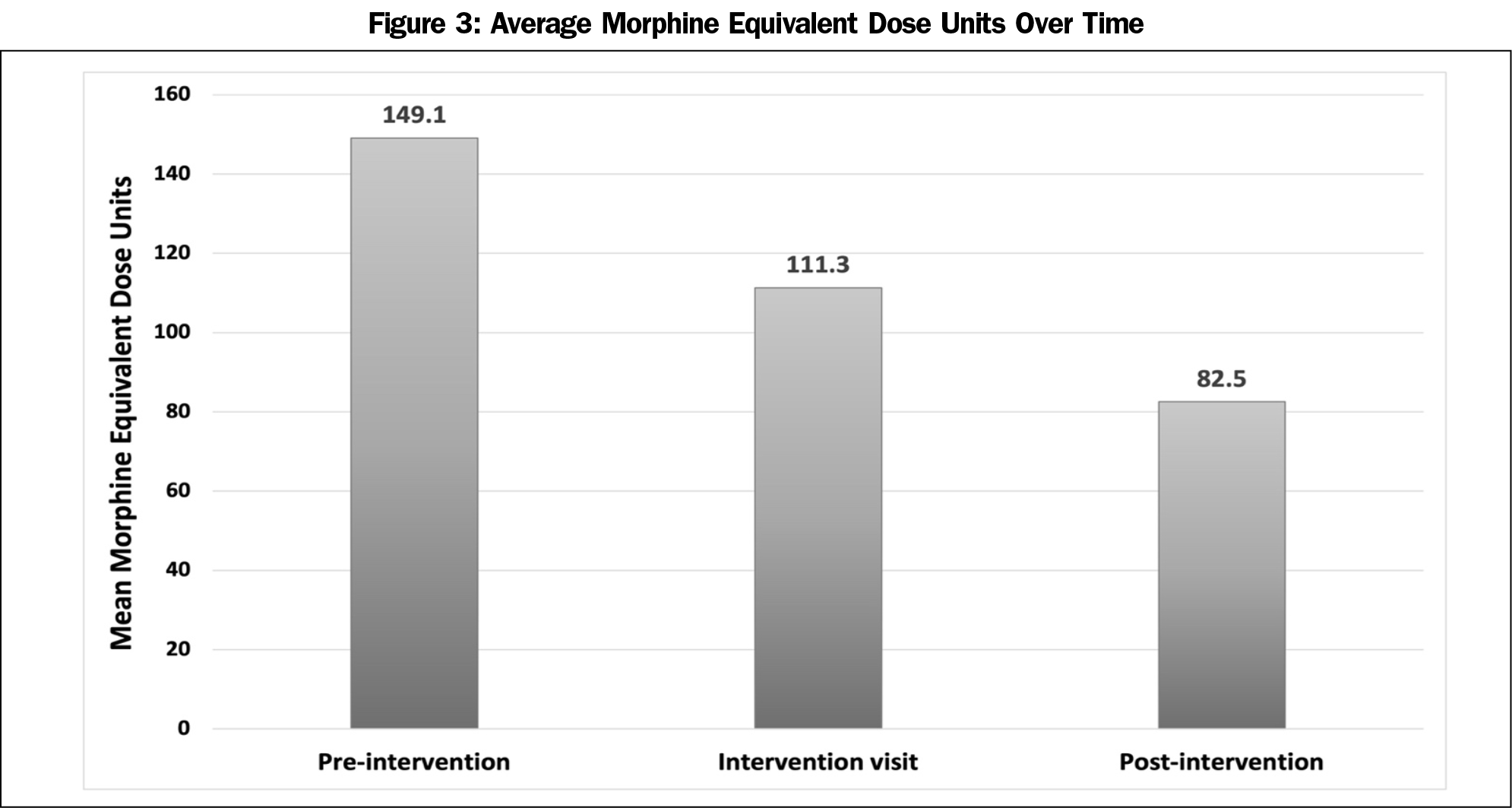
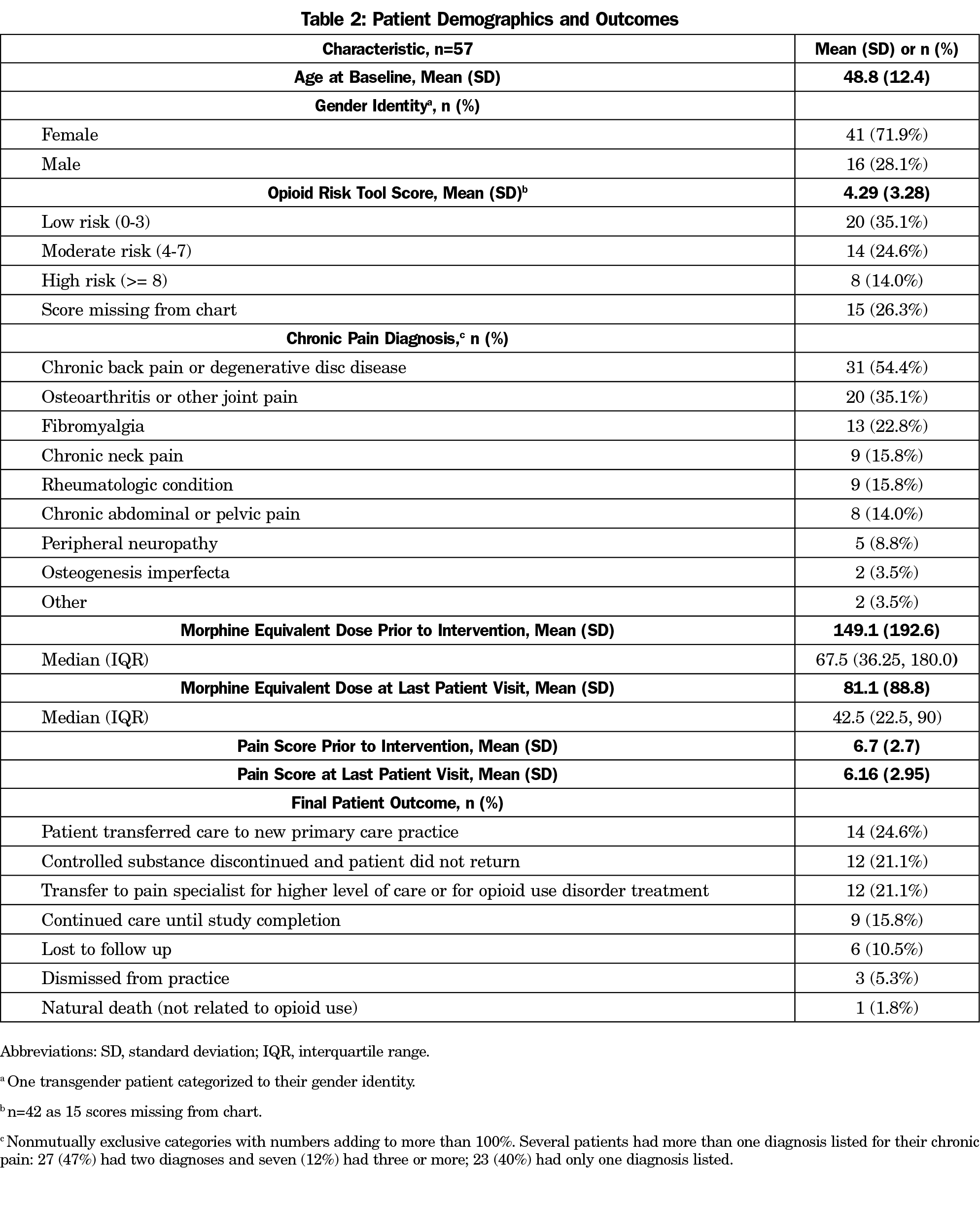
Results: A postcurriculum survey was completed by 20/26 (77%) graduates; 18/20 (90%) felt well-equipped to manage chronic pain based on their residency training experience. We completed a retrospective chart review on 57 patients. We found a significant decrease in MED (-20.34 [SE 5.12], P<.0001) at intervention visit with MED reductions maintained through the postintervention period (-9.43 per year additional decrease [SE 5.25], P=.073). We observed improvement in postintervention pain scores (P=.017).
Conclusions: Our study illustrates the effectiveness of an interprofessional committee in lowering prescribed opioid doses and enhancing chronic pain education in a community-based residency setting.
The HCA-HealthOne Institutional Review Board in Denver, Colorado, deemed this study exempt.
Safe Prescribing Committee
Development and Composition. In 2011, we developed an SPC at our community-based, university-affiliated family medicine residency clinic serving an urban underserved population. Initial committee responsibilities included (1) development and implementation of a policy to ensure that evidence-based care was provided to patients on chronic opioid therapy (COT), and (2) providing resident education on evidence-based practices for chronic pain management and opioid prescribing.18 Committee members included a family medicine faculty physician, clinical pharmacist, clinical psychologist, sitting resident member appointed for a 12-month term, a monthly rotating resident member, a member of the residency program’s quality improvement committee, and a clinical social worker and/or patient care coordinator.
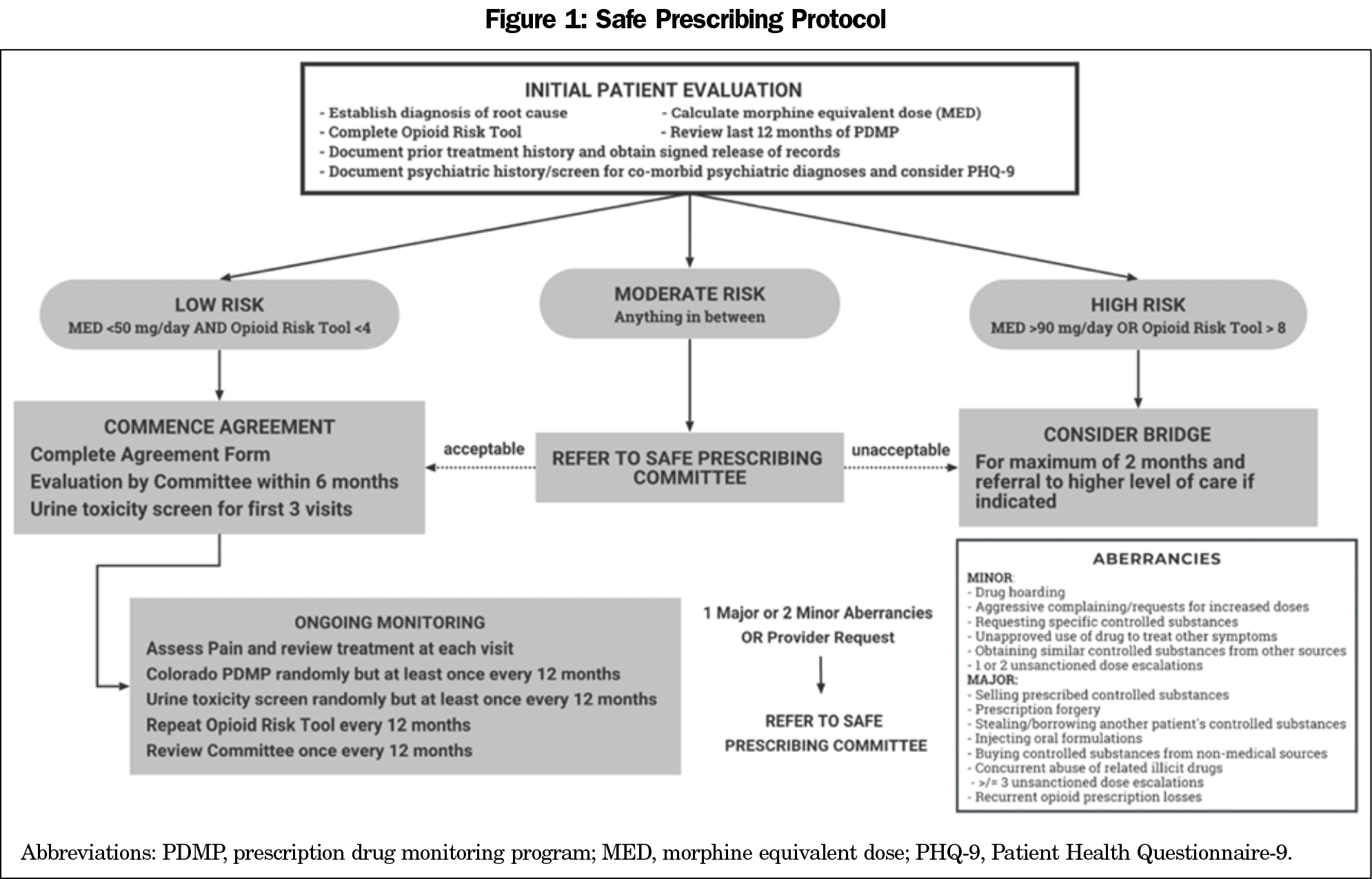
Clinic Policy and Toolbox. Informed by evidence-based guidelines and expert consensus addressing chronic pain management and opioid prescribing, the SPC developed a Safe Prescribing Policy and a prescriber’s toolbox containing easily accessible documents.17,19–23 The toolbox included several documents from the policy, including (1) the Safe Prescribing Protocol for initial patient evaluation and risk stratification developed by the SPC (Figure 1), (2) a copy of our pain management agreement to be reviewed by the patient and treating physician, (3) instructions for ongoing monitoring of patients on COT and, (4) prescribing information including opioid conversion and equianalgesic dosing tools.17,19–23 These documents were printed and placed in a binder labeled “Pain Management Toolbox” in our preceptor room with electronic copies stored on a shared drive.
Committee Workshops. The SPC implemented monthly workshops where quality-based reviews of individual patient cases were discussed. All patients on COT were placed on a secure, clinic-based registry and were intermittently reviewed to ensure consistency with SPC guidelines. Physicians also referred patient cases to SPC workshops for consultation. A minimum of four members of the interprofessional team were required for the committee workshops to occur. Quarterly, the workshops were held as part of the usual didactic curriculum with all available faculty and residents in attendance. Residents had the opportunity to participate in SPC workshops, with resident committee members attending monthly. Resident and faculty physicians were assigned cases to review several days before scheduled workshops and were expected to present the cases for discussion. Risk stratification by Opioid Risk Tool and morphine equivalent dosing (MED), aberrancies, care concerns, and proposed plan moving forward were included in summaries and documented for care teams.17,19–25 All patient care recommendations including assessment or treatment for mental health conditions, use of adjuvants and/or nonopioid treatment options for chronic pain management, treatment recommendations for not-optimally-controlled comorbid health conditions like diabetes, opioid overdose prevention, and tapering indications and recommendations for those who were high risk were noted on the secure registry and sent to the treating and/or primary care physician via the electronic medical record.
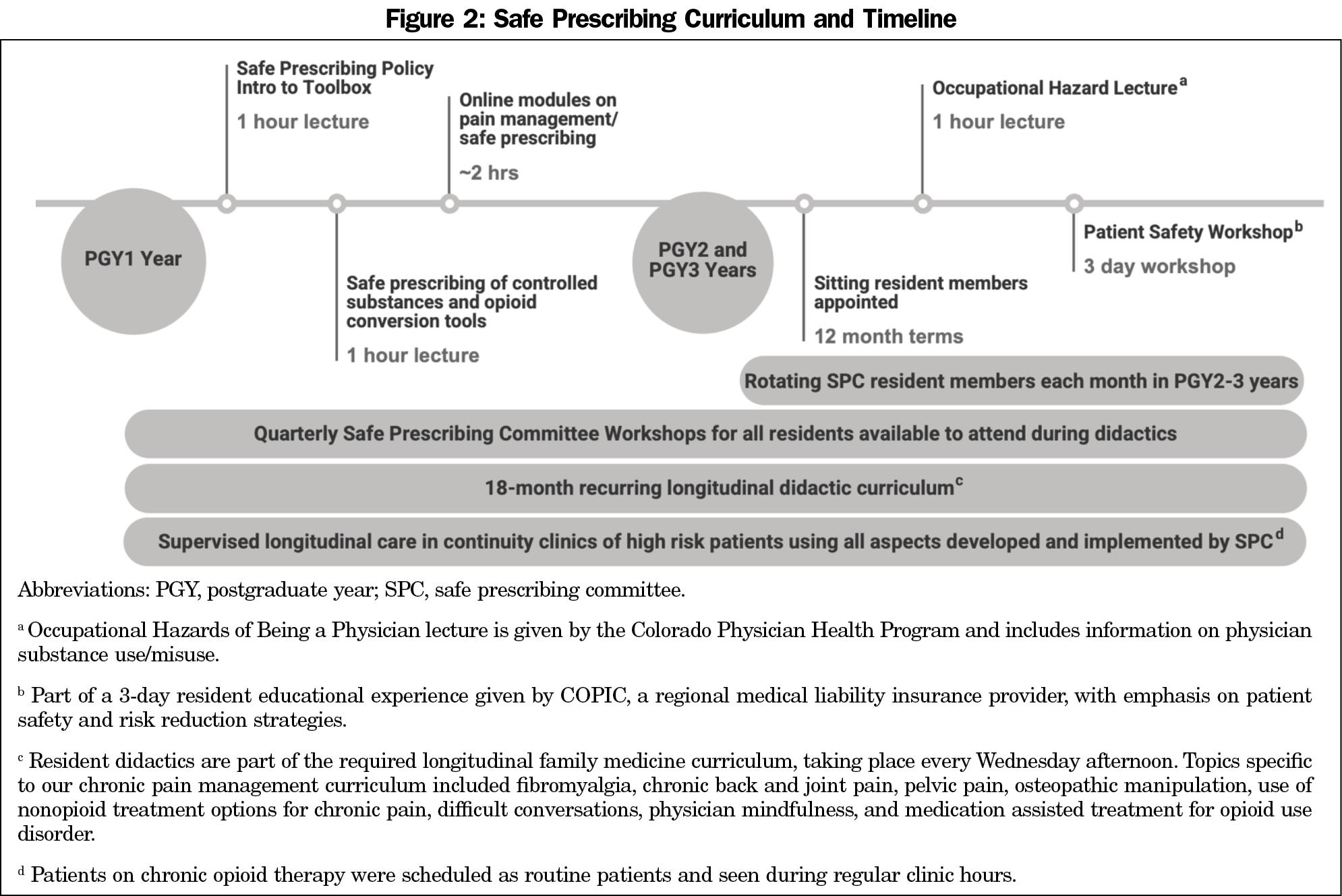
Curriculum Development. The SPC developed a longitudinal curriculum to educate resident trainees on best practices for chronic pain management (Figure 2).17,19–29 The longitudinal curriculum consisted of a combination of lectures, online modules, SPC workshops, and longitudinal patient care in our residency-based clinic with 1:1 precepting. In addition to faculty preceptors, faculty members of the SPC, including a clinical pharmacist and psychologist, were available to answer questions on chronic pain management during clinic in real-time utilizing evidence-based guidelines, expert consensus materials, and the Safe Prescribing Policy, Protocol, and other toolbox materials as resources. Part of our longitudinal curriculum involved incorporating topics of chronic pain management, substance use/misuse, risk management, and patient safety into our regular 18-month recurring longitudinal didactics curriculum. To address the impact of race and/or socioeconomic disparities, we also incorporated experiential activities into our curriculum such as community site visits as well as small-group and reflection activities centered around documentaries on the opioid epidemic and high-risk groups.
Learner Outcomes: Curriculum Assessment
To assess the learner impact of our interventions, we sent an anonymous, voluntary survey to all eligible resident graduates. To qualify for survey participation, graduates must have completed at least the first 2 years of the SPC curriculum and graduated residency between 2015 and 2019. Survey items were developed using an iterative review process by a group of faculty medical educators. To ensure confidentiality, the only demographic information collected was year of residency graduation. The electronic survey link was sent in September 2020, with a reminder sent 1 week later.30
Patient Outcomes: Change in Morphine Equivalent Doses and Pain Scores
Patients on COT were identified by the registry utilized at SPC workshops. A retrospective chart review to assess changes in MED pre/post-SPC implementation was conducted between June 2018 and September 2018. Those with a cancer diagnosis or with no care documented prior to SPC implementation were excluded. Morphine equivalent doses were calculated using Centers for Disease Control and Prevention conversion factors.23 Pain scores recorded during patient care visits using a numerical rating scale from 0 (no pain) to 10 (worst pain) were also reviewed and analyzed.31 Each visit was designated as preintervention (visits prior to initial SPC review), intervention (visit immediately following initial SPC review), or postintervention (all visits after intervention visit). To account for those who were discontinued or dismissed without getting a refill prescription for opioids, second to last visit pain scores and MED were used, with last-visit MED (generally 0) set to missing for these patients. General linear mixed effects models were used to analyze the repeated measures within patients over time, adjusting for age and gender.
Learner Outcomes
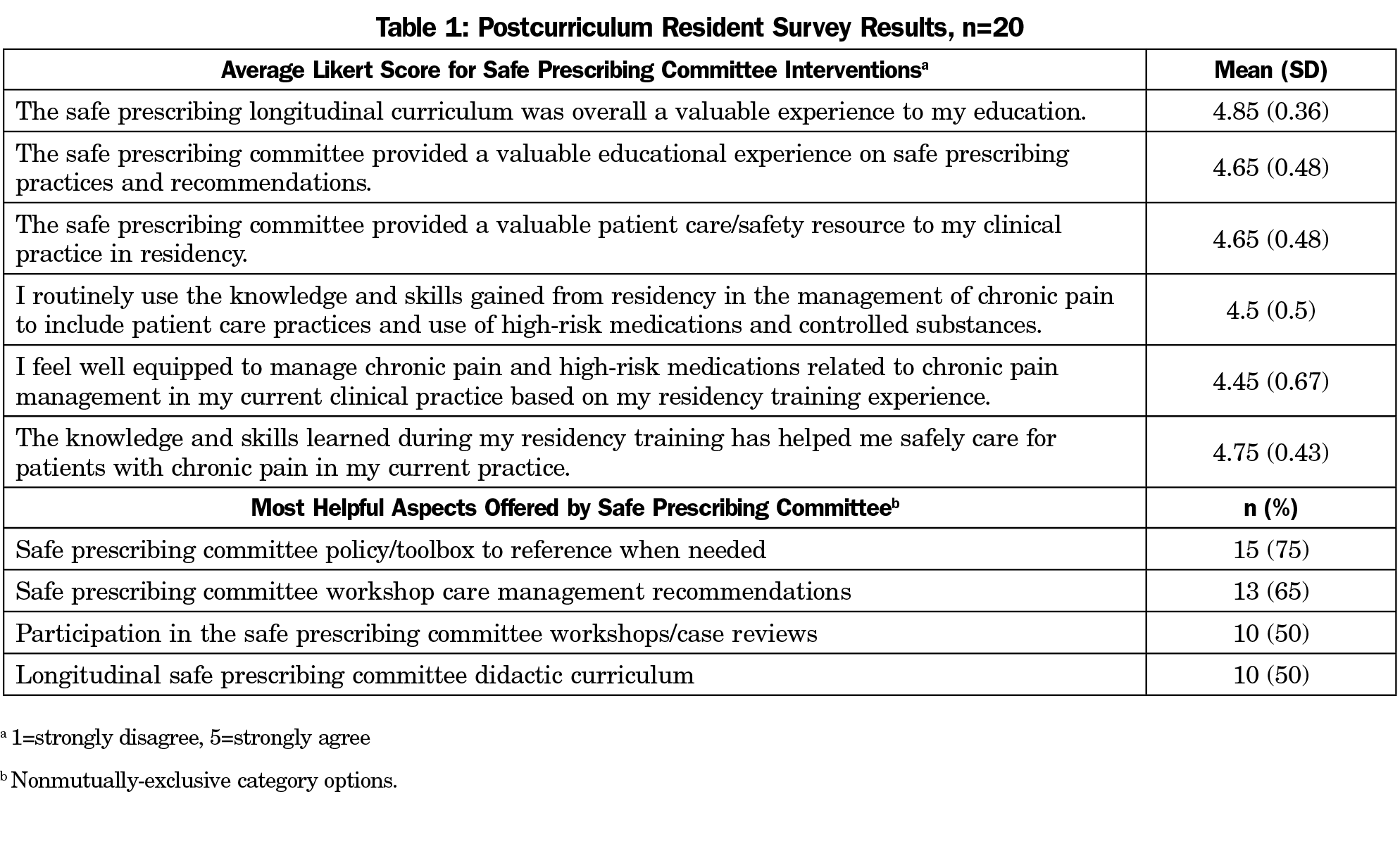
A total of 30 previous resident learners participated in aspects of our curriculum; 26 graduates qualified for survey participation and 20/26 (77%) completed the survey. Of these, five (25%) graduated in 2015, three (15%) in 2016, three (15%) in 2017, six (30%) in 2018, and three (15%) in 2019. All survey respondents agreed or strongly agreed that the longitudinal safe prescribing curriculum was a valuable experience to their education and routinely use the knowledge and skills gained from residency in their current clinical practice, with 18/20 (90%) noting that they feel well-equipped to manage chronic pain and high-risk medications related to chronic pain management in their clinical practice based on their residency training experience. Postcurriculum resident survey results are listed in Table 1.
Patient Outcomes
Between October 2011 and February 2018, 230 patients on COT were added to the registry; 57 patients had care documented before and after SPC initiation. Patient demographics and outcomes are listed in Table 2. Patients had an average of 23.4 (SD=19.5) visits (median=17 [IQR 7, 37.5]). All 57 patients had MED and pain scores documented and included in analysis. We found a small, nonsignificant change in MED during the preintervention period (-1.24 per year [se 7.38], P=.867). At the time of committee review, we found a significant decrease in MED (-20.34 [SE 5.12], P<.0001) with postintervention MED reductions maintained through the postintervention period (-9.43 per year additional decrease [SE 5.25], P=.073). Simple pre/post comparison of MED indicated that significant overall decrease (P=.001; Figure 3). Even with decrease in MED, adjusted postintervention pain scores (all postintervention pain scores, adjusted for clustering of observations within individuals) were significantly improved compared to preintervention pain scores (all preintervention pain scores, adjusted for clustering of observations within individuals; adjusted pre: 6.90 [SE 0.31], adjusted post: 6.56 [SE] 0.31; P=.017).
Our study complements the existing literature demonstrating the effectiveness of an interprofessional committee in the management of high-risk patients on opioids.11–13,15,16 Our study extends the literature by demonstrating the effectiveness of an SPC on resident education.
The SPC faced some challenges. Regular monthly workshops were sometimes difficult to schedule, particularly with all members of the committee present. To circumvent this, only four members were required to be in attendance, and workshops were scheduled in a recurring fashion. In addition, quarterly workshops during didactics made the scheduling process easier and more efficient. Buy-in from a small number of faculty concerned about preserving their autonomy was also difficult initially. Therefore, we emphasized the consultation component and referenced available evidence-based resources in our recommendations. Both physician and patient satisfaction are areas worth exploring in future studies.
Our study has several limitations. Although our anonymous resident graduate survey response rate was 77%, the response rate may be biased in that resident graduates with strong feelings on the subject matter may have been more likely to respond. Also, the SPC was implemented at a single, community-based program serving an urban underserved patient population. This setting may not be generalizable to other patient populations. In addition, only 15.8% of patients included in this study continued care until study completion. About 21% did not return following opioid discontinuation, and 5% were dismissed from our practice. All attempts to gradually decrease doses were made, except for significant aberrancies such as prescription forgery. Those with suspected substance use disorders were referred for specialized care. Attrition rate for patients on COT receiving care in a residency clinic setting should be further investigated to ensure interventions such as these do not have unintended consequences. Lastly, the SPC and its interventions were initiated before medication assisted treatment (MAT) implementation became highly encouraged for family physicians, including residents in training.32 Future studies should include MAT as part of the longitudinal training experience.
The implementation of our SPC and resulting policy, protocol, and longitudinal curriculum illustrates the effectiveness of an interprofessional committee in lowering prescribed opioid doses and enhancing chronic pain education in a community-based residency setting, and can be a roadmap with proven efficacy and measurable outcomes. Future studies can focus on confirming these findings in a variety of settings to fit the needs of different practices and patient populations.
Acknowledgments
Financial Support: This publication was supported by NIH/NCATS Colorado CTSA Grant Number UL1 TR002535. Its contents are the authors’ sole responsibility and do not necessarily represent official NIH views.
Presentations: A poster presentation containing data from this manuscript was presented virtually at the 2021 Society of Teachers of Family Medicine Annual Spring Conference and limited preliminary data and outline of committee policies were presented at the Collaborative Family Healthcare Association 15th Annual Conference in Broomfield, Colorado in 2013.
References
- HHS Acting Secretary Declares Public Health Emergency to Address National Opioid Crisis. US Department of Health and Human Services. Published October 26, 2017. Accessed September 25, 2020. https://www.hhs.gov/about/news/2017/10/26/hhs-acting-secretary-declares-public-health-emergency-address-national-opioid-crisis.html
- Understanding the Epidemic. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. Published March 19, 2020. Accessed March 13, 2021. https://www.cdc.gov/drugoverdose/epidemic/index.html
- Wilson N, Kariisa M, Seth P, Smith H IV, Davis NL. Drug and opioid-involved overdose deaths - United States, 2017-2018. MMWR Morb Mortal Wkly Rep. 2020;69(11):290-297. doi:10.15585/mmwr.mm6911a4
- Upshur CC, Luckmann RS, Savageau JA. Primary care provider concerns about management of chronic pain in community clinic populations. J Gen Intern Med. 2006;21(6):652-655. doi:10.1111/j.1525-1497.2006.00412.x
- Jamison RN, Sheehan KA, Scanlan E, Matthews M, Ross EL. Beliefs and attitudes about opioid prescribing and chronic pain management: survey of primary care providers. J Opioid Manag. 2014;10(6):375-382. doi:10.5055/jom.2014.0234
- O’Rorke JE, Chen I, Genao I, Panda M, Cykert S. Physicians’ comfort in caring for patients with chronic nonmalignant pain. Am J Med Sci. 2007;333(2):93-100. doi:10.1097/00000441-200702000-00005
- Rickert J, Devlin K, Krohn K. Comprehensive care of pain: developing systems and tools to improve patient care and resident education. Int J Psychiatry Med. 2016;51(4):337-346. doi:10.1177/0091217416659270
- Evans L, Whitham JA, Trotter DRM, Filtz KR. An evaluation of family medicine residents’ attitudes before and after a PCMH innovation for patients with chronic pain. Fam Med. 2011;43(10):702-711.
- Smith CD. A curriculum to address family medicine residents’ skills in treating patients with chronic pain. Int J Psychiatry Med. 2014;47(4):327-336. doi:10.2190/PM.47.4.g
- Chen I, Goodman B III, Galicia-Castillo M, Quidgley-Nevares A, Krebs M, Gliva-McConvey G. The EVMS pain education initiative: a multifaceted approach to resident education. J Pain. 2007;8(2):152-160. doi:10.1016/j.jpain.2006.06.008
- Gernant SA, Bastien R, Lai A. Development and evaluation of a multidisciplinary controlled substances committee within a patient-centered medical home. J Am Pharm Assoc (Wash DC). 2015;55(6):656-663. doi:10.1331/JAPhA.2015.14257
- Bourgeois HC, Proteau RC, Vielma CV, Hartung DM, Irwin AN. Evaluation of an interdisciplinary controlled substance review committee on opioid prescribing in a community health center. Pain Med. 2020;21(9):1840-1846. doi:10.1093/pm/pnaa075
- Weimer MB, Hartung DM, Ahmed S, Nicolaidis C. A chronic opioid therapy dose reduction policy in primary care. Subst Abus. 2016;37(1):141-147. doi:10.1080/08897077.2015.1129526
- Jacobs SC, Son EK, Tat C, Chiao P, Dulay M, Ludwig A. Implementing an opioid risk assessment telephone clinic: outcomes from a pharmacist-led initiative in a large Veterans Health Administration primary care clinic, December 15, 2014-March 31, 2015. Subst Abus. 2016;37(1):15-19. doi:10.1080/08897077.2015.1129527
- Zeigler C, Mackey K, Hulen E, Carr T, Saha S, Edwards ST. Frontline account: reducing the stress of pain management through the implementation of a controlled substance review group in a VA internal medicine residency clinic. J Gen Intern Med. 2017;32(7):832-835. doi:10.1007/s11606-016-3930-9
- Rivich J, McCauliff J, Schroeder A. Impact of multidisciplinary chart reviews on opioid dose reduction and monitoring practices. Addict Behav. 2018;86:40-43. doi:10.1016/j.addbeh.2018.04.018
- Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315(15):1624-1645. doi:10.1001/jama.2016.1464
- Chou R, Fanciullo GJ, Fine PG, et al; American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113-130. doi:10.1016/j.jpain.2008.10.008
- Webster LR, Webster RM. Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the Opioid Risk Tool. Pain Med. 2005;6(6):432-442. doi:10.1111/j.1526-4637.2005.00072.x
- Passik SD. Issues in long-term opioid therapy: unmet needs, risks, and solutions. Mayo Clin Proc. 2009;84(7):593-601. doi:10.1016/S0025-6196(11)60748-9
- Dunn KM, Saunders KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85-92. doi:10.7326/0003-4819-152-2-201001190-00006
- Young SS, Ballantyne JC, Domino FJ, Wetterau NW. Balancing Clinical and Risk Management Considerations for Chronic Pain Patients on Opioid Therapy. Leawood, KS: American Academy of Family Physicians; 2008.
- CDC Guideline for Prescribing Opioids for Chronic Pain. Centers for Disease Control and Prevention. Published Updated August 28, 2019. Accessed January 2, 2021. https://www.cdc.gov/drugoverdose/prescribing/guideline.html
- Prescription Drug Monitoring Program: Helping reduce misuse, abuse & diversion of prescription drugs. Colorado Department of Regulatory Agencies, Division of Professions and Occupations. Published 2020. Accessed December 31, 2020. https://dpo.colorado.gov/PDMP
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. doi:10.1046/j.1525-1497.2001.016009606.x
- American Medical Association. Opioid and Pain Management CME: Guidelines, Research and Treatments. American Medical Association Ed Hub. Accessed February 12, 2021. https://edhub.ama-assn.org/pages/opioid-cme-course
- Scope of Pain: Safer/Competent Opioid Prescribing Education. Boston University School of Medicine. Accessed February 12, 2021. https://www.scopeofpain.org/core-curriculum/online-training/
- American Academy of Family Physicians. Reprint No. 286 Recommended Curriculum Guidelines for Family Medicine Residents - Chronic Pain Management. American Academy of Family Physicians. Published August 2008. Revised June 2015. Accessed December 27, 2020. http://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint286_Pain.pdf
- Patient Safety and Risk Management: Resident Rotation. Copic Insurance Company. Published 2021. Accessed June 26, 2021. https://www.callcopic.com/patient-safety-risk-management/resident-rotation
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi:10.1016/j.jbi.2008.08.010
- Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58(3):387-392. doi:10.1016/0304-3959(94)90133-3
- Hauk L. Management of chronic pain and opioid misuse: a position paper from the AAFP. Am Fam Physician. 2017;95(7):458-459.
Lead Author
Nida S. Awadallah, MD
Affiliations: Department of Family Medicine, University of Colorado School of Medicine, Aurora, CO
Co-Authors
Vanessa Rollins, PhD - Department of Family Medicine, University of Colorado School of Medicine, Aurora, CO
Alvin B. Oung, PharmD - University of Wyoming School of Pharmacy, Laramie, WY
Miriam Dickinson, PhD - Department of Family Medicine, University of Colorado School of Medicine, Aurora, CO
Dionisia de la Cerda, MPA - Department of Family Medicine, University of Colorado School of Medicine, Aurora, CO
Susan Calcaterra, MD, MPH - Department of Medicine, Division of General Internal Medicine, University of Colorado School of Medicine, Aurora, CO
Jeremy Orr, MD, MPH - Project Connect Inc, Seattle, WA
Marc Grushan, MD - TRU Community Care, Lafayette, CO
Corresponding Author
Nida S. Awadallah, MD
Correspondence: University of Colorado School of Medicine, Department of Family Medicine, 12631 E. 17th Ave, Mail Stop F496, Aurora, CO 80045. 440-773-5040.
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.