Background and Objectives: Demand for geriatric care is increasing due to aging population. Trends in maintaining certification in geriatrics are unreported.
Our objective was to describe the historic trend of family physicians who certified in geriatric medicine (FPs-GM) since 1988 and to assess differences in practice patterns between FPs-GM and family physicians (FPs).
Methods: We performed a retrospective descriptive study using administrative data collected by the American Board of Family Medicine (ABFM). The study population was family physicians registering to continue their ABFM certification from 2017 to 2019. Medicare public use billing data was linked to ABFM administrative data on certification history. We used univariate analysis for descriptive analysis and logistic regression to identify contributors of recertification in geriatrics.
Results: We identified a total of 3,207 FPs-GM between 1988 and 2019. More than half maintained GM certification since 2009 (57%), with male gender, White race, and urban practice associated with maintaining GM certification; 61% of their patients were older adults. FPs-GM were more likely to be in an academic practice setting with nearly half (53%) also practicing in hospitals or nursing homes. In the adjusted regression model, younger FPs or FPs who treat more older patients were significantly more likely to be recertified in geriatrics whereas other demographics and practice characteristics were not significant.
Conclusions: Most FPs who recently earned GM certification tended to retain certification since the required accredited fellowship started in 1995.
The United States is undergoing a demographic shift with the population over age 65 years projected to reach 73 million by 2030,1 with more than 47% of older adults vulnerable to high rates of frailty, decreased physical function, and complex comorbidities that can co-occur with cognitive impairment. These trends will increase the demand for geriatricians 2, 3 whose comprehensive geriatric assessment and management are associated with lower 30-day readmission rates, 4 improved detection of geriatric syndromes, 5 better quality of life, and more appropriate medication use. 6 Currently, however, only 3.8% of patients 65 years and older are managed by a geriatrician. 4
To develop a structured system for training geriatricians, it is important to understand the practice pattern of geriatricians and needs of older adult patients in primary care. Since 85%-90% of family physicians’ (FPs) patients are adults, of whom 45% are age 65 and older, FPs play an important role in providing accessible care for older adult patients. 7, 8 American Board of Family Medicine (ABFM)-certified FPs can earn a certificate of added qualification (CAQ) in geriatric medicine (GM). From 1988 to 1994, physicians could enter GM certification via a practice pathway but currently, certification is only available to physicians who complete an accredited fellowship. 9 In 2014-2015, about 13.1% of FPs who intended to do a fellowship indicated interest in geriatrics and only 52% of geriatric fellowship training slots were filled in 2021. 10, 11 Despite the need for geriatricians, there is limited evidence about the practice pattern of FPs who certified in GM and long-term trends of CAQ in GM attainment among FPs. Therefore, this study set out to assess trends in GM certification among ABFM-certified FPs. A secondary aim of this study was to examine whether the practice pattern of FPs who certified in GM (FPs-GM) differs from FPs.
Data
We used ABFM administrative data to determine whether an FP was ever certified in GM since 1988 and whether an FP maintained an active GM certificate in 2019. We used practice demographic questionnaires completed by FPs who registered for their Family Medicine Certification examination to continue their certification to examine practice patterns of FPs-GM. 12 We used the Medicare Physician and Other Supplier Public Use File (Physician and Other Supplier PUF) to assess the type of services provided by FPs-GM.
Study Sample
We identified FPs-GM among all FPs who were board certified in 2019 if an initial GM certificate year was found for the physician. Given that board-certified FPs need to pass the GM examination administered by the ABFM every 10 years to maintain GM certificate, FPs were deemed as having an “active GM” certificate in 2019 if their last GM certificate year was 2009 or later, and having an “inactive GM” certificate otherwise. We used this sample to plot the historic trend of GM certification among FPs. We used a subsample of FPs who responded to the practice demographic questionnaires in 2017, 2018, and 2019, and provided direct patient care to examine scope of practice of FPs-GM. We also used this subsample to link with the 2017 (the latest) Medicare Physician and Other Supplier PUF to determine service provision by FP-GMs.
Measures
We counted the number of FPs-GM by year of initial GM certification and calculated the percentage of those with active or inactive GM certification in 2019. We captured practice patterns by practice organization and scope of practice. Practice organization factors included primary practice site (eg, academic health center, hospital, independent practice), secondary practice site (eg, nursing home, hospice, patient home), practice size (eg, solo, small [two to five physicians], medium [6-20 physicians], large [more than 20 physicians]), and practice ownership (eg, zero, partial, or full ownership). We used urban-rural continuum codes (RUCC) to distinguish urban (RUCC=1-3) from rural (RUCC=4-9) practice locations. For practice patterns, we measured scope of practice by whether a physician provided a certain type of care, including behavioral health care, end-of-life care, intensive care, integrative medicine, adult hospital care, delivery, prenatal care, newborn hospital care, pediatric hospital care, and pediatric outpatient care. Additionally, FPs reported the percentage of their patients aged 65 and older and estimated their patient panel size. We also included physicians’ demographic information such as age, gender, and race. We linked each physician to the 2017 Physician and Other Supplier PUF to identify services billed to Medicare. We used Berenson-Eggers Type of Service codes to classify primary care services into office, hospital, nursing home, home visit, emergency room care, and procedures.
Statistical Analysis
We first plotted the number of FPs-GM and the percentage of those with an active GM certificate in 2019 by year of initial GM certification. We presented the numbers for each year but omitted the percentages for 2009 and later years because their GM certification was still active in 2019. We then compared demographic factors, practice organization characteristics, and scope of practice, as well as health care services provided to Medicare beneficiaries of FPs-GM to FPs. We applied χ2 and analyses of variance to determine whether any difference among FPs with active GM certificate, FPs with inactive GM certificate, and FPs was statistically significant. We also conducted logistic regression to identify contributors to GM recertification among FPs. The outcome was dichotomous of being recertified in geriatrics or not and the variables of physicians’ demographics (ie, age, gender and race/ethnicity) and the practice pattern such as practice ownership, patient panel size, primary practice site and other practice site were included. We used age of respondents and percentage of older patients as a continuous variable. We used every year of age and every percentage point to interpret odds ratios. In descriptive analysis, the value of each cell of the tables was calculated using observations with nonmissing data. In regression, observations with missing data on any of the variables were dropped automatically. We conducted all analyses using SAS 9.4 (SAS Institute Inc, Cary, NC). The Institutional Review Board of the American Academy of Family Physicians approved the study.
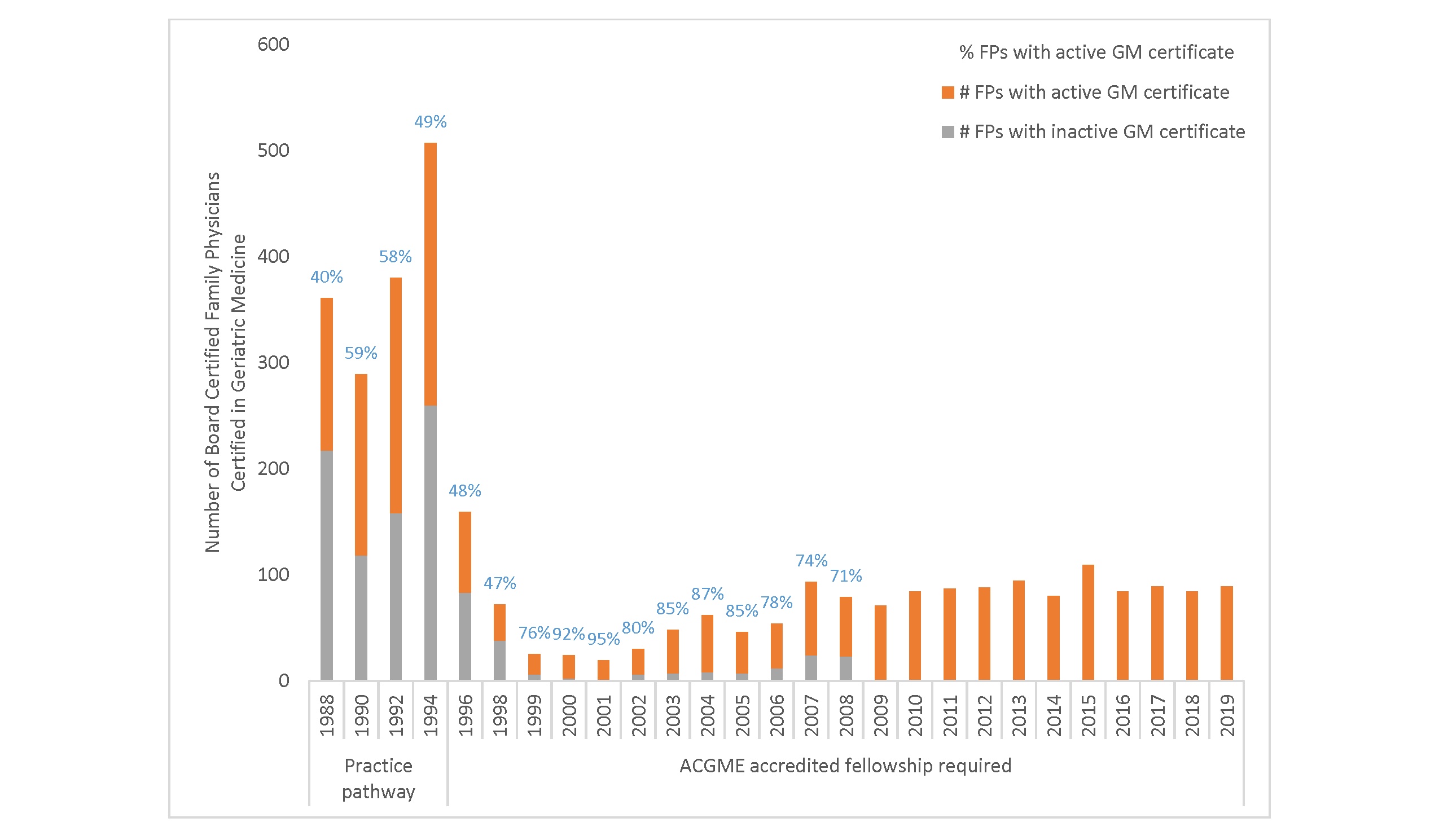
A total of 3,207 board-certified FPs were ever certified in GM from 1988 to 2019 (Figure 1 ). While the practice pathway was open, 51% of all FM-GM’s attained initial certification. However, after the practice pathway closed in 1994, the total number of new FPs-GM decreased. Among those who were certified before 2009 and needed to continue certification prior to 2019 (n=2,248, or 70%), 57% maintained an active GM certificate in 2019. The initial GM certificate for all of the 959 FPs certified in 2009 or later years was still active in 2019, rendering a 100% retention rate. The percentage of FPs with active GM certificate was much higher in the 2000s than in the 1990s.
From 2017 to 2019, 26,699 FPs registered to continue their family medicine certification. In 2019, 625 FPs had active and 296 FPs had inactive GM certificates (Table 1 ). FPs never certified in GM were younger than FPs-GM. Compared to FPs, FPs-GM were more likely to be male, White, and practice in urban rather than rural locations. FPs-GM reported the smallest patient panel size (1,366 vs 2,068 by FPs) but the largest proportion of older patients (61% vs 33% by FPs).
|
Physician Characteristics
|
FPs With Active GM Certificate in 2019
|
FPs With Inactive GM Certificate in 2019
|
FPs Never
Certified in GM
|
P
Value
|
|
N
|
625
|
296
|
25,778
|
|
|
Age, mean (SD)
|
55 (10)
|
63 (7)
|
51 (9)
|
<.01
|
|
Gender
|
|
|
|
|
|
Male
|
62%
|
77%
|
57%
|
<.01
|
|
Female
|
38%
|
23%
|
43%
|
|
Race
|
|
|
|
|
|
White
|
64%
|
84%
|
71%
|
<.01
|
|
Black
|
4%
|
3%
|
7%
|
|
Asian
|
24%
|
8%
|
15%
|
|
Other
|
9%
|
4%
|
7%
|
|
Practice Location
|
|
|
|
|
|
Urban
|
89%
|
82%
|
83%
|
<.01
|
|
Rural
|
11%
|
18%
|
17%
|
|
Patient panel size,** mean (SD)
|
1,366 (1,341)
|
1,706 (1,219)
|
2,068 (1,420)
|
<.01
|
|
% of older patients (aged 65+)
|
61%
|
46%
|
33%
|
<.01
|
|
Primary Practice Site
|
(N=625)
|
(N=296)
|
(N=25,778)
|
|
|
Academic health center
|
17%
|
9%
|
6%
|
<.01
|
|
Hospital owned
|
28%
|
26%
|
28%
|
|
Independently owned
|
21%
|
27%
|
28%
|
|
Managed care/HMO practice
|
7%
|
4%
|
5%
|
|
Federally qualified health center and rural health clinic
|
4%
|
7%
|
7%
|
|
Other
|
22%
|
26%
|
26%
|
|
Secondary Practice Site(s)
|
|
|
|
|
|
No other practice site
|
47%
|
65%
|
66%
|
<.01
|
|
Hospital
|
47%
|
39%
|
48%
|
.25
|
|
Nursing home
|
72%
|
54%
|
30%
|
<.01
|
|
Hospice
|
11%
|
8%
|
4%
|
<.01
|
|
ER
|
2%
|
9%
|
11%
|
.03
|
|
Urgent care
|
5%
|
8%
|
19%
|
<.01
|
|
Patient home
|
34%
|
30%
|
17%
|
<.01
|
|
Another outpatient clinic
|
10%
|
10%
|
12%
|
.16
|
|
Ownership
|
|
|
|
|
|
No ownership, 100% employed
|
71%
|
63%
|
64%
|
<.01
|
|
Partial owner
|
14%
|
11%
|
17%
|
|
Sole owner
|
11%
|
19%
|
14%
|
|
Other (eg, locums)
|
4%
|
7%
|
5%
|
|
Practice Size
|
|
|
|
|
|
Solo
|
11%
|
19%
|
13%
|
<.01
|
|
Small
|
29%
|
32%
|
34%
|
|
Medium
|
27%
|
29%
|
30%
|
|
Large
|
33%
|
20%
|
23%
|
|
Practice Specialty
|
|
|
|
|
|
Family medicine only
|
44%
|
58%
|
51%
|
<.01
|
|
Multiple specialties (not only primary care)
|
27%
|
14%
|
22%
|
|
Primary care specialty mix
|
29%
|
28%
|
27%
|
Not every physician estimated their patient panel size. The number and percentage of physicians with nonmissing panel size was 305 (49%) for FPs with active GM certificate, 137 (46%) for FPs with inactive GM certificate, and 12,083 (47%) for FPs never certified in GM.
While the percentage of FPs with active GM certificate who practiced in hospital-owned practices was the identical to FPs (28%), they were more likely to practice primarily at academic medical centers (17% vs 6%) and less likely to work in independently-owned practices (21% vs 28%; Table 1). Compared to FPs, nearly half (53%) of FPs with active GM certificate practiced at one or more secondary sites, who were also more likely to see patients in nursing homes (72% vs 30%), hospice (11% vs 4%), and patient homes (34% vs 17%). Moreover, FPs with an active GM certificate were less likely to have ownership of the practice and more likely to work in large practices of more than 20 physicians.
FPs with active GM certification reported providing care in all the service areas (Table 2). Compared to FPs, they were more likely to provide palliative care (66% vs 40%), adult inpatient care (45% vs 24%), and care in intensive care unit (14% vs 8%). The percentages of FPs with active GM certificate who reported providing nursery care, prenatal care, pediatric inpatient care, and even delivering babies were similar to FPs. Of the physicians who billed Medicare for services in 2017, FPs with an active GM certificate were more likely to provide inpatient care (44% vs 20% of FPs) and nursing home care (45% vs 9% of FPs) but were less likely to provide office-based care (76% vs 82% of FPs) and procedural services (27% vs 34% of FPs). FPs with an active GM certificate were also more likely to offer home visits (6% vs 1% of FPs).
|
|
FPs With Active GM Certificate in 2019 (%)
|
FPs With Inactive GM Certificate in 2019 (%)
|
FPs Never
Certified in GM (%)
|
P
Value
|
|
By Physician Self-report
|
(N=625)
|
(N=296)
|
(N=25,778)
|
|
|
Palliative care
|
66%
|
40%
|
27%
|
<.01
|
|
Adult inpatient care
|
45%
|
24%
|
24%
|
<.01
|
|
Mental health care
|
29%
|
32%
|
36%
|
<.01
|
|
Pediatric outpatient care
|
25%
|
39%
|
55%
|
<.01
|
|
ICU
|
14%
|
8%
|
9%
|
<.01
|
|
Nursery care
|
11%
|
9%
|
12%
|
.10
|
|
Prenatal care
|
7%
|
5%
|
11%
|
<.01
|
|
Pediatric inpatient care
|
7%
|
8%
|
9%
|
.35
|
|
Delivering babies
|
4%
|
3%
|
6%
|
<.01
|
|
Integrative medicine
|
3%
|
1%
|
5%
|
<.01
|
|
By Services Billed to Medicare
**
|
(N=496)
|
(N=225)
|
(N=19,858)
|
|
|
Office
|
76%
|
85%
|
82%
|
<.01
|
|
Hospital
|
44%
|
23%
|
20%
|
<.01
|
|
Nursing home
|
45%
|
21%
|
9%
|
<.01
|
|
Home visit
|
6%
|
3%
|
1%
|
<.01
|
|
Emergency care
|
2%
|
4%
|
8%
|
<.01
|
|
Procedures
|
27%
|
35%
|
34%
|
<.01
|
In the adjusted logistic regression model, younger FPs or FPs who treat more older patients were significantly more likely to be recertified in GM. Those who had a secondary practice site also had twice the odds of GM recertification. However, any demographics except age and the practice characteristics such as size, ownership, and the primary practice site were not significant factors (Table 3 ).
|
|
Adjusted Odds Ratio (95% CI)
|
|
Age*
|
0.90 (0.87-0.93)
|
|
Sex
|
|
|
Male
|
Ref
|
|
Female
|
0.77 (0.39-1.54)
|
|
Race
|
|
|
White
|
Ref
|
|
Black
|
0.59 (0.14-2.46)
|
|
Asian
|
1.56 (0.64-3.81)
|
|
Others
|
1.11 (0.31-3.93)
|
|
Practice Location
|
|
|
Urban
|
Ref
|
|
Rural
|
0.62 (0.31-1.24)
|
|
% of Older Patients *
|
1.03 (1.01-1.04)
|
|
Patient Panel Size
|
1.00 (1.00-1.00)
|
|
Ownership
|
|
|
No ownership
|
Ref
|
|
Have an ownership
|
0.93 (0.34-2.53)
|
|
Practice Size
|
|
|
Large
|
Ref
|
|
Solo
|
0.42 (0.16-1.15)
|
|
Small
|
0.84 (0.40-1.79)
|
|
Medium
|
0.71 (0.35-1.45)
|
|
Practice Specialty
|
|
|
Multispecialty
|
Ref
|
|
Family medicine only
|
1.12 (0.64-1.97)
|
|
Primary Practice Site
|
|
|
Independence practice
|
Ref
|
|
Academic health center
|
0.61 (0.19-2.02)
|
|
Hospital owned
|
1.41 (0.42-4.71)
|
|
Managed care
|
0.72 (0.26-1.99)
|
|
Government health care
|
1.19 (0.33-4.27)
|
|
Others
|
1.84 (0.51-6.65)
|
|
Secondary Practice Site*
|
|
|
No
|
Ref
|
|
Yes
|
2.26 (1.35-3.79)
|
This study shows that the retention in FM certification is higher in those who certified after the practice pathway closed, and the number of FPs with a new GM certificate is declining. We additionally report on the clinical activities of FPs-GMs who were more likely to work at large hospitals and nursing homes in urban areas that have more resources. FP-GMs provide not only geriatric care for older adults but also core primary care services.
GM certificate retention rate among FPs has remained higher than 75% since 1999, roughly the closing of the practice pathway. It is consistent with the findings of about 90% of geriatricians who chose to recertify or plan to renew certification in geriatric medicine. 13, 14 This difference in retention between practice pathway physicians and fellowship-trained physicians may result from aging physicians who first took the exam and who may have retired since then. In addition, the difference may point to the uncertainty around the need for the credential to work in certain settings in early days of geriatrics certification. These physicians may not have been as committed to practicing geriatric medicine as ones who complete another year of training. The low numbers of FPs entering GM certification raises concerns of a deficit of geriatricians across all health care settings. According to the Health Resources and Services Administration’s 2017 report, National and Regional Projections of Supply and Demand for Geriatricians: 2013-2025,” the projected deficit of geriatricians will be 26,980 by 2025. 3 This will be impossible to meet with only half of the 400 geriatric fellowship positions offered annually filling, 11 despite high job satisfaction and positive career impacts of GM certification. 13, 14, 15 Specifically, geriatricians are one of the top-two subspecialties in terms of job satisfaction. 16 However, according to the American Board of Medical Specialties, the 10-year total number of certificates issued for FP-GM and internists who certified in geriatric medicine (IM-GM) between 2010 and 2019 was 909 and 1,729, respectively. 17 In addition, in 2016, the total number of active FM-osteopathic-GM and IM-osteopathic-GM was 300 and 50, respectively. 18 Demand will only increase as the number of Medicare beneficiaries has steadily increased. 19 A key reason of this shortage is lower financial reimbursement for geriatricians. 15 As they manage more complex and frail older patients, geriatricians spend more time with older adult patients. 4, 20 Despite higher satisfaction, there are limited financial benefits for geriatricians. For instance, while FPs are paid more by $6,000 than FPs-GM reported by physician report 2021, this discrepancy has persisted for at least 10 years. 21, 22 There is no explicit incentive system to support geriatricians once they are in practice. Although Medicare supports the costs of approved graduate medical education (GME) programs (ie, fellowship training), it covers only a 1-year fellowship caring for a limited number of beneficiaries. 23 This gap of supply and demand, with limited financial benefits, may deteriorate access to geriatric care and increase physician burnout. It indicates that older adult patients may not receive better patient-centered, well-coordinated care.
FPs with GM certification were more likely to be employed in a large academic center or hospital-owned facilities. This career path was consistent with previous studies. A significant number of GM fellows chose to pursue academic careers. 14, 21 Moreover, the majority of FP-GMs tended to work in nursing homes as a secondary practice site, which supports our finding that approximately half of FP-GMs bill Medicare geriatric care services. According to Lam and colleagues, geriatricians who underwent postgraduate geriatric training felt more confident in understanding and diagnosing complex geriatric conditions. 24 Furthermore, they were more likely to show better understanding in polypharmacy and managing geriatric syndromes regardless of number of visits and patients’ characteristics compared to primary care physicians. 25 Some US studies also found that many FP-GMs who performed home visits for older adult patients or who received palliative care trainings during the fellowship program reported achievement in competency and positive attitude about the value of the training. 26, 27 Our findings not only corroborate existing evidence but also indicate that the added qualifications in GM do translate into FPs providing geriatric care with greater focus and depth, a desired outcome of GM certification.
Most FPs-GM are practicing in urban areas and in larger health care systems whereas it was not a significant factor for recertification. This disproportionate distribution has been observed in the entire geriatric workforce for years even though FPs are more evenly distributed. 28 This rural/urban disparity becomes more critical as people in rural areas tend to be older and need more health care resources. In 2016, 17.5% of residents in rural areas were older adults, and this percentage is expected to increase. 29 Disproportionate distribution of geriatricians may exacerbate health disparities in rural areas since these older adults have limited access to resources focused on healthy lifestyle and social functioning. 30 In addition, despite extended benefits of telehealth such as better access to geriatric specialty care for rural areas amid COVID-19, geriatricians practicing in rural areas still struggle with limited training and educational resources for technology. 31 Furthermore, more accessible resources for geriatrics training and an integrated health care system tailored to older patients such as Age-Friendly Health Systems (AFHS) can address disproportionate distribution of geriatricians in urban areas. Callahan and colleagues suggested web-based geriatrics education modules and reverse minifellowship to allow FPs in rural areas to have access to geriatrics training resources and increase attention to certification in geriatrics. 32 In addition, AFHS is an innovative way of leveraging the existing geriatrics workforce through implementing the four essentials including what matters to older patients, medication, mobility and mentation in the hospital setting. 33 These examples may attract younger FPs and geriatricians to practice in rural areas. Plus financial incentives also need to be considered. Currently, Medicare is the only government organization sponsoring GME programs, 26 however, there is no additional direct financial aid from the employer (ie, hospitals). As reimbursement for geriatric care is relatively lower, financial aid for early-career geriatricians may have a direct impact on attracting FPs and mitigating financial burden for those who want to pursue extra trainings.
This study has some limitations. First, as administrative data were used, we were not able to identify reasons for renewal of GM-CAQ by FPs and reasons of declining trend of GM-CAQ. Also, although most geriatric care services are delivered in a coordinated care form, our study captured only practice locations in which FP-GMs delivered the care without a form of delivery of care. Future studies need to examine the impact of geriatric CAQ on clinical practice using primary survey data or qualitative data from FPs. Also, future studies utilizing data on practice patterns are needed to identify reasons for the declining trend of recertifications and new certifications. Next, our study focused only on FP-GMs. According to the American Osteopathic Association, in 2017, there were 310 total active FP-GMs whereas there were only 59 total active certifications in internal medicine. 18 Thus our finding may not apply to the entire geriatrician workforce.
Most FP-GMs were more likely to practice at academic medical centers and long-term care centers that have more resources. Most FPs who recently earned their geriatric CAQ tend to retain certification, whereas the number of new GM-CAQ is declined. To respond to the emerging demand from aging population, well-trained geriatricians who are knowledgeable in complex conditions of older adult patients and who communicate effectively with patients and caregivers are critical. Therefore, better financial incentives will be needed for current FP-GMs and potential FPs who have interests in GM-CAQ.
Ara Jo, PhD, led the entire research process and composed the manuscript. Mingling Dai, PhD, performed data analysis and wrote the manuscript. Lars Peterson, MD, PhD, and Arch G. Mainous III, PhD, reviewed and edited the manuscript.
This study was presented in November 2020 at the North American Primary Care Research Group (NAPCRG) Annual Meeting (virtual).
References
-
-
Sanford AM, Morley JE, Berg-Weger M, et al. High prevalence of geriatric syndromes in older adults. PLoS One. 2020;15(6):e0233857. doi:10.1371/journal.pone.0233857
-
-
Sinvani L, Carney M, Kozikowski A, et al. The role of geriatrician-hospitalists in the care of older adults: A retrospective cohort study. Arch Gerontol Geriatr
. 2018;77:31-37. doi:10.1016/j.archger.2018.03.006
-
Mason MC, Crees AL, Dean MR, Bashir N. Establishing a proactive geriatrician led comprehensive geriatric assessment in older emergency surgery patients: outcomes of a pilot study. Int J Clin Pract. 2018;72(5):e13096. doi:10.1111/ijcp.13096
-
Romskaug R, Skovlund E, Straand J, et al. Effect of clinical geriatric assessments and collaborative medication reviews by geriatrician and family physician for improving health-related quality of life in home-dwelling older patients receiving polypharmacy: a cluster randomized clinical trial. JAMA Intern Med
. 2020;180(2):181-189. doi:10.1001/jamainternmed.2019.5096
-
-
Cherry D, Lucas C, Decker SL. Population aging and the use of office-based physician services. NCHS Data Brief. 2010;(41):1-8.
-
Warshaw GA, Bragg EJ. The training of geriatricians in the United States: three decades of progress. J Am Geriatr Soc
. 2003;51(7)(suppl):S338-S345. doi:10.1046/j.1365-2389.2003.51345.x
-
Sairenji T, Dai M, Eden AR, Peterson LE, Mainous AG III. Fellowship or further training for family medicine residents. Fam Med. 2017;49(8):618-621.
-
-
Peterson LE, Fang B, Phillips RL Jr, Avant R, Puffer JC. The American Board of Family Medicine’s data collection method for tracking their specialty. J Am Board Fam Med
. 2019;32(1):89-95. doi:10.3122/jabfm.2019.01.180138
-
Shah U, Aung M, Chan S, Wolf-Klein GP. Do geriatricians stay in geriatrics? Gerontol Geriatr Educ
. 2006;27(1):57-65. doi:10.1300/J021v27n01_04
-
Cao Q, Lee TJ, Hayes SM, et al. Are geriatric medicine fellows prepared for the important skills of hospice and palliative care? Am J Hosp Palliat Care
. 2015;32(3):322-328. doi:10.1177/1049909113517050
-
-
Leigh JP, Tancredi DJ, Kravitz RL. Physician career satisfaction within specialties. BMC Health Serv Res
. 2009;9(1):166. doi:10.1186/1472-6963-9-166
-
-
Wieting JM, Williams DG, Kelly KA, Morales-Egizi L. Appendix 2: American Osteopathic Association Specialty Board Certification. J Am Osteopath Assoc. 2018;118(4):275-279.
-
-
Peterson LE, Cochrane A, Bazemore AW, Petterson S. Reported practice patterns among family physicians with a geriatrics certificate of added qualifications. J Am Board Fam Med
. 2015;28(3):314-315. doi:10.3122/jabfm.2015.03.140333
-
Golden AG, Xu P, Wan TT, Issenberg SB. Estimating the net career income of a geriatrician and a nurse practitioner: still want to be a doctor. South Med J
. 2016;109(7):409-414. doi:10.14423/SMJ.0000000000000484
-
-
-
Lam TP, Chow RW, Lam KF, Lennox IM, Chan FH, Tsoi SL. Evaluation of the learning outcomes of a year-long postgraduate training course in community geriatrics for primary care doctors. Arch Gerontol Geriatr
. 2011;52(3):350-356. doi:10.1016/j.archger.2010.05.019
-
Phelan EA, Genshaft S, Williams B, LoGerfo JP, Wagner EH. A comparison of how generalists and fellowship-trained geriatricians provide “geriatric” care. J Am Geriatr Soc
. 2008;56(10):1807-1811. doi:10.1111/j.1532-5415.2008.01942.x
-
Bryce C, Kam-Magruder J, Jackson J, Ledford CJW, Unwin BK. Palliative care education in the family medicine clerkship: a CERA study. PRiMER Peer-Rev Rep Med Educ Res
. 2018;2(20):20. doi:10.22454/PRiMER.2018.457651
-
Sairenji T, Wilson SA, D’Amico F, Peterson LE. Training family medicine residents to perform home visits: a CERA survey. J Grad Med Educ
. 2017;9(1):90-96. doi:10.4300/JGME-D-16-00249.1
-
Peterson LE, Bazemore A, Bragg EJ, Xierali I, Warshaw GA. Rural-urban distribution of the U.S. Geriatrics physician workforce. J Am Geriatr Soc
. 2011;59(4):699-703. doi:10.1111/j.1532-5415.2011.03335.x
-
-
Baernholdt M, Yan G, Hinton I, Rose K, Mattos M. Quality of life in rural and urban adults 65 years and older: findings from the National Health and Nutrition Examination survey. J Rural Health
. 2012;28(4):339-347. doi:10.1111/j.1748-0361.2011.00403.x
-
Nearing KA, Lum HD, Dang S, et al. National Geriatric Network rapidly addresses trainee telehealth beeds in response to COVID-19. J Am Geriatr Soc. 2020;68(9):1907-1912. doi:10.1111/jgs.16704
-
Callahan KE, Tumosa N, Leipzig RM. Big ‘G’and little ’g′ geriatrics education for physicians. J Am Geriatr Soc
. 2017;65(10):2313-2317. doi:10.1111/jgs.14996
-
Fulmer T, Mate KS, Berman A. The age-friendly health system imperative. J Am Geriatr Soc
. 2018;66(1):22-24. doi:10.1111/jgs.15076



There are no comments for this article.