Background and Objectives: Educational components and electives that may influence medical student choice of primary care careers have been studied individually, but not reviewed or synthesized. Examining educational components and electives in a comprehensive manner may inform evidence-based approaches to raise the number of primary care physicians in the United States and help optimize use of finite resources. We sought to determine evidence-based educational components and electives associated with increased medical student choice of primary care careers.
Methods: We searched PubMed, Scopus, and CINAHL for undergraduate medical education articles in English describing an educational component or elective and outcome relevant to primary care specialty choice. We assessed titles, then abstracts, and finally full texts for inclusion in a narrative synthesis.
Results: The searches returned 11,211 articles and we found 42 that met the inclusion criteria. The most described components were outpatient clinical rotations, preclinical courses, and preceptorships. The most common electives were international health, summer preceptorships, and rural medicine. While most articles described curricula that appeared to have a positive correlation with primary care specialty choice, six articles found limited benefit. In sum, results were mixed.
Conclusions: The current literature is limited, and many contemporary electives have not been studied with respect to primary care choice. Increased attention and funding to studying the impact of electives and other educational components on primary care specialty choice is warranted.
Primary care (PC) that is longitudinal, comprehensive, coordinated, and person-centered decreases disparities, improves health system performance, and reduces mortality.1–3 PC supports the quintuple aim of enhanced patient outcomes, population health, health equity, and clinician well-being at lower costs.4 Despite these benefits, the United States faces a PC shortage.5,6 To address this gap, increased attention to the PC workforce is needed.7,8 One way to develop the PC workforce is through medical education programs.
Medical school electives are common, positively reviewed, and effectively increase student knowledge.9 However, the influence of electives on PC specialty choice is uncertain. Additionally, medical education programs contain components within courses or clerkships that could impact specialty choice. While knowledge, attitudes, and satisfaction have been assessed for some educational components,10–13 their impact on PC selection is less certain. We explored how electives and other educational components impact student choice of PC specialties.
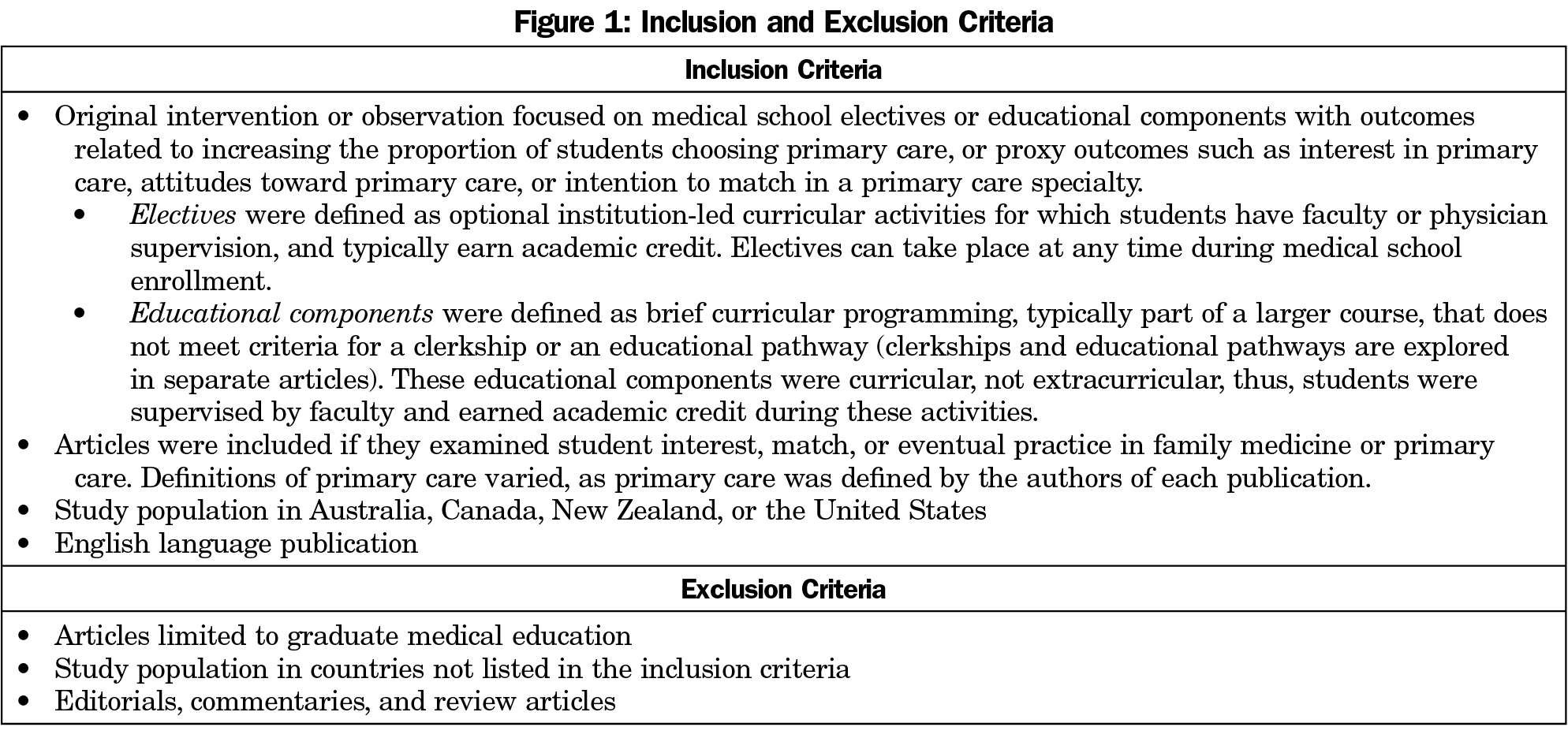
We performed a review and narrative synthesis of relevant literature.14 Starting with publications identified by a scoping review,15 we searched MEDLINE (PubMed) and Education Resources Information Center (ERIC) databases for additional original research focused on electives and educational components from index inception to April 14, 2020, using search terms developed with a language mapping process.15 We used keywords and database-specific controlled vocabulary to describe concepts of choice behavior, family and PC physicians, medical education, curricula, and electives with subsequent citation chaining in Scopus to ensure comprehensiveness. Inclusion and exclusion criteria are shown in Figure 1 and search terms are shown in Appendix A (https://journals.stfm.org/media/4917/nguyen-fm-v54appendixa.pdf).
All articles were independently assessed for inclusion by two authors. When assessments differed, authors discussed to reach consensus. We defined electives as optional educational experiences led by institutions; and educational components as modules, class sessions, or other elements within a course, clinical rotation, or educational program. We categorized studies by theme, study design, institutional characteristics, and effectiveness.
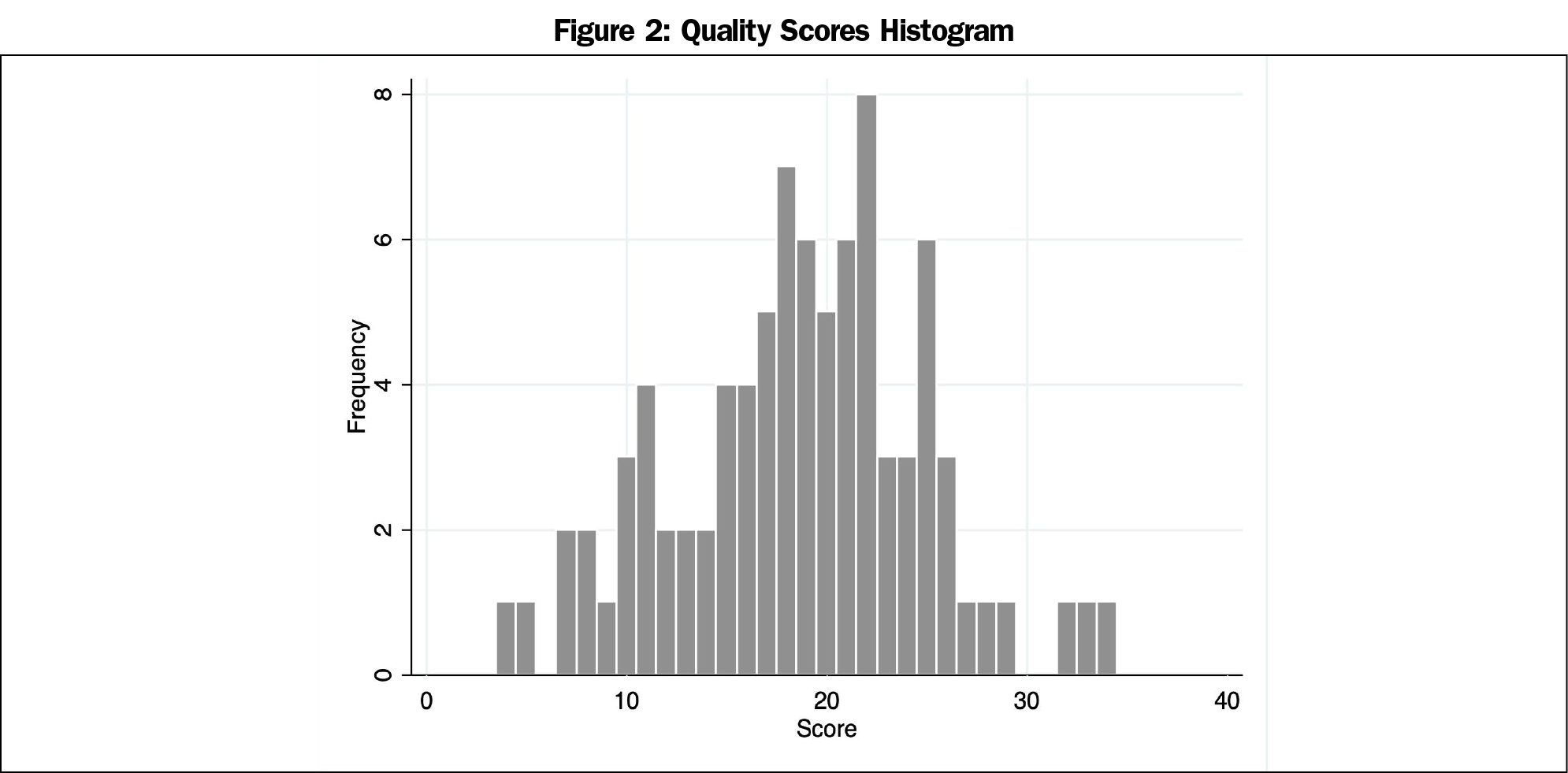
We assessed the quality of included articles using the 16-item quality assessment tool (QATSDD; maximum possible score=48), that was developed to examine studies with varied methodologies.16 Each article was evaluated by two authors, who discussed scoring discrepancies larger than one standard deviation until consensus was achieved.
Our study was determined to be non-human subjects research by the Michigan State University Institutional Review Board.
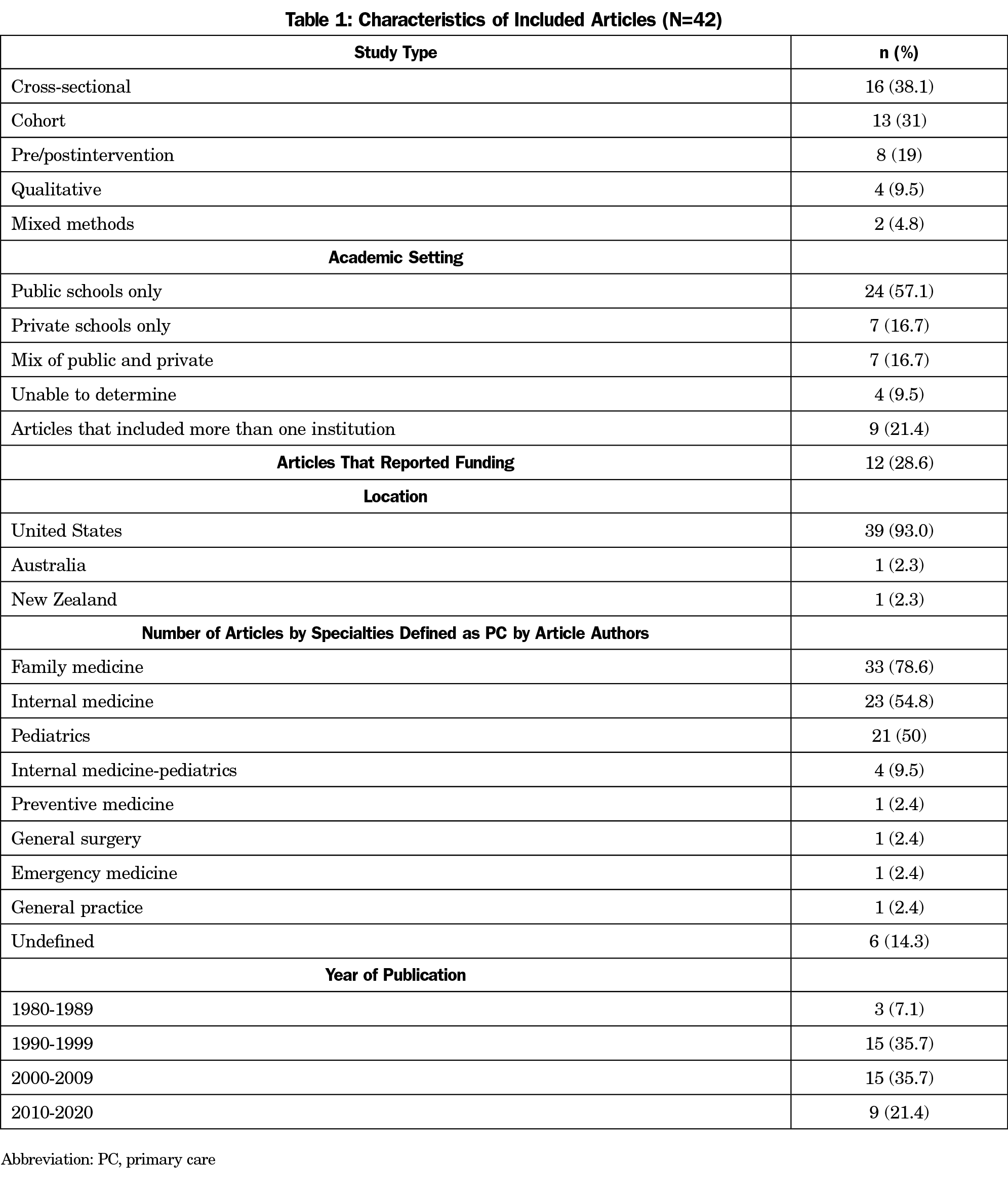
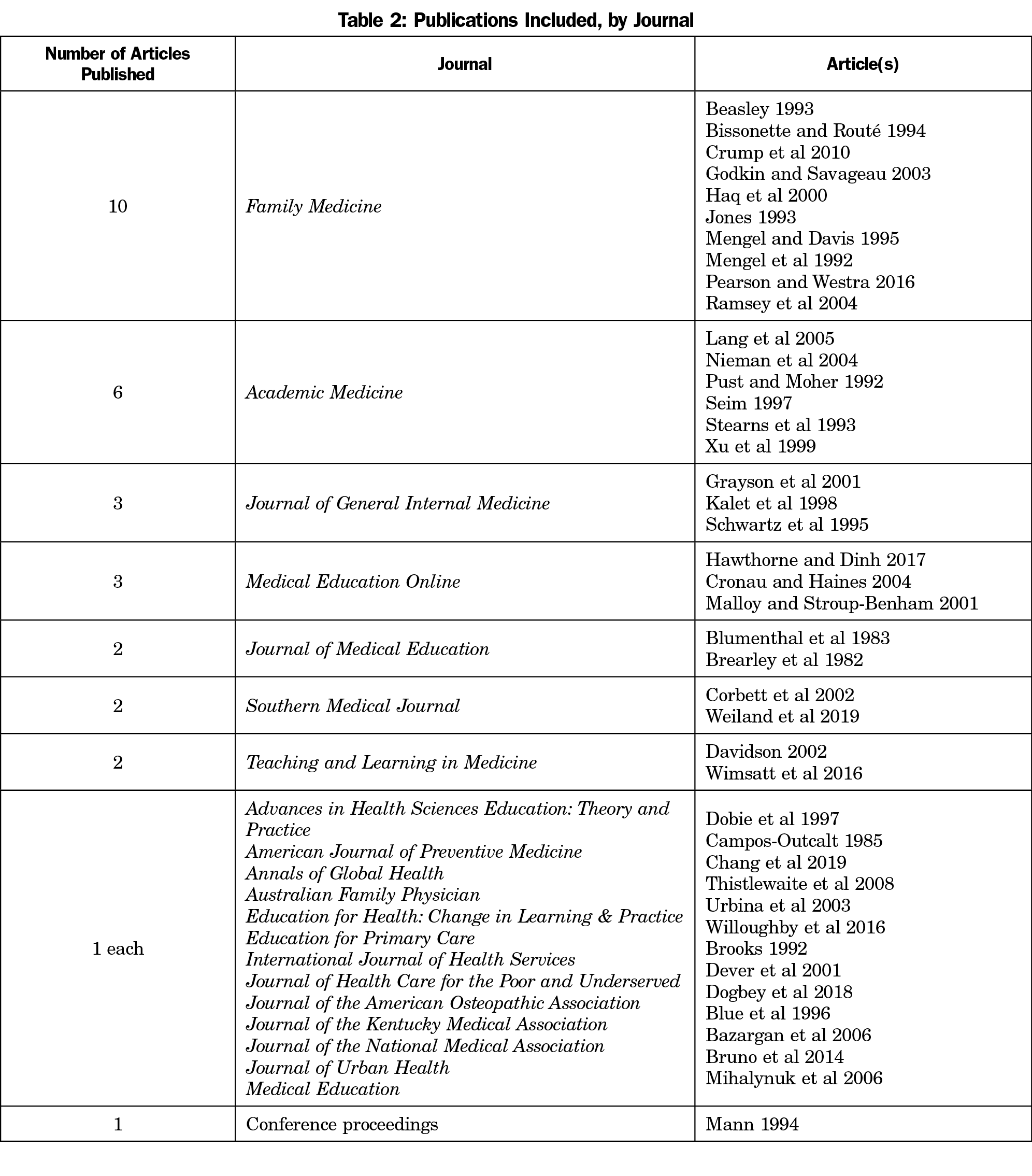
The scoping review identified 33 articles. Our secondary search found 1,784 articles post-deduplication, including nine that met inclusion criteria, for a total of 42 included studies. Most used cross-sectional or cohort designs and were conducted at US public medical schools (Table 1). Less than one-third described funding sources or were multi-institutional, and the specialties included as PC varied. More than half were published in four journals (Table 2). About half described electives and half described other educational components.
Quality scores ranged from 4 to 34 with a mean (SD) score of 18.6 (6.2) and a median score of 19 (Figure 2). Six articles found no benefit17–22 or a negative impact23 from the studied intervention; all others described interventions that appeared to have a positive influence on PC specialty choice.
International health and summer preclinical experiences were the most described electives. Outpatient clinical rotations were the most studied educational components. All showed an association between participation and interest in, or selection of, a PC residency. One study found that intention to participate had as much impact on specialty choice as actual participation, suggesting the experience reflects student interests, but may not influence specialty choice.21 Another noted the difference in FM specialty choice was not significant between program participants and those who applied, but were not accepted.24
Studies examining preclinical exposure to generalist courses or longitudinal FM experiences had mixed results. One article did not find preclinical exposure to FM faculty to be influential17 while others did.25,26 Another study reported a longitudinal clinical experience during preclinical years did not increase students’ interest in or selection of a PC career,21 whereas others were successful.27,28
Studies conducted prior to the widespread adoption of required FM clerkships found some benefit from ambulatory experiences on PC specialty choice.29,30 Nonetheless, more recent studies showed no effect.20,21 Furthermore, a survey of 123 departments found that community medicine experiences in private schools may be associated with lower family medicine match rates.23
Most electives and educational components studied were associated with PC specialty choice. While this may reflect a publication bias toward positive findings, seven of 42 did not show a benefit of the studied intervention.
International health and summer preclinical electives were positively associated with FM specialty choice; however, most studies did not control for initial student interest. Few articles examined obstetrics, community medicine, or domestic service-learning experiences. We found no studies that measured the impact of FM electives in addiction medicine, adolescent medicine, hospice/palliative care, integrative health, geriatrics, public health, sleep medicine, sports medicine, or women’s health. Future studies should assess the impact of such electives on PC specialty choice.
Another area that was not explored in the included articles was the potential influence of working with physician faculty or volunteer preceptors who were burned out or dissatisfied with their work. Examining the impression of overworked doctors on learners could be a future consideration.
Many of the interventions described are now common elements of medical education programs. Despite widespread adoption, the PC workforce shortage persists, suggesting the need for further curricular innovation. While some interventions were designed to produce more PC physicians,21,23,27,28,31–33 others reflected shifts in clinical practice20 or did not describe intent in their development.17,30,34,35
Given most studies were descriptive, cross-sectional, or single institution, results are difficult to generalize and causality cannot be determined. Few studies were funded and most of those were cross-sectional surveys. Increased support for PC educational research could improve its scope and quality.
This study is limited by the heterogeneity and methodological rigor of the identified articles. Also, 33 of the studies were published before 2010, and their relevance to contemporary medical education is uncertain.
We conclude that some electives and educational components are associated with PC specialty choice. However, the current literature is limited, contemporary electives have not been adequately studied, and none describe clear causation between intervention and specialty choice. Increased attention and funding are needed to develop more robust research in this area. Career choice is a complex issue and electives and educational components are only one contributing factor.
- NAPCRG Annual Meeting, November 20-24, 2020 (virtual)
- STFM Conference on Medical Student Education, February 1-4, 2021 (virtual)
- STFM Annual Spring Conference, May 3-7, 2021 (virtual)
Acknowledgments
The authors thank Deborah Erlich, Esther Guard, Amanda Kost, Christy Ledford, Amy Lee, Morgan Pratte, Mimi Raleigh, Tomoko Sairenji, and Dean Seehusen for developing the list of articles, discussions, and providing feedback.
Financial Support: This project was partially supported by a grant from the American Board of Family Medicine Foundation (J. Phillips, PI), and partially by the Health Resources and Services Administration (HRSA) of the United States Department of Health and Human Services (HHS) under grant number D54HP23297, “Academic Administrative Units” (C. Morley, PI). This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by AAFP, HRSA, HHS, or the US Government.
Conflict Disclosure: Author B. Nguyen owns equity in Abbvie, a biopharmaceutical research and development corporation, but it is not in conflict with the topic of this study.
Presentations: Preliminary findings have been presented at the following conferences:
- NAPCRG Annual Meeting, November 20-24, 2020 (virtual)
- STFM Conference on Medical Student Education, February 1-4, 2021 (virtual)
- STFM Annual Spring Conference, May 3-7, 2021 (virtual)
References
- Phillips RL Jr, Starfield B. Why does a U.S. primary care physician workforce crisis matter? Am Fam Physician. 2003;68(8):1494-1500, 1496-1498, 1500.
- Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of primary care physician supply with population mortality in the United States, 2005-2015. JAMA Intern Med. 2019;179(4):506-514. doi:10.1001/jamainternmed.2018.7624
- Starfield B. Primary Care and Equity in Health: The importance to effectiveness and equity of responsiveness to peoples’ needs. Humanity Soc. 2009;33(1-2):56-73. doi:10.1177/016059760903300105
- Committee on Implementing High-Quality Primary Care, Board on Health Care Services, Health and Medicine Division, National Academies of Sciences, Engineering, and Medicine. Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care. (McCauley L, Phillips RL, Meisnere M, Robinson SK, eds.). Washington, DC: National Academies Press; 2021. Accessed June 14, 2021. https://www.nap.edu/catalog/25983
- West CP, Dupras DM. General medicine vs subspecialty career plans among internal medicine residents. JAMA. 2012;308(21):2241-2247. doi:10.1001/jama.2012.47535
- Petterson SM, Liaw WR, Phillips RL Jr, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010-2025. Ann Fam Med. 2012;10(6):503-509. doi:10.1370/afm.1431
- Prunuske J. America Needs More Family Doctors: The 25x2030 Collaborative aims to get more medical students into family medicine. Am Fam Physician. 2020;101(2):82-83.
- Council on Graduate Medical Education. Twentieth Report: Advancing Primary Care. COGME; 2010:1-53. Accessed April 22, 2021. https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/graduate-medical-edu/reports/archive/2010.pdf
- Agarwal A, Wong S, Sarfaty S, Devaiah A, Hirsch AE. Elective courses for medical students during the preclinical curriculum: a systematic review and evaluation. Med Educ Online. 2015;20(1):26615. doi:10.3402/meo.v20.26615
- Kyaw BM, Posadzki P, Paddock S, Car J, Campbell J, Tudor Car L. Effectiveness of digital education on communication skills among medical students: systematic review and meta-analysis by the Digital Health Education Collaboration. J Med Internet Res. 2019;21(8):e12967. doi:10.2196/12967
- Chokshi B, Chen KD, Beers L. Interactive case-based childhood adversity and trauma-informed care electronic modules for pediatric primary care. MedEdPORTAL. 2020;16(1):10990. doi:10.15766/mep_2374-8265.10990
- Lewin LO, Singh M, Bateman BL, Glover PB. Improving education in primary care: development of an online curriculum using the blended learning model. BMC Med Educ. 2009;9(1):33. doi:10.1186/1472-6920-9-33
- Wilechansky R, Burgermaster M, Jones D, Seres D. Obesity, diet, and exercise education for the primary care clerkship using an articulate storyline 2 e-learning module. MedEdPORTAL. 2016;12(1):mep_2374-8265.10497. doi:10.15766/mep_2374-8265.10497
- Sutton A, Clowes M, Preston L, Booth A. Meeting the review family: exploring review types and associated information retrieval requirements. Health Info Libr J. 2019;36(3):202-222. doi:10.1111/hir.12276
- Phillips JP, Wendling AL, Prunuske J, et al. Medical school characteristics, policies, and practices that support primary care specialty choice: a scoping review of five decades of research. Fam Med. 2022;54(7):xxx-xx.
- Sirriyeh R, Lawton R, Gardner P, Armitage G. Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Pract. 2012;18(4):746-752. doi:10.1111/j.1365-2753.2011.01662.x
- Beasley JW. Does teaching by family physicians in the second year of medical school increase student selection of family practice residencies? Fam Med. 1993;25(3):174-175.
- Brooks CH. Do area health education center programs produce primary care specialists? Results of a longitudinal study. Int J Health Serv. 1992;22(3):567-578. doi:10.2190/FLCX-NYD9-MBUA-FYJ5
- Dogbey GY, Collins K, Russ R, Brannan GD, Mivsek M, Sewell S. Factors associated with osteopathic primary care residency choice decisions. J Am Osteopath Assoc. 2018;118(4):225-233. doi:10.7556/jaoa.2018.046
- Kalet A, Schwartz MD, Capponi LJ, Mahon-Salazar C, Bateman WB. Ambulatory versus inpatient rotations in teaching third-year students internal medicine. J Gen Intern Med. 1998;13(5):327-330. doi:10.1046/j.1525-1497.1998.00099.x
- Malloy MH, Stroup-Benham CA. Impact of generalist physician initiatives on residency selection. Med Educ Online. 2001;6(1):4524. doi:10.3402/meo.v6i.4524
- Mann MP. A Light at the End of the Tunnel: The Impact of Early Clinical Experiences on Medical Students. Presented at: American Educational Association Research Conference; April 1994; New Orleans, LA.
- Wimsatt LA, Cooke JM, Biggs WS, Heidelbaugh JJ. Institution-specific factors associated with family medicine residency match rates. Teach Learn Med. 2016;28(3):269-278. doi:10.1080/10401334.2016.1159565
- Jones JE. The effect of a student summer assistantship program in family medicine on specialty selection. Fam Med. 1993;25(3):176-178.
- Brearley WD, Simpson W, Baker RM. Family practice as a specialty choice: effect of premedical and medical education. J Med Educ. 1982;57(6):449-454. doi:10.1097/00001888-198206000-00004
- Mengel MB, Davis AB. Required first-year generalist clinical experience courses and their relationship to career choice: the critical effect of family medicine involvement. Fam Med. 1995;27(10):652-657.
- Urbina C, Solan B, Counsellor A, Mines J, Serna L, Kalishman S. “Where have all the students gone?” Retaining medical school graduates through educational innovations. Educ Health (Abingdon). 2003;16(3):279-285. doi:10.1080/13576280310001607451
- Willoughby KA, Rodríguez C, Boillat M, et al. Assessing students’ perceptions of the effects of a new Canadian longitudinal pre-clerkship family medicine experience. Educ Prim Care. 2016;27(3):180-187. doi:10.1080/14739879.2016.1172033
- Schwartz MD, Linzer M, Babbott D, Divine GW, Broadhead WE; The Society of General Internal Medicine Task Force on Career Choice in Internal Medicine. The impact of an ambulatory rotation on medical student interest in internal medicine. J Gen Intern Med. 1995;10(10):542-549. doi:10.1007/BF02640362
- Blue AV, Donnelly MB, Harrell-Parr P, Murphy-Spencer A, Rubeck RF, Jarecky RK. Developing generalists for Kentucky. J Ky Med Assoc. 1996;94(10):439-445.
- Dever GEA, Eveland AP, Tedders SH, Fehlenberg RD, Laurens MB, Harrelson JC. Impact of a population-based medical curriculum on specialty choice. J Health Care Poor Underserved. 2001;12(3):261-271. doi:10.1353/hpu.2010.0817
- Blumenthal DS, McNeal-Steele MS, Bullard LL, Daniel SL, Satcher D. Introducing preclinical students to primary care through a community preceptorship program. J Med Educ. 1983;58(3):179-185. doi:10.1097/00001888-198303000-00003
- Hawthorne MR, Dinh A. Meeting the demand of the future: a curriculum to stimulate interest in careers in primary care internal medicine. Med Educ Online. 2017;22(1):1340780. doi:10.1080/10872981.2017.1340780
- Stearns J, Glasser M, Miller B, Flach D, Cowen J. A longitudinal ambulatory care clerkship: graduates’ reports on the effect on specialty choice and preparation for residency. Acad Med. 1993;68(10)(suppl):S37-S39. doi:10.1097/00001888-199310000-00039
- Corbett EC Jr, Owen JA, Hayden GF. Effect of a second-year primary care preceptorship on medical students’ career plans. South Med J. 2002;95(7):691-694. doi:10.1097/00007611-200295070-00007



There are no comments for this article.