Background and Objectives: The family medicine (FM) clerkship is appropriate for incorporating musculoskeletal ultrasound (MSKUS) education, as many outpatient visits in primary care occur for musculoskeletal (MSK) concerns. Despite rising popularity of point-of-care imaging in primary care, ultrasound (US) training in medical education is limited due to lack of resources and time. The purpose of this study is to evaluate the effects of an MSKUS workshop in the FM clerkship through student self-evaluations.
Methods: Seventy-five medical students enrolled in the FM clerkship during the 2019-2020 academic year participated in hands-on MSKUS workshops staffed by faculty, residents, and a fellow. Workshops coincided with FM residency didactic teaching, allowing for protected time to host US training. Of workshop participants, 98.6% completed both pre- and postworkshop evaluations assessing confidence and acceptability of the workshop (rated on a 0-10 Likert scale, where higher scores represent more confidence or greater benefit, respectively).
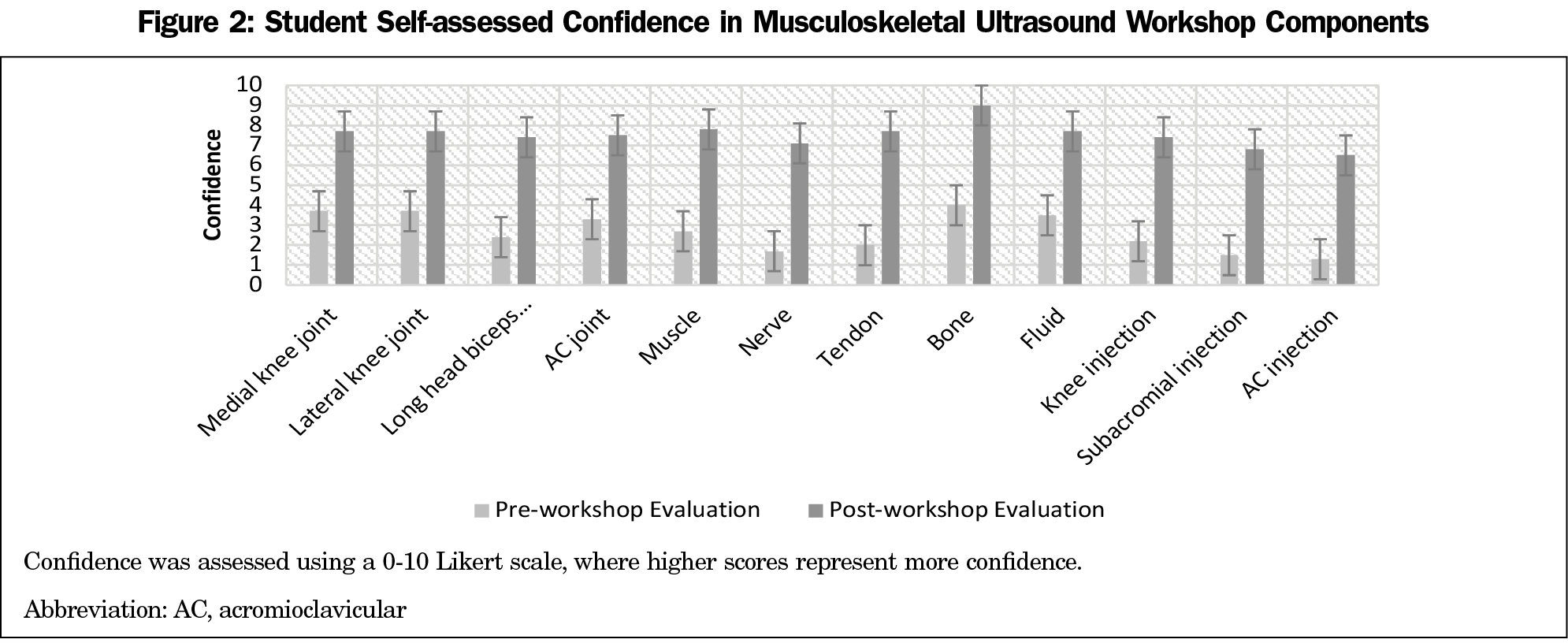
Results: Students noted increased confidence with use of ultrasound, recognition of MSK structures, and performance of landmark-guided procedures (preworkshop 2.6±1.6; postworkshop 7.4±1.1). Students endorsed high levels of agreement in the benefit of the workshop to their education (9.4±1.3) and MSK understanding (9.4±1.2).
Conclusions: This study demonstrates the benefit of an MSKUS workshop as part of the FM clerkship and addresses previously identified challenges to providing US education. Results suggest a short-term benefit from an MSKUS workshop in confidence in MSKUS knowledge and satisfaction with the curriculum.
Ultrasound (US) imaging has gained notoriety for its diagnostic and interventional uses in the primary care setting and is becoming more common in medical education.1-5 The family medicine (FM) clerkship is well positioned to incorporate US education to evaluate musculoskeletal (MSK) conditions given high volumes of patient visits for MSK concerns, of which conditions of the knee and shoulder are common.6 Approximately 39% of outpatient visits for MSK conditions occur in the primary care setting, therefore it is important to ensure adequate MSK training.7
Studies evaluating MSKUS education for medical students and residents suggest this training enhances MSK knowledge and examination skills.8-11 While literature exists evaluating MSKUS education in FM residency and preclinical training, little is known about the benefit of MSKUS in the FM clerkship. Additionally, despite the benefit of US training in medical education, creating a sustainable curriculum has barriers that threaten implementation, such as lack of time, resources, and faculty.12
Therefore, there is a need for a concise yet thorough curriculum during medical training addressing US use and MSK anatomy while utilizing available resources and time. In this study, we evaluate the effects of an MSKUS workshop in the FM clerkship through student self-assessments.
Study Population
The East Carolina University (ECU) Institutional Review Board approved this study as exempt. Seventy-five third-year medical students from ECU Brody School of Medicine completed the FM clerkship during the 2019-2020 academic year. The school is located in Greenville, North Carolina, and consists of approximately 320 medical students. Students earned participation credit by completing evaluations.
Teaching Methods and Equipment
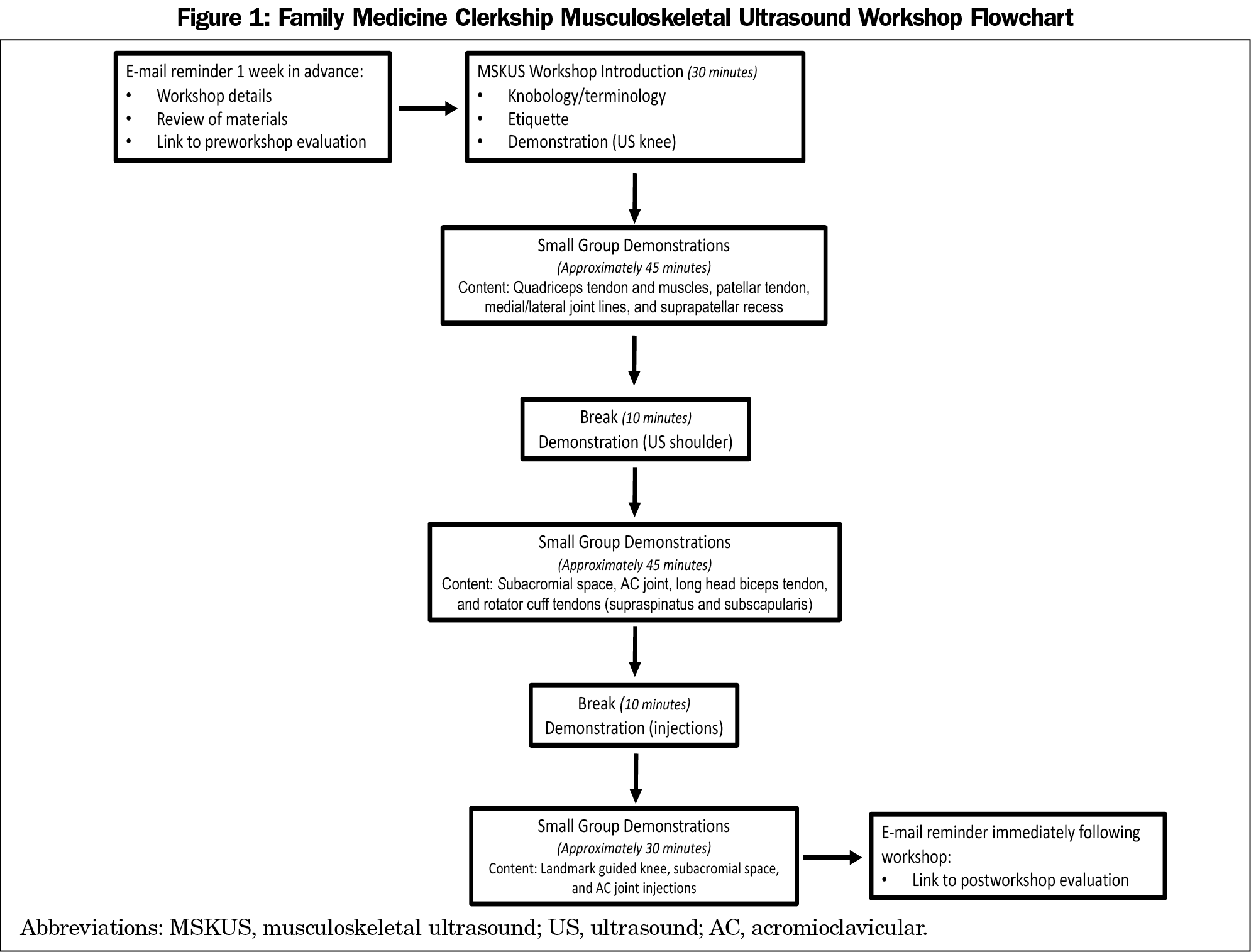
The outline of the MSKUS workshop is provided in Figure 1. Students prepared for the workshop by completing assigned reading. Twelve workshops occurred during the academic year, hosting four to eight students each. Three facilitators, including one attending physician trained in MSKUS, attended each 3-hour workshop. Facilitators reviewed basic US skills (knobology, US terminology and etiquette, MSK anatomy, and US structure identification) as applied to the anterior knee and shoulder, followed by demonstration of landmark-guided MSK injections (subacromial, acromioclavicular, and knee). After large-group review and demonstration, students and facilitators formed small groups (≤3 students, one facilitator, one live MSK model, one US unit) for hands-on training. Groups utilized GE Venue 50 Ultrasound System units and live models through the simulation center.
Evaluation and Data Analysis
Students completed pre- and postworkshop evaluations through a secure web-based platform (Qualtrics, LLC, Provo, UT). Students rated confidence on a 0-10 Likert scale, with higher scores noting more confidence. In addition to evaluating confidence in workshop components, questionnaires assessed compliance with preworkshop reading, prior US and MSK injection experience (including hours of experience), and satisfaction with the workshop. Questionnaire categories were scaled for reliability as categorical measures. We calculated Cronbach α coefficients for each of three categories of interest: identification of MSK structures (0.93; four questions), US structure identification (0.88; five questions) and confidence in injections (0.78; three questions), demonstrating survey instrument reliability. A multiple regression analysis evaluated effects of independent covariates (online preworkshop review, prior US use, hours of US experience, prior experience with injections) on differences between pre- and postworkshop scores, noting hours of prior US use as a possible predictor of a small difference between scores. We used a paired-samples t test to evaluate differences between pre- and postworkshop scores using IBM SPSS Statistics for Windows, Version 25.0 (IBM Corp, Armonk, NY).
Of the 75 students participating in the workshop, 74 completed both pre- and postworkshop evaluations (98.6%). Most students completed the preworkshop reading (91.9%), and less than half endorsed prior experience administering MSK injections (41.9%). Only 10% of students had prior US experience, and average hours of prior US use was minimal (2.7±4).
Pooled data from questions regarding workshop components are demonstrated in Figure 2, showing overall higher levels of confidence following the intervention. A paired samples t test revealed significant improvement in overall confidence levels from preworkshop (2.6±1.6) to postworkshop assessments (7.4±1.1; P<.001). Minimal variation of mean Likert scores by cohort for pre- and postworkshop assessments suggests workshop timing throughout the year did not influence scores. Students agreed with usefulness of the online prereading (7.3+2.6), the live presentation (9.0+1.5), the overall benefit of the workshop (9.4+1.3), and in understanding MSK medicine (9.4+1.2) through the postworkshop evaluations, noting an overall favorable experience.
We found integration of an MSKUS workshop into the FM clerkship improves student confidence in the use of US, MSK structure identification, and MSK injections. Students endorsed usefulness of workshop components to their education, and it was received well overall.
Our workshop addresses previously identified challenges to US education delivery in medical training. As few medical schools offer an US curriculum (27%) and recognize personnel, funding, and time as limiting factors,12 we effectively hosted an MSKUS experience with postgraduate physicians and simulation center resources. Maintaining low student-to-facilitator ratios follows recommendations endorsing small-group US teaching to optimize learning.13,14 The 3-hour time frame fit within the clerkship schedule and occurred during the FM residency didactic session, allowing for availability of facilitators, faculty, and students to participate. By offering participation credit, our evaluation benefited from timely survey completion and significant participation. While an objective measure of acquired skill was not included, other studies demonstrated objective findings of improved palpation skills and objective structured clinical examination (OSCE) scores after incorporating an MSKUS curriculum.3,10,11,15 A comparison of FM clerkship grades, MSK knowledge, and examination skills between students participating in an MSK workshop both with and without US may strengthen a broad recommendation for incorporation of MSKUS in the curriculum.
In conclusion, an MSKUS workshop in the FM clerkship is feasible, and student feedback suggests this is a favorable educational experience that improves confidence in US and MSK medicine. There is potential for an introduction to MSKUS during the FM clerkship, providing increased exposure to point-of-care imaging and addressing MSK education needs. Similar workshops may prove enriching as an introduction to basic US concepts and improve confidence in MSK anatomy, identification, and skills.
Acknowledgments
The study team acknowledges the faculty and staff of the Interprofessional Clinical Simulation Program at the Brody School of Medicine for providing equipment, standardized patients, and operational support for the MSKUS workshop.
Presentations: A preliminary report presenting early data prior to complete data collection was presented as a virtual poster presentation at the American Medical Society of Sports Medicine Conference (April 24-29, 2020).
References
- Dietrich CF, Hoffmann B, Abramowicz J, et al. Medical student ultrasound education: a WFUMB position paper, part I. Ultrasound Med Biol. 2019;45(2):271-281. Review. doi:10.1016/j.ultrasmedbio.2018.09.017
- Kondrashov P, Johnson JC, Boehm K, Rice D, Kondrashova T. Impact of the clinical ultrasound elective course on retention of anatomical knowledge by second-year medical students in preparation for board exams. Clin Anat. 2015;28(2):156-163. doi:10.1002/ca.22494
- Dinh VA, Frederick J, Bartos R, Shankel TM, Werner L. Effects of ultrasound implementation on physical examination learning and teaching during the first year of medical education. J Ultrasound Med. 2015;34(1):43-50. doi:10.7863/ultra.34.1.43
- Tarique U, Tang B, Singh M, Kulasegaram KM, Ailon J. Ultrasound curricula in undergraduate medical education: a scoping review. J Ultrasound Med. 2018;37(1):69-82. doi:10.1002/jum.14333
- Hall JW, Holman H, Bornemann P, et al. Point of care ultrasound in family medicine residency programs: a CERA study. Fam Med. 2015;47(9):706-711.
- Houston TK, Connors RL, Cutler N, Nidiry MA. A primary care musculoskeletal clinic for residents: success and sustainability. J Gen Intern Med. 2004;19(5 Pt 2):524-529. doi:10.1111/j.1525-1497.2004.30173.x
- United States Bone and Joint Decade. The Burden of Musculoskeletal Diseases in the United States. 2nd ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2010.
- Mehta P, Rand EB, Visco CJ, Wyss J. Resident accuracy of musculoskeletal palpation with ultrasound verification. J Ultrasound Med. 2018;37(7):1719-1724. doi:10.1002/jum.14523
- Knobe M, Münker R, Sellei RM, et al. Peer teaching: a randomised controlled trial using student-teachers to teach musculoskeletal ultrasound. Med Educ. 2010;44(2):148-155. doi:10.1111/j.1365-2923.2009.03557.x
- Walrod BJ, Schroeder A, Conroy MJ, et al. Does ultrasound-enhanced instruction of musculoskeletal anatomy improve physical examination skills of first-year medical students? J Ultrasound Med. 2018;37(1):225-232. doi:10.1002/jum.14322
- So S, Patel RM, Orebaugh SL. Ultrasound imaging in medical student education: impact on learning anatomy and physical diagnosis. Anat Sci Educ. 2017;10(2):176-189. doi:10.1002/ase.1630
- Dinh VA, Fu JY, Lu S, Chiem A, Fox JC, Blaivas M. Integration of ultrasound in medical education at United States medical schools: a national survey of directors’ experiences. J Ultrasound Med. 2016;35(2):413-419. doi:10.7863/ultra.15.05073
- Patel SG, Benninger B, Mirjalili SA. Integrating ultrasound into modern medical curricula. Clin Anat. 2017;30(4):452-460. doi:10.1002/ca.22864
- Celebi N, Griewatz J, Malek NP, Krieg S, Kuehnl T, Muller R, Pauluschke-Fröhlich J, Debove I, Riessen R, Zipfel S, Fröhlich E. Development and implementation of a comprehensive ultrasound curriculum for undergraduate medical students - a feasibility study. BMC Med Educ. 2019 May 28;19(1):170. doi: 10.1186/s12909-019-1611-1.
- Woods R, Wisniewski SJ, Lueders DR, Pittelkow TP, Larson DR, Finnoff JT. Can ultrasound be used to improve the palpation skills of physicians in training? A prospective Study. PM R. 2018;10(7):730-737. doi:10.1016/j.pmrj.2017.11.016



There are no comments for this article.