Background and Objectives: Medical schools should understand how to matriculate students who are more likely to enter primary care specialties and put admissions processes into place that achieve this result. However, there are no existing reviews that have systematically evaluated medical school admission practices and primary care specialty choice.
Methods: We conducted a narrative synthesis utilizing a systematic literature search to evaluate the effectiveness of medical school admission strategies designed to increase the percentage of graduates entering primary care specialties.
Results: We included 34 articles in the narrative review. Multiple prematriculation programs that appear to produce students with a high likelihood of entering primary care have been described in the literature. However, all of these studies are from single institutions, were observational, and limited by selection bias. Applicants who self-identify an interest in primary care, grew up with a rural background, and are older at matriculation are more likely to enter primary care, with stated interest in primary care being most predictive. Gender and race have been associated with primary care specialty choice in some studies, but not all. Insufficient literature on admissions policies and procedures exists to draw conclusions about best practices.
Conclusions: Medical schools that want to increase the percentage of graduates entering primary care should consider developing a prematriculation program that attracts and prepares motivated and talented students with primary care interest. Admissions committees should understand which demographic criteria are associated with increased likelihood of entering primary care. The most important identifiable trait is an applicant’s stated interest in primary care.
The overall trend toward specialization in American medicine, combined with a payment structure tilted toward the same has resulted in a declining interest in primary care among medical students.1 General lack of prestige and financial disincentives have contributed to a significant shortage of primary care physicians.1,2 This shortage is likely to grow even larger in the coming years.3 As a result, there is interest in what medical schools can do to increase the number of students who enter primary care specialties.4
Additionally, because primary care physicians offer high-quality care at a lower cost, increasing the percentage of graduates entering primary care will improve the overall health of the nation.5,6 In response to this need, family medicine, as a specialty, has adopted a collective goal of 25% of medical students entering family medicine by 2030.7 There has been a slight increase in the proportion of US medical students entering family medicine over the last decade, which is mostly driven by an increase in the percentage of osteopathic medical students entering the National Residency Matching Program match,8 but this is not sufficient to meet population based needs.
One strategy to increase the number of graduates entering primary care careers is to modify medical school admissions to matriculate a larger proportion of applicants likely to go into primary care upon graduation. The admissions process and the characteristics of applicants selected are two potentially modifiable variables. The purpose of this study was to review and synthesize existing literature that describes medical school admissions practices and how they relate to the percentage of graduates entering primary care.
Approach
We conducted a narrative synthesis using a comprehensive and systematic literature search to identify medical school admission strategies designed to increase the percentage of graduates entering primary care specialties.9 Narrative synthesis was chosen for two reasons. First, it allows researchers to summarize the evidence collected from a wide mixture of methodologies, which reflects this body of literature. Second, it allows researchers to distill this information into a narrative description, enabling qualitative understanding and a descriptive, concise analysis of the current state of the literature.10
Data Retrieval
We obtained articles in the topic area of medical school admissions initially from those meeting inclusion criteria in a previous scoping review, which broadly examined medical school structures, curricula, admission practices, and other characteristics that promote primary care specialty choice by medical students.4 To supplement this initial search and ensure a comprehensive evidentiary base for the narrative review, we conducted additional searches in Medline (PubMed) and Education Resource Information Center (ERIC) on February 27, 2020. We used topic-specific subject headings and free-text terms developed through language mapping from the scoping review process. We included terms that described the concepts of medical education, medical students, primary care, career decision making, and admissions variables such as matriculation, acceptance, and the term “School Admission Criteria” [MeSH]. Finally, we performed citation chaining on relevant articles to make certain no pertinent published literature was missed.
Article Selection
Two medical librarians crafted and ran the searches, collated the citations, assisted with manuscript retrieval, and performed citation chaining in Scopus and Google Scholar. No time limits were placed on the literature search in order to prevent missing foundational studies and assess for trends over time. We included only English-language, peer-reviewed, published research. Countries of origin considered were the United States, Canada, Australia, and New Zealand, as we felt the medical education and health care workforce structure in these countries are sufficiently similar to be aggregated.
We developed inclusion and exclusion criteria before reviewing the articles. All research studies, regardless of methodology, within the topic’s scope were included. To meet criteria, studies had to describe an outcome meaningfully related to primary care, family medicine, or specialty choice. These outcomes included long-term primary care or family medicine practice; match into a primary care residency or a family medicine residency; student interest in primary care or family medicine; and student attitudes regarding primary care or family medicine. We excluded studies that evaluated outcomes related to internal medicine, pediatrics, or another discipline without a general or primary care focus.
Article titles and abstracts were initially reviewed by a single researcher with expertise in primary care medical education and familiarity with the existing literature. Initially, we kept the threshold to retain articles low. Retained articles were then reviewed by a team of researchers to make final decisions about inclusion. When necessary, we reviewed the full text of an article.
Nonresearch articles, such as commentaries, were excluded. We excluded graduate medical education interventions. We did not exclude studies based on quality. When uncertainty about inclusion existed, we used focused discussion until we reached consensus.
Initially, we reviewed admissions practices and institutional factors and selected them together; we divided these topics into two manuscripts for ease of synthesis. This paper describes the impact of admissions practices on medical student choice of primary care careers.
Article Selection
We identified twenty-one studies related to admission practices from the initial scoping review. The supplemental searches performed in February 2020 retrieved an additional 1,153 articles, of which 13 met inclusion criteria, for a total of 34 articles (see Appendix 1: https://journals.stfm.org/media/4914/raleigh-fm-appendix1.pdf).
All of the articles included were observational studies. Many were secondary analyses of existing databases or single-institution studies. The lack of prospective or comparative studies reduces the generalizability of the findings of this synthesis.
Narrative Synthesis
We found no studies that reported a complete admission process that was shown to lead to a higher rate of graduates choosing primary care. In our review, we categorized the separate aspects of the admissions process, studied in the context of primary care outcomes, that are represented in the literature. These include admission subcommittees, prematriculation programs, targeted premedical recruitment, the influence of applicant characteristics on primary care careers, and admissions processes.
Admission Subcommittees
Two single-institution studies examined admissions committees, and these had mixed results. One 2002 study showed that admissions committee members were very poor at predicting which matriculants would eventually enter primary care.11 Another, published in 1986, compared outcomes of a special admission subcommittee (SAS) that recruited students from a broad range of socioeconomic and cultural backgrounds with graduates admitted through traditional admission processes. The SAS was the result of a 1969 policy to achieve a target of 30% of the matriculants being from diverse backgrounds. A higher percentage of SAS-admitted students ultimately entered a primary care specialty residency.12
Prematriculation Programs
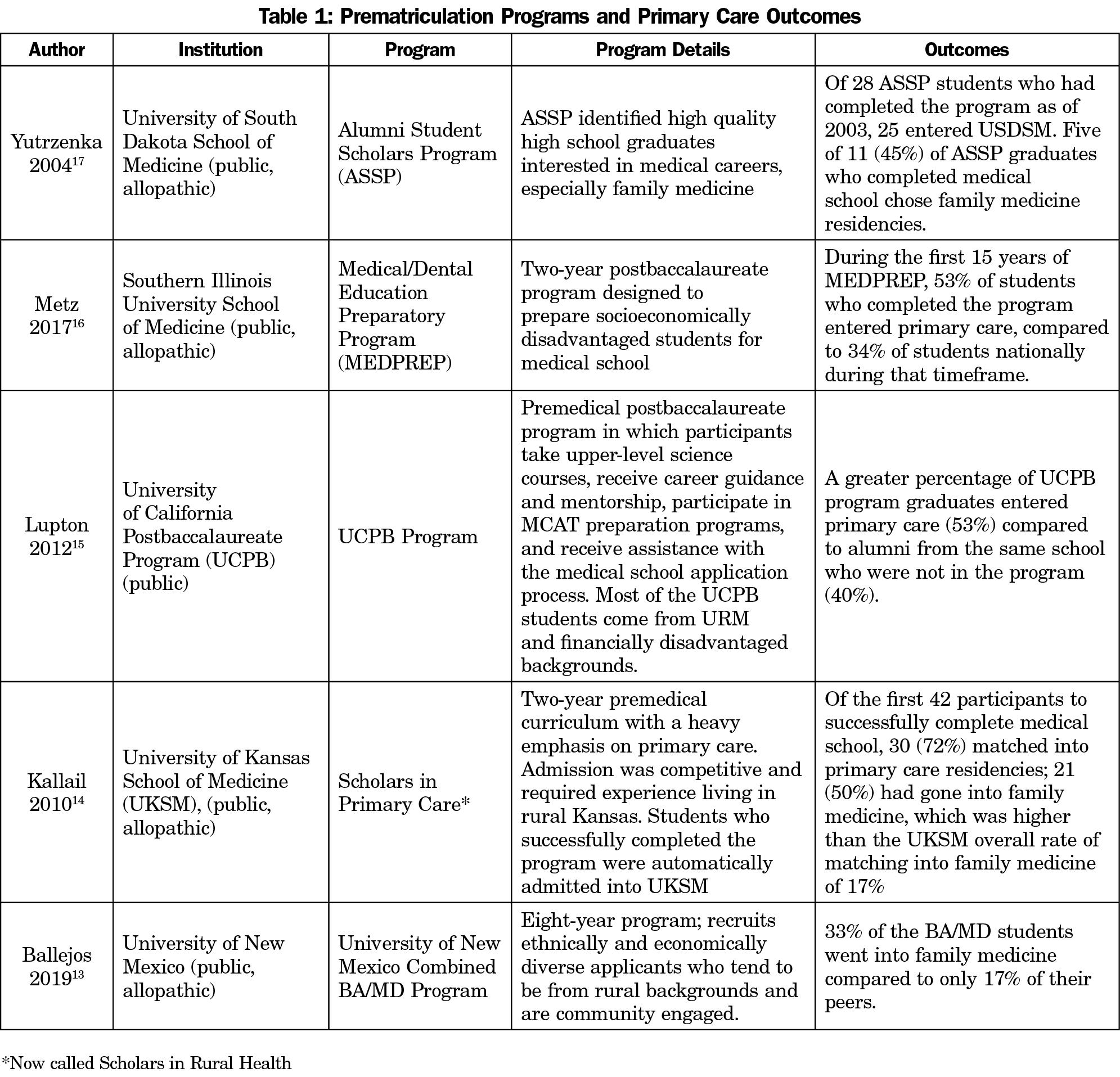
All prematriculation program studies were single-institution studies and each produced a high percentage of primary care graduates. Their populations ranged from high school to postbaccalaureate students, and programs ranged from one to multiple years in length. Many included a community service component.13,15,16 Each of these studies compared the specialty choice of program graduates to other medical students from within the same institution. They found that students who entered medical school through these pathways were more likely to enter primary care residencies. However, as they were single-program studies without control groups, all were limited by selection bias (Table 1).13-17
Targeted Premedical Recruitment
In a national study using Association of American Medical Colleges (AAMC) data from the mid-1990s, one-third of medical schools were found to have premedical recruitment programs targeting future generalists, and students entering schools with such programs were more likely to express an interest in primary care on the Matriculating Student Questionnaire (MSQ), although more definitive outcomes such as residency choice were not studied.18 A 2012 study reported that only 8% of private US medical schools and 32% of public medical schools indicated their admissions practices explicitly favored students with a primary care interest; in logistic regression these schools did have higher percentages of graduates entering family medicine, but the effect was small.19
Applicant Characteristics
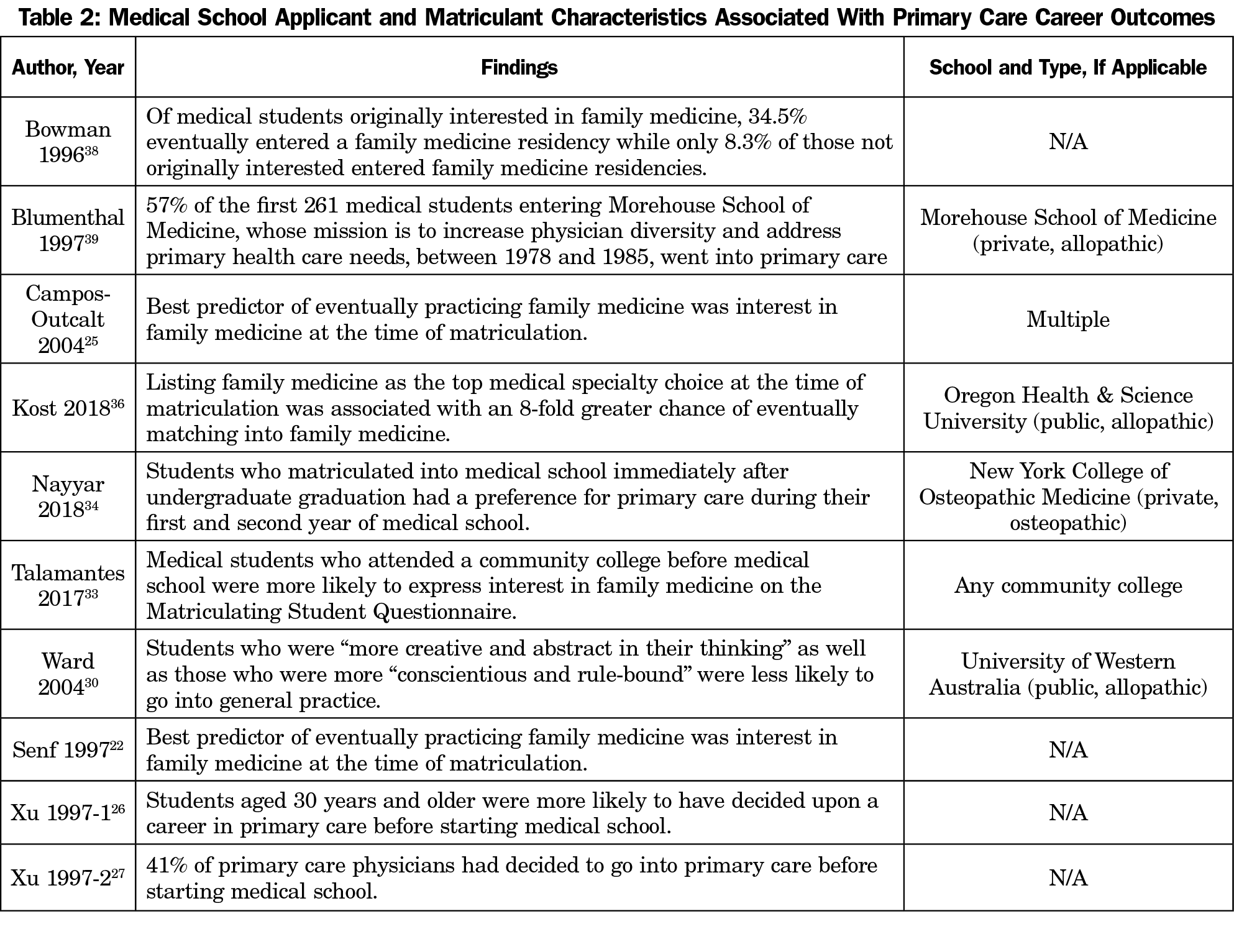
Multiple studies indicate that medical school applicants who express interest in primary care have a greater chance of eventually selecting primary care.11, 20-27 All of these studies compared outcomes between those applicants who expressed interest in primary care and those who did not. Additionally, a retrospective analysis of 3 years of medical school application essays from a single school found that essays by students who eventually entered primary care were more than twice as likely to include a mention of their interest in primary care (Table 2).28
Two demographic factors have consistently been identified over time and across countries to be associated with an eventual career in primary care: rural background,20,22-24,29 and older age at matriculation.20,24,29 Female gender11,22,24,30-32 and being part of an underrepresented minority group20,23,31 show mixed results in the literature. Findings for gender and race varied by the year of publication, the definition of primary care, the study population, and what other variables were controlled.
There are two small studies that suggest specific educational paths that may be associated with primary care career choice. In a national study of AAMC data, Talamantes reported that medical students who attended a community college during their undergraduate studies were more likely to express interest in family medicine on the MSQ.33At a single medical school, Nayyar found that students who matriculated into medical school immediately after undergraduate graduation had a preference for primary care during their first and second years of medical school.34 Neither study assessed more robust outcomes, such as eventual residency choice.
Some researchers have examined personality traits or personal values, but findings are not consistent enough to draw conclusions. Loosely defined “personal social values” were reported to be an influence on primary care specialty choice in a survey of graduates of a single institution.20 Through personality testing, Ward et al longitudinally studied 229 students at the University of Western Australia between 1984 and 1989 and concluded that students who were “more creative and abstract in their thinking,” and “more conscientious and rule-bound” were less likely to choose primary care.30
Admissions Process
Almost no details of medical school admission processes have been published. For example, Pearson et al speculated that admission criteria might account for practice specialty differences between graduates of the Universities of Newcastle and Sydney without specifying what those differences were.35
We found two admission practices that identify or recruit candidates with a high likelihood of eventually practicing primary care: instituting prematriculation programs that support primary care and identifying students who express interest in primary care at the time of application. There is insufficient evidence to advocate for or against other published admission practices or policies. Furthermore, all research regarding this topic is limited due to the dearth of multi-institutional studies, lack of prospective studies, and reliance on observational data for all outcomes.
Although more robust research in this area is needed, both of these admission practices are practical strategies that medical schools should consider. Prematriculation programs, designed to foster primary care interest among premedical students, could serve as both recruitment programs and experience enhancement opportunities for student participants. Tying such programs to a medical college’s primary care mission or to underserved communities that a medical school serves, and then recruiting students most likely to meet that mission, could be an effective strategy to bolster a medical school’s primary care workforce output.
Similarly, medical schools should consider evaluating applicants’ interest in primary care, and strongly considering this interest in their admissions decisions. Although it has not yet been studied in an admissions context, Kost et al have developed and validated an instrument that predicts students’ entry into family medicine at the time of medical school matriculation.36 In light of our nation’s severe and persistent primary care shortage, the low proportion of US medical schools that favor admitting students with a primary care interest is extremely concerning.18,37
Other admission practices, such as admission subcommittees and targeted whole-institution primary care recruitment, had mixed support and should be studied further. Combining these strategies with exploration of applicant characteristics that predict primary care career interest might bolster their effectiveness. These characteristics include expressed and demonstrated interest in a primary care career prior to matriculation, rural background, older age, and possibly female gender and identification with racial or ethnic minority groups.
Future research needs to deliberately and prospectively examine the outcomes of any of these interventions, in order to develop best practices. Studies are needed to examine more specific details of the admissions processes of institutions that produce higher percentages of primary care physicians. The exact structure and the most effective components of prematriculation programs should also be researched.
The reasons for lack of published admissions processes successful in graduating students who choose primary care specialties are not clear. Institutions may be reluctant to share admissions processes and policies through concern that applicants will manipulate their applications, in order to appear to be a better fit for the institution, or possibly due to fear of legal repercussions.
While it should be noted that some of this literature looked specifically at primary care in rural environments, the findings from these studies were consistent with broader literature on the subject. Additionally, most of the existing literature on this topic is relatively old, and the factors identified may not accurately reflect the current generation of medical students.
Medical schools that want to increase the percentage of their graduates entering primary care should consider the creation of prematriculation programs that attract and prepare highly motivated and talented students with an interest in primary care. Admissions committees should understand which demographic criteria are associated with an increased likelihood of entering primary care, the most important of which is a stated interest in primary care. More robust studies are needed to elucidate the true impact of any admission strategy on the primary care workforce.
Acknowledgments
Funding Statement: This project was partially supported by a grant from the American Board of Family Medicine (ABFM) Foundation (Julie Phillips, PI), and also partially by the Health Resources and Services Administration (HRSA) of the United States Department of Health and Human Services (HHS) under grant number D54HP23297, “Academic Administrative Units” (Christopher Morley, PI). This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by the ABFM, HRSA, HHS, or the US Government.
References
- Phillips J, Weismantel D, Gold K, Schwenk T. How do medical students view the work life of primary care and specialty physicians? Fam Med. 2012;44(1):7-13. doi:10.22454/FamMed.2018.784272
- Phillips RL, Dodoo MS, Green LA, et al. Usual source of care: an important source of variation in health care spending. Health Aff (Millwood). 2009;28(2):567-577. doi:10.1377/hlthaff.28.2.567
- Petterson SM, Liaw WR, Phillips RL Jr, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010-2025. Ann Fam Med. 2012;10(6):503-509. doi:10.1370/afm.1431
- Phillips JP, Wendling AL, Prunuske J, et al. Medical school characteristics, policies, and practices that support primary care specialty choice: a scoping review of five Decades of research. Fam Med. 2022;54(7):542-554.
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Implementing High-Quality Primary Care, Robinson SK, Meisnere M, Phillips Jr RL, McCauley L, editors. Implementing high-quality primary care: rebuilding the foundation of health care. Washington, DC: National Academies Press; May 4, 2021.
- Shi L. The impact of primary care: a focused review. Scientifica (Cairo). 2012;2012:432892. doi:10.6064/2012/432892
- Kelly C, Coutinho AJ, Goldgar C, et al. Collaborating to achieve the optimal family medicine workforce. Fam Med. 2019;51(2):149-158. doi:10.22454/FamMed.2019.926312
- Phillips JP, Wendling A, Bentley A, Marsee R, Morley CP. Trends in US medical school contributions to the family physician workforce: 2018 update From the American Academy of Family Physicians. Fam Med. 2019;51(3):241-250. doi:10.22454/FamMed.2019.395617
- Sutton A, Clowes M, Preston L, Booth A. Meeting the review family: exploring review types and associated information retrieval requirements. Health Info Libr J. 2019;36(3):202-222. doi:10.1111/hir.12276
- Popay J, Roberts H, Sowden A, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. ESRC Methods Programme, 2006. Accessed January 6, 2022. https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf
- Owen JA, Hayden GF, Connors AF Jr. Can medical school admission committee members predict which applicants will choose primary care careers? Acad Med. 2002;77(4):344-349. doi:10.1097/00001888-200204000-00018
- Penn NE, Russell PJ, Simon HJ, et al. Affirmative action at work: a survey of graduates of the University of California, San Diego, Medical School. Am J Public Health. 1986;76(9):1144-1146. doi:10.2105/AJPH.76.9.1144
- Ballejos MP, Shane N, Romero-Leggott V, Sapién RE. Combined baccalaureate/medical degree students match into family medicine residencies more than similar peers: a matched case-control study. Fam Med. 2019;51(10):854-857. doi:10.22454/FamMed.2019.110812
- Kallail KJ. The Scholars in Primary Care Program: an assured admission program. Acad Med. 2001;76(5):499. doi:10.1097/00001888-200105000-00025
- Lupton K, Vercammen-Grandjean C, Forkin J, Wilson E, Grumbach K. Specialty choice and practice location of physician alumni of University of California premedical postbaccalaureate programs. Acad Med. 2012;87(1):115-120. doi:10.1097/ACM.0b013e31823a907f
- Metz AM. Medical school outcomes, primary care specialty choice, and practice in medically underserved areas by physician alumni of MEDPREP, a postbaccalaureate premedical program for underrepresented and disadvantaged students. Teach Learn Med. 2017;29(3):351-359. doi:10.1080/10401334.2016.1275970
- Yutrzenka GJ, Amundson LH. USDSM Alumni Student Scholars Program: successes of the first decade. S D J Med. 2004;57(11):491-498.
- Basco WT Jr, Buchbinder SB, Duggan AK, Wilson MH. Associations between primary care-oriented practices in medical school admission and the practice intentions of matriculants. Acad Med. 1998;73(11):1207-1210. doi:10.1097/00001888-199811000-00021
- Wimsatt LA, Cooke JM, Biggs WS, Heidelbaugh JJ. Institution-specific factors associated with family medicine residency match rates. Teach Learn Med. 2016;28(3):269-278. doi:10.1080/10401334.2016.1159565
- Schieberl JL, Covell RM, Berry C, Anderson J. Factors associated with choosing a primary care career. West J Med. 1996;164(6):492-496.
- Senf JH, Campos-Outcalt D, Kutob R. Family medicine specialty choice and interest in research. Fam Med. 2005;37(4):265-270.
- Senf JH, Campos-Outcalt D, Watkins AJ, Bastacky S, Killian C. A systematic analysis of how medical school characteristics relate to graduates’ choices of primary care specialties. Acad Med. 1997;72(6):524-533. doi:10.1097/00001888-199706000-00020
- Martini CJM, Veloski JJ, Barzansky B, Xu G, Fields SK. Medical school and student characteristics that influence choosing a generalist career. JAMA. 1994;272(9):661-668. doi:10.1001/jama.1994.03520090025014
- Kost A, Cawse-Lucas J, Evans DV, Overstreet F, Andrilla CHA, Dobie S. Medical student participation in family medicine department extracurricular experiences and choosing to become a family physician. Fam Med. 2015;47(10):763-769.
- Campos-Outcalt D, Senf J, Kutob R. A comparison of primary care graduates from schools with increasing production of family physicians to those from schools with decreasing production. Fam Med. 2004;36(4):260-264.
- Xu G, Veloski JJ, Barzansky B, Hojat M, Diamond J, Silenzio VMB. Comparisons among three types of generalist physicians: personal characteristics, medical school experiences, financial aid, and other factors influencing career choice. Adv Health Sci Educ Theory Pract. 1996;1(3):197-207. doi:10.1023/A:1018319914329
- Xu G, Veloski JJ, Politzer RM. Factors influencing learners’ specialty decisions. Acad Med. 1997;72(6):469-470. doi:10.1097/00001888-199706000-00001
- Hull AL, Glover PB, Acheson LS, et al. Medical school applicants’ essays as predictors of primary care career choice. Acad Med. 1996;71(1)(suppl):S37-S39. doi:10.1097/00001888-199601000-00037
- Mitra G, Gowans M, Wright B, Brenneis F, Scott I. Predictors of rural family medicine practice in Canada. Can Fam Physician. 2018;64(8):588-596.
- Ward AM, Kamien M, Lopez DG. Medical career choice and practice location: early factors predicting course completion, career choice, and practice location. Med Ed. 2004;38:239-48.
- Roman SA Jr, McGanney ML. The sophie davis school of biomedical education: the first 20 years of a unique BS-MD program. Acad Med. 1994;69(3):224-230. doi:10.1097/00001888-199403000-00018
- Lawson SR, Hoban JD, Mazmanian PE. Understanding primary care residency choices: a test of selected variables in the Bland-Meurer model. Acad Med. 2004;79(10)(suppl):S36-S39. doi:10.1097/00001888-200410001-00011
- Talamantes E, Hernandez AM, Gonzalez R, et al. Interest in family medicine among US medical students and its association with a community college academic pathway. Fam Med. 2017;49(10):759-764.
- Nayyar N, Saggio G, Plummer M, Jung MK, Kappenberg J. Association of mindfulness with residency preference and curriculum selection in preclinical osteopathic medical students. J Am Osteopath Assoc. 2018;118(9):587-595.
- Pearson SA, Rolfe I, Ringland C, Kay-Lambkin F. A comparison of practice outcomes of graduates from traditional and non-traditional medical schools in Australia. Med Ed. 2002;36:985-91. doi:10.1046/j.1365-2923.2002.01281.x
- Kost A, Cantone RE, Schneider B, Sairenji T, Palmer R. Validation and comparison of a brief instrument vs a single-item screen to predict entry to family medicine at matriculation to medical school. Fam Med. 2018;50(9):672-678. doi:10.22454/FamMed.2018.258795
- Phillips J, Nguyen BM. Curricula that promote primary care: time for action. Med Educ. 2021;55(11):1218-1221. doi:10.1111/medu.14661
- Bowman MA, Haynes RA, Rivo ML, Killian CD, Davis PH. Characteristics of medical students by level of interest in family practice. Fam Med. 1996;28(10):713-719.
- Blumenthal D, Williams M, Pederson L, Okuyemi K. Sixteen-year longitudinal evaluation of a community-oriented primary care curriculum. Educ Health. 1997;10(2):213-220.



There are no comments for this article.