Background and Objectives: Obstetric care is a core element in family medicine education. New interns typically learn the sterile cervical exam on the job by examining women in labor. This can be uncomfortable for patients and may increase the risk of infection. Simulated training could minimize these challenges, but manufactured models are expensive and not widely available in residency programs. We sought to evaluate a simple, homemade sewn model using stretchy fabric and pipe cleaners that could improve teaching and acquisition of cervical examination skills and common obstetrical procedures.
Methods: We used the model to teach cervical examination skills to students and new interns and assessed participant satisfaction. We evaluated examination accuracy by grading practice exams on the model before and after a workshop teaching obstetrical procedures including the sterile vaginal exam. We calculated satisfaction using summary statistics. We evaluated pre- and postscores for exam accuracy using paired t tests.
Results: Interns demonstrated a significant improvement in cervical exam skills using the model, and participants reported very high satisfaction with the workshop utilizing the model.
Conclusions: We developed a simple, low-cost cervical exam model that was shown to be well-regarded by trainees and could be duplicated by other residency programs. This approach provides a unique and accessible way to offer hands-on simulation during obstetrical training. The model may improve trainees’ understanding of the procedures which would lead to better experiences for obstetrical patients.
Obstetric care, including accurate assessment of cervical dilation, is an essential part of family medicine training. Obstetrical deliveries by family medicine residents have dropped in the last decade, in part due to reductions in required obstetrical training during residency. Clinical simulation opportunities offer an important tool to fill a training gap.
New interns typically learn the sterile cervical exam (SVE) on the job by examining women in labor, but it is difficult to learn and teach as the internal exam is not visible. Early training requires having attendings repeat the SVE, which may increase discomfort for patients, and can potentially put a patient at higher infection risk.1 To provide simulation-based training of the SVE and internal obstetrical procedures, we developed a small, portable, and low-cost cervical model sewn with easily available materials and tested it for exam reproducibility and acceptability among trainees.
Model Development
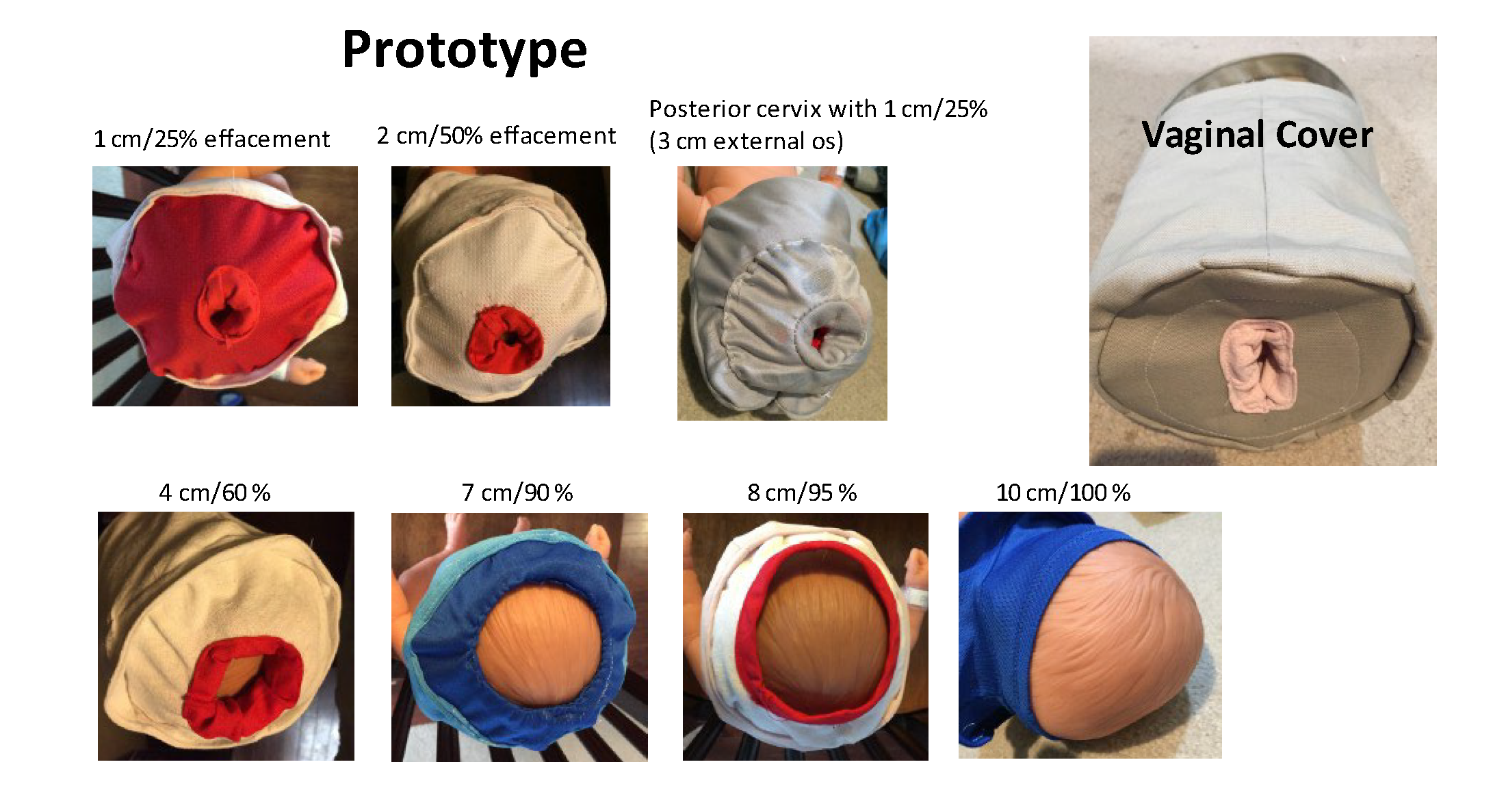
Author S.H.L. created 14 beanie hats with a top opening, using silky, thin, and stretchy technical shirt fabric to mimic different dilations, thicknesses, and cervical positions (Figure 1). This hat fits over a newborn doll head to simulate the cervix. Cervical thickness was created using pipe cleaners, yarn, and foam pads sewn inside shirt material. A removable cover—a bucket made of canvas and foam—was developed with an opening to simulate the vaginal introitus. Using this cover, trainees can practice a blind exam; without it, they can be observed.
Evaluation
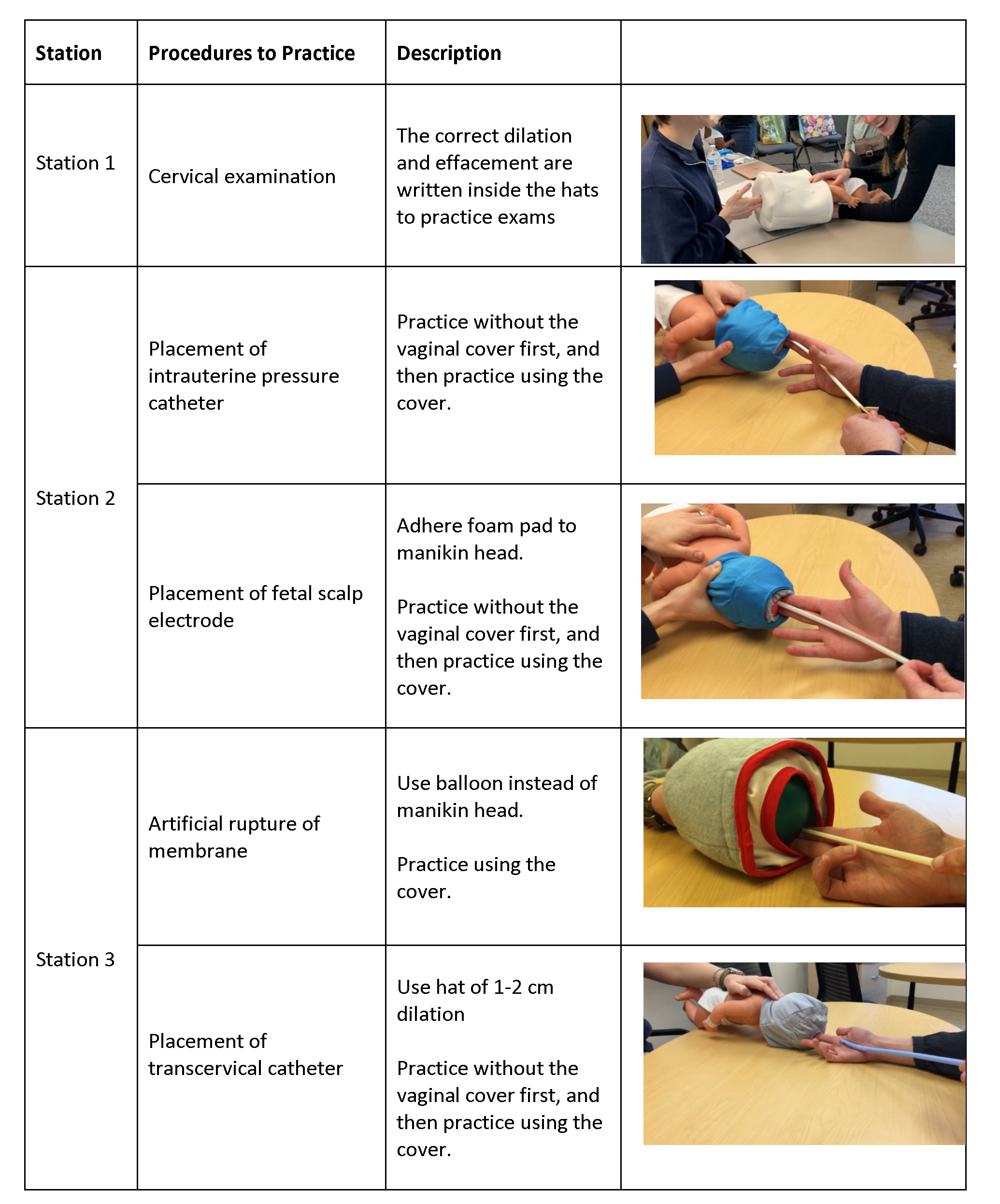
We conducted a skills workshop with new family medicine interns in their first month of residency (2019) and again with new residents in 2021. The workshop consisted of three stations to teach the SVE and related obstetrical procedures described in Figure 2. Residents participating in the research completed a brief paper survey using a random study ID to link pre- and postworkshop SVE testing. The institutional review board at the University of Michigan reviewed and deemed the study exempt from ongoing review.
Before the workshop, participating residents completed 10 consecutive SVEs using the model hidden by the vaginal cover and reported dilation and effacement of each cervix. Accuracy was assessed by comparing these scores to the actual measurement. Dilation was accepted as correct if within 1 cm and effacement as correct if within 25% (4 cm thickness is 0% effacement). We scored 1 point for each correct answer. Postworkshop, residents completed 10 additional practice SVEs using the model. To ensure the model accurately represented real-world practice, we asked eight attending physicians who practice inpatient obstetrics to test the model as well.
We developed a 4-item Likert-style survey about trainee experience and satisfaction with the workshop and use of the model; residents completed this survey after the workshop. We conducted a similar workshop in 2021 with fourth-year medical students and used this survey but not the pre- and posttesting of exam accuracy.
Data Analysis
We evaluated scores from pre- and posttesting using paired t tests. Due to mild skewness, we performed sensitivity analyses with P values generated using a bootstrap method that is robust to departures from normality. We created individual change scores and tested association with gender and prior SVE experience via linear regression analysis. We carried out linear mixed regression analysis with a random subject intercept accounting for within-subject clustering, further adjusting for gender and prior SVE experience. We compared the posttest resident scores with attending physician scores using a two-sample t test. We analyzed satisfaction questions with summary statistics for mean and standard deviation.
A total of 26 residents and 12 medical students completed the training. All 26 residents and 8 of 12 medical students completed the evaluation measures. Table 1 shows demographics and prior training. Residents represented 20 US medical schools and had limited SVE experience—typically fewer than five prior exams. We found significant improvements in accuracy before and after the training course (Figure 3). Using our linear mixed-model analysis with a random subject intercept, adjusting for gender and prior SVE experience, pre/post differences for both dilation and effacement remained significant (P<.001). Differences were not significantly associated with gender or prior SVEs. There were no significant differences in scores by attending physicians and postworkshop residents.
On the satisfaction survey (Table 2), most participants reported that training with the model improved their understanding of different obstetrical procedures while increasing skills and comfort. All strongly agreed that they would recommend the training to others.
|
|
|
Residents (n=26)
|
Medical Students (n=8)
|
|
Gender
|
|
|
|
|
Female
|
13
|
|
|
Male
|
13
|
|
|
Number of SVE on patients practiced during medical school
|
|
|
|
|
0
|
13
|
3
|
|
1-4
|
7
|
5
|
|
5-10
|
3
|
0
|
|
11 or more
|
3
|
0
|
|
Education about cervical examination during school
|
|
|
|
|
Yes
|
10
|
1
|
|
No
|
16
|
7
|
|
Method used for cervical exam education, if any
|
|
|
|
|
Patient
|
4
|
0
|
|
Cloth model
|
2
|
1
|
|
Plastic board
|
1
|
0
|
|
Unsure
|
3
|
0
|
|
Survey Item
|
Average (Standard Deviation)
|
|
Residents (n=26)
|
Medical Students (n=8)
|
|
The educational session for cervical exam and procedures through cervix using the model improved my understanding of the procedures.
|
|
|
|
|
Strongly disagree (1)
|
Somewhat disagree (2)
|
Somewhat agree (3)
|
Strongly agree (4)
|
3.96 (+/- 0.20)
|
3.88 (+/- 0.35)
|
|
The educational sessions for cervical exam and procedures through cervix using the model helped me improve my skills.
|
|
|
|
|
Strongly disagree (1)
|
Somewhat disagree (2)
|
Somewhat agree (3)
|
Strongly agree (4)
|
3.92 (+/- 0.27)
|
3.75 (+/- 0.46)
|
|
The educational sessions for cervical exam and procedures through cervix using the model improved my comfort level towards these procedures.
|
|
|
|
|
Strongly disagree (1)
|
Somewhat disagree (2)
|
Somewhat agree (3)
|
Strongly agree (4)
|
3.80 (+/- 0.40)
|
3.75 (+/-0.46)
|
|
I would recommend this training to my peers.
|
|
|
|
|
Strongly disagree (1)
|
Somewhat disagree (2)
|
Somewhat agree (3)
|
Strongly agree (4)
|
4.00 (+/- 0.00)
|
3.88 (+/-0.35)
|
This work demonstrates the efficacy of using a simple cervical simulation model to teach cervical examination and common procedures. Most trainees in our study had limited prior SVE practice as medical students often report being excluded from routine gynecological examinations during their Ob-Gyn clerkship due to patient requests.2
Simulation training in obstetrics is widely accepted, and use of silicone-based models to improve SVE accuracy has been reported previously.3, 4 While such models are commercially available, they are expensive, and silicone tears with repeated use. Less-costly rigid models improve SVE accuracy but are not as realistic. 5, 6 The most unique attributes of this model are that it allows direct visualization and can be used to teach procedures.
Study limitations of this pilot work included small sample size, lack of a control group, and use at a single institution. Testing the effectiveness of this simulation training on subsequent real-world exams was beyond the scope of our study but is worth further exploration. As dilation and effacement on the model can be physically measured, it serves as a training tool that may be more accurate than comparison to subjective exams on patients by other clinicians. Like other models described in the literature, our model did not always accurately reproduce fetal station.4, 5
We noted significant improvements in exam accuracy after training. Universally high satisfaction ratings suggest the model has good potential as a training tool. We plan to create a reproducible, professional prototype and patterns to make widely available to other residency programs and encourage additional research on the impact of this simulation model on trainee performance on service.
Acknowledgments
Conflict Disclosure: The model was developed by author S.H.L. All other authors have no other conflicts to disclose.
Presentations: Preliminary data from this study were presented as:
Little SH, Medaugh CM, Heinrich L. A novel portable model for teaching cervical examination skills. STFM Annual SpringConference (virtual); May 2021.
References
1. Gluck O, Mizrachi Y, Ganer Herman H, Bar J, Kovo M, Weiner E. The correlation between the number of vaginal examinations during active labor and febrile morbidity, a retrospective cohort study. BMC Pregnancy Childbirth. 2020;20(1):246. doi:10.1186/s12884-020-02925-9
2. Jiang X, Altomare C, Egan JF, Tocco DB, Schnatz PF. The ObGyn clerkship: are students denied the opportunity to provide patient care and what is the role of gender? Conn Med. 2012;76(4):231-236.
4. Lin W, Song Y. Effectiveness of different numbers of simulation training models on medical students’ cervical examination performance. Int J Gynaecol Obstet. 2018;141(2):255-260. doi:10.1002/ijgo.12404
5. Nitsche JF, Fino NF, Palomo JM, Perdomo AP, Brost BC. Effectiveness of a labor cervical exam model in family medicine and OB-GYN residents. Fam Med. 2017;49(5):384-387.
6. Swaminathan G, Parulekar SV. Does Simulation Training Improve the Accuracy of Vaginal Assessment of Labour Progress? Cureus. 2021;13(7):e16089. doi:10.7759/cureus.16089




There are no comments for this article.