Background and Objectives: Workforce diversity is associated with improved health outcomes. Currently, primary care physicians who are underrepresented in medicine (URiM) disproportionately work in underserved areas. Increasingly, URiM faculty describe experiencing imposter syndrome (IS), including a sense of not belonging in their work environment and a lack of recognition. Studies of IS among family medicine faculty are not prevalent nor are the factors most associated with IS among URiMs and non-URiMs. The objectives of our study were to (1) determine prevalence of IS among URiM faculty compared to non-URiM faculty; (2) determine factors associated with IS among both URiM and non-URiM faculty.
Methods: Four hundred thirty participants completed anonymous, electronic surveys. We measured IS using a 20-item validated scale.
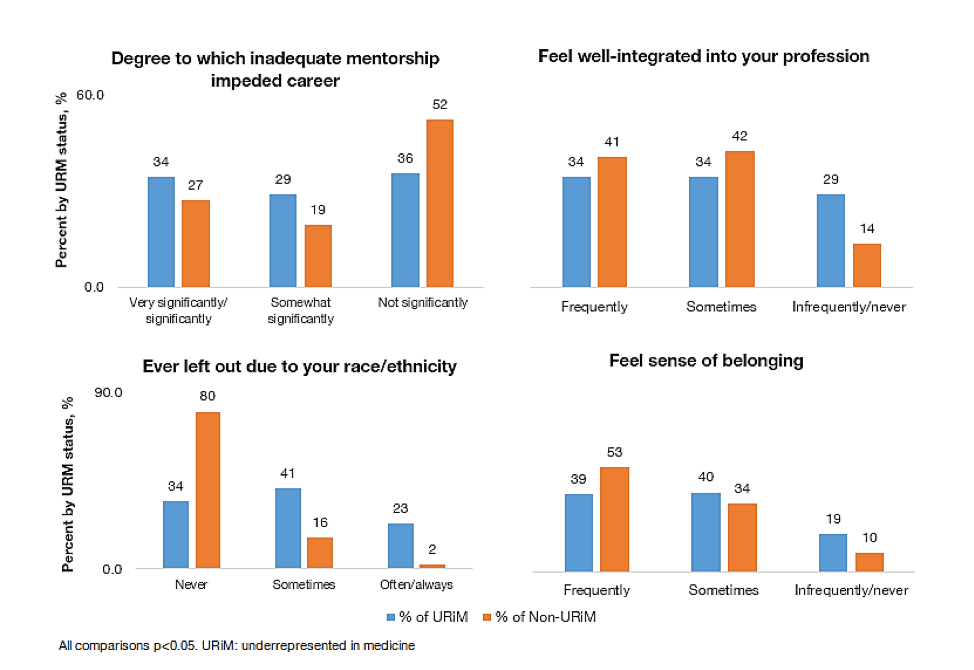
Results: Among all respondents, 43% reported frequent/intense IS. URiMs were not more likely than non-URiMs to report IS. Factors independently associated with IS for both URiM and non-URiM respondents include inadequate mentorship (P<.05) and poor professional belonging (P<.05). However, inadequate mentorship, low professional integration and belonging, and racial/ethnic discrimination-based exclusion from professional opportunities (all P<.05) were more prevalent among URiMs than non-URiMs.
Conclusions: While URiMs are not more likely than non-URiMS to experience frequent/intense IS, they are more likely to report racial/ethnic discrimination, inadequate mentorship, and low professional integration and belonging. These factors are associated with IS and may be reflective of how institutionalized racism impedes mentorship and optimal professional integration, which may be internalized and perceived as IS among URiM faculty. Yet, URiM career success in academic medicine is crucial for achieving health equity.
Diversity in the medical workforce is associated with improved health outcomes, especially for the most disadvantaged communities. 1 Physicians who are underrepresented in medicine (URiM) are more likely than non-URiM physicians to work in medically underserved areas, especially primary care physicians. 1-3 Yet, URiMs often describe a sense of not belonging in their current work environment, 4, 5 a lack of recognition of their own successes, and a lack of attribution of their achievements to their own intrinsic worth as opposed to just luck or happenstance. These experiences are consistent with elements of the imposter syndrome 6 (IS) and are likely to negatively influence URiM recruitment, retention, and career persistence.
The term Impostor Phenomenon (IP) was coined in the late 1970s by two clinical psychologists, Pauline Rose Clance and Suzanne Imes, who used it to describe a series of traits and behaviors of high-achieving, primarily White, middle/upper-middle class women. 6 They described highly successful professional women, many with high scores on standardized tests, advanced degrees, significant academic achievements, and positions of authority, who, despite their accomplishments, reported feelings of fraudulence about their successes and a lack of capacity to attribute their successes to their own intrinsic abilities. 6 Specific familial characteristics thought to be potential root causes of IP included families that persistently and unreasonably valued achievement. As such, when IP was designated, the concept itself was originally thought to apply mostly to high-achieving White women with characteristic family dynamics. Since then, however, the phenomenon has become known by the term imposter syndrome (IS) and is widely applied across racial/ethnic, gender, and class-based experiences as well as frequently referenced among many who feel they do not belong in their professional space. 7
Extant literature has suggested that IS generally is more common among females than males and is notably prevalent among medical students and other medical professionals. 8-10 One review reported rates of IS ranging from 22% to 60% among physicians and physicians in training. 11 Research findings on the prevalence of IS and associated factors among racial/ethnic minorities are inconsistent. For example, a recent study found no difference in the prevalence of IS by race/ethnicity among a group of nursing students. 12 In contrast, a systematic review of the prevalence and predictors of IS showed that symptoms of IS were particularly high among ethnic minority groups. 13 Yet, another scoping review of medical students found no association between IS and minority status. 11, 14 Factors that have been associated with IS for racial/ethnic minorities include microaggressions and experiences of racial/ethnic discrimination. Such experiences were found to be significantly predictive of increased feelings of otherness and intellectual ineptitude. 15, 16 Additionally, Cokley et al 17 and McClain et al 18 found that for racial/ethnic minorities, a combination of stressors—including racial discrimination, microaggressions, and fears of not belonging—correlated with IS. In 2017, Cokley et al. 19 also reported that perceived discrimination had a stronger impact on feelings of IS among African American and Latino/a/x students compared to their Asian American peers. More investigation is needed to understand the prevalence and potential factors associated with IS among URiMs and non-URiMs in academic medicine.
Since the 1970s, the number of URiMs entering and remaining in the medical workforce has been stagnant. 20 Even fewer URiMs pursue academic medicine, and when they do, they often are disproportionately overextended with clinical care responsibilities, diversity efforts, and other forms of volunteer service to their institutions compared to non-URiM faculty.4, 21 These institutional activities are reflective of the minority tax often experienced by URiMs in academic medicine, which can deter participation in activities such as mentorship and scholarly work necessary to achieve promotion. 5, 21 Compounding the effect of the minority tax on the promotion and tenure process, URiMs often are passed over for leadership positions as a result of structural and systemic mechanisms of inequity, including racism and sexism. 4, 5 URiMs often are surprised when White faculty evaluate their level of accomplishment, devaluing their work, and in some cases, blatantly or subtly racially discriminating despite the individual’s high academic achievement. 4 These mechanisms of micro- and macroaggression may take a physical and psychological toll. 22 Therefore, not surprisingly, many URiMs perceive (1) isolation in their academic environments 4, 5; (2) little acknowledgment of their successes, and (3) lack of ascription of their achievements to their own intrinsic worth. These perceptions are associated with IS and contribute to anxiety, depression, low self-confidence, 23, 24 and subsequent adverse effects on job well‐being, satisfaction, and performance. 25
This study furthers the research about IS by examining the prevalence of IS and related factors among academic family medicine (FM) faculty. The study aimed to (1) determine the prevalence of IS among URiM and non-URiM FM faculty and teachers; and (2) identify the factors associated with IS among both URiM and non-URiM faculty and teachers.
Data Collection and Participants
For this cross-sectional study, we e-mailed an anonymous web-based survey to a convenience sample of participants who identified as family medicine faculty and/or teachers across the United States from September through November 2020. We also extended an invitation to participate in the study to physicians and faculty/teachers from various disciplines. We recruited participants via national organization listservs (eg, from the Society of Teachers of Family Medicine and the North American Primary Care Research Group) as well as by survey dissemination to known academic contacts (also family medicine faculty and/or teachers) of the principal investigator. The Institutional Review Board of the American Academy of Family Physicians reviewed and granted exemption to the study.
Dependent and Independent Variables and Instruments
We collected demographic data, including age, race/ethnicity, gender identity, academic degree, faculty appointment, years since training, and practice region. We used the Clance Imposter Phenomenon Scale (CIPS) to measure IS, the outcome variable. CIPS is a 20-item validated instrument in which scores range from 20 through 100 and correspond to four categories of IS: low (score≤40), moderate (41-60), frequent (61-80), or intense (>80). CIPS items measure the presence of cognitions and effects associated with IS, including feelings related to fear of (a) evaluation, (b) not being able to repeat successes, and (c) being less capable than others (see Appendix for complete list of questions). 26
Other important independent factors potentially related to career experiences included perceived professional discrimination based on gender, race/ethnicity, or class; mentorship; and professional integration. We measured discrimination experiences using the Perceived Gender, Race/Ethnicity, and Class Bias Scale, a 6-item scale measuring perceived structural and systemic bias and discrimination in professional advancement. 4 A sample question was, “In your professional career, have you ever been left out of opportunities for professional advancement based on your race/ethnicity?” Response options included never, sometimes, often, and always. We assessed mentorship experiences using several items from the Robert Wood Johnson Foundation’s Mentorship Relationship Functions Scale, which assesses the perceived performance of a respondent’s faculty mentor. We focused on the following item: “Do you believe that inadequate mentoring has impeded your career growth?” Response options ranged from 1 (very significantly) to 5 (not at all significantly). We measured perceptions of professional integration by asking respondents whether they perceived themselves well-integrated into their profession and perceived a sense of belonging in their positions. Response options ranged from 1 (frequently) to 4 (never). 27
Analysis
We classified participants as URiM based on the Association of American Medical Colleges’ definition of underrepresented in medicine: “racial and ethnic populations that are underrepresented in the medical profession relative to their numbers in the general population.” 28 The following groups are underrepresented in medicine compared to their representation in the general US population: Black/African American, Hispanic/Latino/a/x, Native American (American Indian, Alaska Natives), and Native Hawaiian/other Pacific Islanders. 29, 30 We used Fisher’s exact tests to compare demographic and career experience variables between URiMs and non-URiMs. We compared the percentage of respondents with IS scores categorized as frequent or intense across respondents’ career experiences. We used unadjusted and adjusted Firth logistic regression models to compare covariate odds of frequent/intense IS vs low/moderate IS. Regression models included dummy variables for missing covariate values. The variables age, faculty appointment type, primary degree, and years since training each strongly correlated with one another. We compared adjusted model fit characteristics (eg, Akaike information criterion) and found years since training to be the variable to best fit the data in terms of explaining differences between IS categories. We performed all analyses using SAS software version 9.4. 31
A total of 542 respondents began the survey; among those, 430 completed the survey. Demographically, of those who completed surveys, 45% were under 40 years of age and about three-quarters (77%) identified as cigender female (Table 1). A majority identified as White non-Hispanic/Latino (65%) with 21% of respondents identifying as URiM. Thirty-eight percent were assistant professors, and 36% were less than 7 years posttraining. Most respondents were located either in the Northeastern (32%) or in the Western (30%) region of the United States. The percentage of URiM respondents working in the South (29%) was nearly twice the percentage of non-URiM respondents (16%, P<.05). The percentage of non-URiM respondents in the Midwest (19%) was nearly twice the percentage of URiM respondents (10%).
|
Characteristic
|
Total, N (%)
|
URiM, n (%)
|
Non-URiM, n (%)
|
P value
|
|
|
430 (100)
|
90 (21)
|
340 (79)
|
|
|
Age group
|
|
|
|
.426
|
|
<40 years
41-50 years
51-64 years
65+ years
|
193 (45)
109 (25)
98 (23)
30 (7)
|
43 (48)
25 (28)
19 (21)
3 (3)
|
150 (44)
84 (25)
79 (23)
27 (8)
|
|
|
Gender identity
|
|
|
|
.344
|
|
Cisgender female
Cisgender male
Other gender identity/sexual orientation
|
329 (77)
85 (20)
16 (4)
|
71 (79)
14 (16)
5 (6)
|
258 (76)
71 (21)
11 (3)
|
|
|
Race/ethnicity
|
|
|
|
<.001
|
|
White NH
Black NH
Hispanic/Latino/a/x
AI/AN NH
Native Hawaiian/Other
Pacific Islander NH
Asian/Asian American NH
Mixed race NH
Other NH
|
279 (65)
29 (7)
45 (10)
1 (0)
5 (1)
53 (12)
16 (4)
8 (2)
|
0 (0)
29 (32)
45 (50)
1 (1)
5 (6)
7 (8)
8 (9)
1 (1)
|
279 (82)
0 (0)
0 (0)
0 (0)
0 (0)
46 (14)
8 (2)
7 (2)
|
|
|
MD/DO as primary degree
|
384 (89)
|
81 (90)
|
303 (89)
|
.810
|
|
Faculty appointment
|
|
|
|
.475
|
|
Professor/Associate Professor
Assistant Professor
Clinical instructor
None of the above
|
154 (36)
165 (38)
52 (12)
59 (14)
|
27 (30)
40 (44)
12 (13)
11 (12)
|
127 (37)
125 (37)
40 (12)
48 (14)
|
|
|
Years since training
|
|
|
|
.285
|
|
<7 years
7-10 years
11-19 years
20+ years
|
155 (36)
58 (13)
103 (24)
114 (27)
|
38 (42)
13 (14)
22 (24)
17 (19)
|
117 (34)
45 (13)
81 (24)
97 (29)
|
|
|
Practice region
|
|
|
|
.005
|
|
Northeast
Midwest
South
West
Other
|
139 (32)
73 (17)
82 (19)
131 (30)
5 (1)
|
24 (27)
9 (10)
26 (29)
28 (31)
3 (3)
|
115 (34)
64 (19)
56 (16)
103 (30)
(1)
|
|
Nearly half of all respondents (43%) reported either frequent (37%) or intense (6%) feelings of IS while 45% reported moderate IS and 12% reported low feelings of IS (Table 2). Twenty-nine percent of respondents indicated that inadequate mentorship significantly or very significantly impeded their career growth. A greater percentage of respondents with frequent or intense IS reported that inadequate mentorship very significantly/significantly impeded their career growth, sometimes/infrequently/never feeling professionally well-integrated, and sometimes/infrequently/never perceiving a sense of belonging compared to respondents with low or moderate IS. Slightly more than one-third of URiM respondents (34%) reported that inadequate mentorship impeded their career growth compared with 27% of non-URiM respondents (P<.05, Figure 1). URiMs were significantly more likely to report sometimes, often, or always being left out of professional opportunities due to their race/ethnicity (P<.05). In addition, URiMs were more likely than non-URiMs to infrequently/never feel professionally well-integrated (29% vs 14%, respectively; P<.05). Lastly, URiMs were more likely than non-URiMs to infrequently/never feel a sense of belonging in their current professional position (19% vs 10%, respectively; P<.05).
|
|
|
Imposter syndrome type
|
|
Characteristic
|
Total, N (%)
|
Low/moderate, n (%)
|
Frequent/intense, n (%)
|
|
|
430 (100)
|
246 (57)
|
184 (43)
|
|
Do you believe inadequate mentoring has impeded your career growth?*
|
|
Very significantly/significantly
|
123 (29)
|
54 (22)
|
69 (38)
|
|
Somewhat significantly
|
92 (21)
|
53 (22)
|
39 (21)
|
|
Not significantly
|
210 (49)
|
137 (56)
|
73 (40)
|
|
Do you feel well-integrated into the network of your current professional position?*
|
|
Frequently
|
169 (39)
|
120 (49)
|
49 (27)
|
|
Sometimes
|
175 (41)
|
83 (34)
|
92 (50)
|
|
Infrequently/never
|
73 (17)
|
34 (14)
|
39 (21)
|
|
Do you feel a sense of belonging in your current professional position?*
|
|
Frequently
|
214 (50)
|
154 (63)
|
60 (33)
|
|
Sometimes
|
153 (36)
|
64 (26)
|
89 (48)
|
|
Infrequently/never
|
50 (12)
|
19 (8)
|
31 (17)
|
|
Ever felt left out of professional opportunities because of your race/ethnicity?*
|
|
Never
|
304 (71)
|
174 (71)
|
130 (71)
|
|
Sometimes
|
91 (21)
|
52 (21)
|
39 (21)
|
|
Often/always
|
28 (7)
|
16 (7)
|
12 (7)
|
|
*Fisher’s exact P value <.05 comparing the overall distribution of low/moderate and frequent/intense responses within each career experience. Note: Responses were missing for inadequate mentorship (n=5), feeling well-integrated (n=13), feeling a sense of belonging (n=13), and feeling left out of professional opportunities because of race/ethnicity (n=7). Across all questions, the missing data comprised 1% to 3% of responses.
|
The percentages of respondents with frequent or intense IS and unadjusted and adjusted odds ratios of frequent or intense IS by respondent characteristics are presented in Table 3. Compared with reference groups, the odds of frequent or intense IS were highest for respondents with fewer than 7 years since training completion (OR=3.45; 95% CI: 1.88, 6.30), who practiced in the Northeast (OR=2.23; 95% CI: 1.18, 4.22) or West (OR=1.98; 95% CI: 1.04, 3.78), who very significantly/significantly experienced inadequate mentorship as impeding career growth (OR=1.94; 95% CI: 1.13, 3.31), and who only sometimes (OR=2.77; 95% CI: 1.57, 4.87) or infrequently/never (OR=3.69; 95% CI: 1.378 9.87) felt a sense of professional belonging (Table 3). Notably, URiM cis-females were not more likely than non-URiM cicgender females to report frequent or intense IS.
|
Characteristic
|
Frequent/intense IS
|
Frequent/intense IS vs low/moderate IS
|
|
|
%
|
Unadjusted OR(95% CI)
|
Adjusted OR(95% CI)
|
|
Underrepresented in medicine (URiM)
|
|
|
|
Non-URiM
|
42.1
|
ref
|
ref
|
|
URiM
|
45.6
|
1.15 (0.72, 1.84)
|
1.00 (0.59, 1.72)
|
|
Gender identity
|
|
|
|
|
Cisgender male/other
|
30.7
|
ref
|
ref
|
|
Cisgender female
|
46.5
|
1.95 (1.21, 3.13)*
|
1.48 (0.85, 2.58)
|
|
Years since training
|
|
<7 years
|
59.4
|
4.86 (2.83, 8.36)*
|
3.45 (1.88, 6.30)*
|
|
7-10 years
|
44.8
|
2.72 (1.38, 5.36)*
|
1.88 (0.89, 4.00)
|
|
11-19 years
|
38.8
|
2.13 (1.18, 3.84)*
|
1.39 (0.72, 2.68)
|
|
20+ years
|
22.8
|
ref
|
ref
|
|
Region
|
|
|
|
|
Northeast
|
47.5
|
1.93 (1.09, 3.42)*
|
2.23 (1.18, 4.22)*
|
|
Midwest
|
43.8
|
1.67 (0.87, 3.21)
|
1.98 (0.95, 4.14)
|
|
South
|
31.7
|
ref
|
ref
|
|
West
|
45.0
|
1.75 (0.98, 3.12)
|
1.98 (1.04, 3.78)*
|
|
Degree to which inadequate mentorship impeded career growth
|
|
Very significantly/significantly
|
56.6
|
2.39 (1.51, 3.76)*
|
1.94 (1.13, 3.31)*
|
|
Somewhat significantly
|
55.7
|
1.38 (0.84, 2.28)
|
1.09 (0.62, 1.94)
|
|
Not significantly
|
34.8
|
ref
|
ref
|
|
How often do you feel well integrated into your profession?
|
|
Frequently
|
29.0
|
ref
|
ref
|
|
Sometimes
|
52.6
|
2.70 (1.73, 4.21)*
|
1.36 (0.77, 2.41)
|
|
Infrequently/never
|
53.4
|
2.79 (1.58, 4.91)*
|
0.69 (0.28, 1.67)
|
|
How often do you feel belonging in your current profession?
|
|
Frequently
|
28.0
|
ref
|
ref
|
|
Sometimes
|
58.2
|
3.54 (2.29, 5.49)*
|
2.77 (1.57, 4.87)*
|
|
Infrequently/never
|
62.0
|
4.13 (2.17, 7.85)*
|
3.69 (1.38, 9.87)*
|
|
Age group
|
|
<40 years
|
55.4
|
3.89 (1.61, 9.41)*
|
|
|
41-50 years
|
44.0
|
2.47 (0.99, 6.18)
|
|
|
51-64 years
|
22.4
|
0.92 (0.35, 2.41)
|
|
|
65+ years
|
23.3
|
ref
|
|
|
Primary degree
|
|
|
|
|
MD/DO
|
44.0
|
1.60 (0.84, 3.05)
|
|
|
Other
|
32.6
|
ref
|
|
|
Faculty appointment
|
|
Full/Associate professor
|
29.9
|
ref
|
|
|
Assistant professor
|
52.1
|
2.54 (1.60, 4.02)*
|
|
|
Clinical instructor
|
40.4
|
1.59 (0.83, 3.06)
|
|
|
None of the above
|
52.5
|
2.58 (1.39, 4.78)*
|
|
|
Ever felt left out of professional opportunities because of your race/ethnicity?
|
|
Never
|
42.8
|
ref
|
|
|
Sometimes
|
42.9
|
1.01 (0.63, 1.61)
|
|
|
Often/always
|
42.9
|
1.01 (0.46, 2.21)
|
|
Our study revealed that specific demographic factors (ie, years since training completion, which correlated with younger age and lower faculty rank; practice region) and career experiences (ie, inadequate mentorship, sense of belonging) are particularly associated with frequent or intense feelings of IS. We observed significant differences between URiM and non-URiM faculty in terms of career experiences. URiMs were not more likely to report frequent or intense IS compared to non-URiMs; but compared with non-URiMs, URiMs were more likely to report racial/ethnic discrimination in their careers, low professional integration, inadequate mentorship, and infrequent sense of belonging in the profession. The latter two are associated with frequent or intense IS.
Findings that URiM respondents report more racial/ethnic discrimination and inadequate mentorship in their career trajectories compared to non-URiM respondents confirm previous research. URiM health care professionals and trainees, 32-34 including family physicians, 35 reported experiences of racism and discrimination in the health care setting during direct patient care as well as during interactions with colleagues and institutions. Moreover, URiMs reported feeling unsupported by their institutions when they did experience such macro- and microagressions. 33, 35 Mentorship, however, is widely thought to be a crucial, supportive component of success in academic medicine 36-39 and may also be helpful in mitigating experiences of racial/ethnic discrimination. 40, 41 Yet, as reflected in our findings, URiMs often experience inadequate mentorship. 5, 42-45
Inadequate mentorship is also likely related to inadequate professional integration and sense of belonging—whether that factor is the cause, effect, or both. Previous research has corroborated our findings that URiMs often experience deficits in professional integration, 5, 46, 47 which may also have some relationship to inadequate mentorship. Low professional integration and belonging may also be connected to the severe underrepresentation of Black, Latino/a/x, Native American/America Indian and Pacific Islander medical students and faculty across the country. Underrepresented medical school enrollees and full-time URiM faculty across US medical schools have increased minimally over the past 40 years. 20, 48 While faculty diversity in the specialty of family medicine is higher than in other specialties, it still significantly lags behind that of the general US population. 49 Combined factors of covert and overt racial/ethnic discrimination and disproportionate burdens associated with diversity efforts, 5, 21, 50 augmented by inadequate mentoring, can exacerbate experiences of professional isolation and invisibility and lead to low professional integration for URiMs.
Considering our study results with prior findings on URiMs in academic medicine, 51-54 we are compelled to question the impact of racial/ethnic discrimination, inadequate mentorship, and low professional integration and belonging on the career advancement of URiMs. Compared to White faculty in academic medicine, URiMs are significantly less likely to advance in rank or faculty appointment. 55, 56 Despite their often greater workloads, few URiMs have leadership positions such as chairpersons or deans in academic institutions. 57 Given the differences we found between URiM and non-URiM respondents, we urge contemplation of how institutionalized racism can disallow adequate mentorship and produce suboptimal professional integration, ultimately negatively affecting career development. 58
When considering IS, our data do not reflect higher instances of the phenomenon among URiM respondents. Yet, URiMs and other faculty of color in academic settings often describe a sense of imposterism. 59, 60 We argue that rather than true IS among URiMs, an internalization of feelings of inadequacy and fraudulence as a result of institutionalized racism experienced across educational and career trajectories may instead subsequently be mislabeled as IS. This false attribution is important to recognize precisely because the group to which IS was originally ascribed may have vastly different educational, career, and social experiences than URiMs. IS is often noted to be intrinsic to a person and, consequently, must be addressed and overcome by the affected individual. 61, 62 This ascription puts the onus of change on individuals rather than on external structures of institutionalized racism that have upheld and perpetuated racial/ethnic discrimination and disseminated messages of not belonging in academia.
Our data builds on existing evidence that change is needed to achieve equity. Many recommendations exist for addressing the dearth of recruitment and retention among URiMs in academic medicine. 21, 50, 63, 64, 65 Leaders can take advantage of the wealth of literature documenting the unique challenges of URiMs to begin to dismantle the structures of institutionalized racism and oppression that contribute to feelings of IS, namely micro/macroaggressions and minority tax experiences that many URiMs disproportionately face in academia. 21, 50, 63-68 One example of action that leaders can take is to determine the racial/ethnic composition of departments/institutions to understand who and how many are underrepresented, while also then investigating whether URiMs are overrepresented on diversity committees, for instance, and therefore are taking on the brunt of DEI (diversity/equity/inclusion) efforts. Other important actions that leaders can take include intentional training on how to identify and address institutional racism in academia and holding not only their own organizational leadership accountable for change but also holding national specialty organizations accountable for implementing strategies to improve DEI and career development efforts of faculty across the specialty. 5 Lastly, leaders and their institutions can invest in developing and supporting senior mentors of all racial/ethnic backgrounds (including White allies) to promote greater integration of URiM faculty into their professional circles. Experienced mentors can do this not only by helping early to midcareer URiM faculty navigate scholarly work but also by revealing to young faculty what they need to know about the hidden curriculum of academia. In this way, mentors can serve as advocates for URiM faculty and can also support them through micro- and macroaggressions.67
Limitations
This study’s cross-sectional design limited causality, and the convenience sample of respondents limited generalizability of findings. Additionally, this study did not measure other factors that might contribute both to feelings of IS in general and to career advancement, especially among URiMs. Such factors include parental education, family income, and wealth. Nonetheless, to our knowledge, this is the first study to examine IS and associated factors among family medicine faculty.
Workforce diversity is intricately linked to attainment of health equity for patients. Yet, diversity alone is insufficient to address the disadvantage of some groups compared to others. Diversity must be combined with equity and welcoming institutional environments. For many URiMs, long-standing experiences of discrimination and exclusion continue to pave their educational and career experiences in medicine. To provide high-quality care for disadvantaged communities, URiM recruitment, retention, career development, promotion, and leadership in academic medicine must improve to equitably diversify our workforce. For URiMs in family medicine to succeed, we must work with allies and our leading professional organizations to implement strategies that address the disadvantage of those groups who have the least access to professional opportunities. Moreover, to function as optimal mentors for rising learners, URiMs also must have access to positions of power. Institutional inaction and maintenance of structural racism in medical academia has helped to create and perpetuate feelings of imposterism among URiMs, which may mask experiences of racial/ethnic discrimination. Our study findings reinforce that differential factors are associated with the lived experiences of historically underrepresented racial/ethnic groups with respect to their professional experiences. This work also brings to light that structural racism can have a detrimental impact on academic medical careers. The time to implement policies that promote the change we want and need, is now—not just for us as academic physicians, but for our patients.
Dr Carvajal’s time was supported in part by the American Academy of Family Physician’s Health Equity Fellowship and the National Institute of Child Health and Human Development; Dr Zambrana acknowledges the support, in part, of the Latino Research Institute at University of Austin for the 2021-2022 Distinguished Research Fellowship.
Oral presentation (virtual) on November 22, 2021, for the annual meeting of the North American Primary Care Research Group; Oral presentation on May 3, 2022, at the Society of Teachers of Family Medicine Annual Spring Conference in Indianapolis, Indiana.
References
-
Marrast LM, Zallman L, Woolhandler S, Bor DH, McCormick D. Minority physicians’ role in the care of underserved patients: diversifying the physician workforce may be key in addressing health disparities. JAMA Intern Med. 2014;174(2):289-291. doi: 10.1001/jamainternmed.2013.12756
-
Garcia AN, Kuo T, Arangua L, Pérez-Stable EJ. Factors associated with medical school graduates’ intention to work with underserved populations: policy implications for advancing workforce diversity.
Acad Med. 2018;93(1):82-89.
doi: 10.1097/ACM.0000000000001917
-
Jetty A, Hyppolite J, Eden AR, Taylor MK, Jabbarpour Y. Underrepresented minority family physicians more likely to care for vulnerable populations.
J Am Board Fam Med. 2022;35(2):223-224.
doi: 10.3122/jabfm.2022.02.210280
-
Zambrana RE, Harvey Wingfield A, Lapeyrouse LM, Dávila BA, Hoagland TL, Valdez RB. Blatant, subtle, and insidious: URiM faculty perceptions of discriminatory practices in predominantly White institutions.
Sociol Inq. 2017;87(2):207-232.
doi: 10.1111/soin.12147
-
Pololi L, Cooper LA, Carr P. Race, disadvantage and faculty experiences in academic medicine. J Gen Intern Med. 2010;25(12):1,363-1,369. doi: 10.1007/s11606-010-1478-7
-
Clance PR, Imes SA. The imposter phenomenon in high achieving women: dynamics and therapeutic intervention.
Psychotherapy (Chic). 1978;15(3):241-247.
doi: 10.1037/h0086006
-
Cheung L. Understanding Imposter Phenomenon in Graduate Students Using Achievement Goal Theory. ProQuest Information & Learning; 2018.
-
Thomas M, Bigatti S. Perfectionism, impostor phenomenon, and mental health in medicine: a literature review.
Int J Med Educ. 2020;11:201-213.
doi: 10.5116/ijme.5f54.c8f8
-
-
Deshmukh S, Shmelev K, Vassiliades L, Kurumety S, Agarwal G, Horowitz JM. Imposter phenomenon in radiology: incidence, intervention, and impact on wellness.
Clin Imaging. 2022;82:94-99.
doi: 10.1016/j.clinimag.2021.11.009
-
Gottlieb M, Chung A, Battaglioli N, Sebok-Syer SS, Kalantari A. Impostor syndrome among physicians and physicians in training: A scoping review.
Med Educ. 2020;54(2):116-124.
doi: 10.1111/medu.13956
-
Jacobs MD, Sasser JT. Impostor phenomenon in undergraduate nursing students: a pilot study of prevalence and patterns.
J Nurs Educ. 2021;60(6):329-332.
doi: 10.3928/01484834-20210520-05
-
Bravata DM, Watts SA, Keefer AL, et al. prevalence, predictors, and treatment of impostor syndrome: a systematic review.
J Gen Intern Med. 2020;35(4):1,252-1,275.
doi: 10.1007/s11606-019-05364-1
-
Levant B, Villwock JA, Manzardo AM. Impostorism in third-year medical students: an item analysis using the Clance impostor phenomenon scale.
Perspect Med Educ. 2020;9(2):83-91.
doi: 10.1007/S40037-020-00562-8
-
Bernard DL, Lige QM, Willis HA, Sosoo EE, Neblett EW. Impostor phenomenon and mental health: the influence of racial discrimination and gender.
J Couns Psychol. 2017;64(2):155-166.
doi: 10.1037/cou0000197
-
Lige QM, Peteet BJ, Brown CM. Racial identity, self-esteem, and the impostor phenomenon among African American college students.
J Black Psychol. 2017;43(4):345-357.
doi: 10.1177/0095798416648787
-
Cokley K, McClain S, Enciso A, Martinez M. An examination of the impact of minority status stress and impostor feelings on the mental health of diverse ethnic minority college students.
J Multicult Couns Devel. 2013;41(2):82-95.
doi: 10.1002/j.2161-1912.2013.00029.x
-
McClain S, Beasley ST, Jones B, Awosogba O, Jackson S, Cokley K. An examination of the impact of racial and ethnic identity, impostor feelings, and minority status stress on the mental health of black college students. J Multicult Couns Devel. 2016;44(2):101-117. doi: 10.1002/jmcd.12040
-
Cokley K, Smith L, Bernard D, et al. Impostor feelings as a moderator and mediator of the relationship between perceived discrimination and mental health among racial/ethnic minority college students.
J Couns Psychol. 2017;64(2):141-154.
doi: 10.1037/cou0000198
-
Xierali IM, Nivet MA, Rayburn WF. Full-time faculty in clinical and basic science departments by sex and underrepresented in medicine status: a 40-year review.
Acad Med. 2021;96(4):568-575.
doi: 10.1097/ACM.0000000000003925
-
Rodríguez JE, Campbell KM, Pololi LH. Addressing disparities in academic medicine: what of the minority tax?
BMC Med Educ. 2015;15(1):6.
doi: 10.1186/s12909-015-0290-9
-
Zambrana RE, Valdez RB, Pittman CT, Bartko T, Weber L, Parra-Medina D. Workplace stress and discrimination effects on the physical and depressive symptoms of underrepresented minority faculty.
Stress Health. 2021;37(1):175-185.
doi: 10.1002/smi.2983
-
McGregor LN, Gee DE, Posey KE. I feel like a fraud and it depresses me: the relation between the imposter phenomenon and depression. Soc Behav Pers. 2008;36(1):43-48. doi: 10.2224/sbp.2008.36.1.43
-
-
Kumar S, Jagacinski CM. Imposters have goals too: the imposter phenomenon and its relationship to achievement goal theory.
Pers Individ Dif. 2006;40(1):147-157.
doi: 10.1016/j.paid.2005.05.014
-
Chrisman SM, Pieper WA, Clance PR, Holland CL, Glickauf-Hughes C. Validation of the Clance Imposter Phenomenon Scale.
J Pers Assess. 1995;65(3):456-467.
doi: 10.1207/s15327752jpa6503_6
-
Robert Wood Johnson Foundation. National faculty survey. Published online 1995.
-
-
-
Taparra K, Deville C Jr. Native Hawaiian and other Pacific Islander representation among US allopathic medical schools, residency programs, and faculty physicians.
JAMA Netw Open. 2021;4(9):e2125051.
doi: 10.1001/jamanetworkopen.2021.25051
-
SAS. Version 9.4. SAS Institute Inc; 2013.
-
Mpalirwa J, Lofters A, Nnorom O, Hanson MD. Patients, pride, and prejudice: exploring Black ontarian physicians’ experiences of racism and discrimination.
Acad Med. 2020;95(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 59th Annual Research in Medical Education Presentations):S51-S57.
doi: 10.1097/ACM.0000000000003648
-
-
-
Serafini K, Coyer C, Brown Speights J, et al. Racism as experienced by physicians of color in the health care setting.
Fam Med. 2020;52(4):282-287.
doi: 10.22454/FamMed.2020.384384
-
Henry-Noel N, Bishop M, Gwede CK, Petkova E, Szumacher E. Mentorship in medicine and other health professions.
J Cancer Educ. 2019;34(4):629-637.
doi: 10.1007/s13187-018-1360-6
-
Kashiwagi DT, Varkey P, Cook DA. Mentoring programs for physicians in academic medicine: a systematic review.
Acad Med. 2013;88(7):1,029-1,037.
doi: 10.1097/ACM.0b013e318294f368
-
Bonifacino E, Ufomata EO, Farkas AH, Turner R, Corbelli JA. Mentorship of underrepresented physicians and trainees in academic medicine: a systematic review.
J Gen Intern Med. 2021;36(4):1,023-1,034.
doi: 10.1007/s11606-020-06478-7
-
Ortega G, Smith C, Pichardo MS, Ramirez A, Soto-Greene M, Sánchez JP. Preparing for an academic career: the significance of mentoring.
MedEdPORTAL. March 5, 2018:10690.
doi: 10.15766/mep_2374-8265.10690
-
Oliver KB Jr, Nadamuni MV, Ahn C, Nivet M, Cryer B, Okorodudu DO. Mentoring Black men in medicine.
Acad Med. 2020;95(12S Addressing Harmful Bias and Eliminating Discrimination in Health Professions Learning Environments):S77-S81.
doi: 10.1097/ACM.0000000000003685
-
Flores G, Mendoza FS, DeBaun MR, et al. Keys to academic success for under-represented minority young investigators: recommendations from the Research in Academic Pediatrics Initiative on Diversity (RAPID) National Advisory Committee.
Int J Equity Health. 2019;18(1):93.
doi: 10.1186/s12939-019-0995-1
-
Beech BM, Calles-Escandon J, Hairston KG, Langdon SE, Latham-Sadler BA, Bell RA. Mentoring programs for underrepresented minority faculty in academic medical centers: a systematic review of the literature.
Acad Med. 2013;88(4):541-549.
doi: 10.1097/ACM.0b013e31828589e3
-
Merchant JL, Omary MB. Underrepresentation of underrepresented minorities in academic medicine: the need to enhance the pipeline and the pipe.
Gastroenterology. 2010;138(1):19-26.E3.
doi: 10.1053/j.gastro.2009.11.017
-
Sumler ML, Capdeville M, Ngai J, Cormican D, Oakes D. A call for diversity: underrepresented minorities and cardiothoracic anesthesiology fellowship education.
J Cardiothorac Vasc Anesth. 2022;36(1):58-65.
doi: 10.1053/j.jvca.2021.09.028
-
Espino MM, Zambrana RE. “How do you advance here? How do you survive?” an exploration of under-represented minority faculty perceptions of mentoring modalities.
Rev Higher Educ. 2019;42(2):457-484.
doi: 10.1353/rhe.2019.0003
-
Elliott BA, Dorscher J, Wirta A, Hill DL. Staying connected: native American women faculty members on experiencing success.
Acad Med. 2010;85(4):675-679.
doi: 10.1097/ACM.0b013e3181d28101
-
Pololi LH, Evans AT, Gibbs BK, Krupat E, Brennan RT, Civian JT. The experience of minority faculty who are underrepresented in medicine, at 26 representative U.S. medical schools.
Acad Med. 2013;88(9):1,308-1,314.
doi: 10.1097/ACM.0b013e31829eefff
-
Morris DB, Gruppuso PA, McGee HA, Murillo AL, Grover A, Adashi EY. Diversity of the national medical student body: four decades of inequities.
N Engl J Med. 2021;384(17):1,661-1,668.
doi: 10.1056/NEJMsr2028487
-
Xierali IM, Nivet MA, Gaglioti AH, Liaw WR, Bazemore AW. Increasing family medicine faculty diversity still lags population trends.
J Am Board Fam Med. 2017;30(1):100-103.
doi: 10.3122/jabfm.2017.01.160211
-
Campbell KM. The diversity efforts disparity in academic medicine.
Int J Environ Res Public Health. 2021;18(9):4,529.
doi: 10.3390/ijerph18094529
-
Coombs AAT, King RK. Workplace discrimination: experiences of practicing physicians. J Natl Med Assoc. 2005;97(4):467-477.
-
Peterson NB, Friedman RH, Ash AS, Franco S, Carr PL. Faculty self-reported experience with racial and ethnic discrimination in academic medicine.
J Gen Intern Med. 2004;19(3):259-265.
doi: 10.1111/j.1525-1497.2004.20409.x
-
Filut A, Alvarez M, Carnes M. Discrimination toward physicians of color: a systematic review.
J Natl Med Assoc. 2020;112(2):117-140.
doi: 10.1016/j.jnma.2020.02.008
-
Flores G, Mendoza FS, Fuentes-Afflick E, et al. Hot topics, urgent priorities, and ensuring success for racial/ethnic minority young investigators in academic pediatrics.
Int J Equity Health. 2016;15(1):201.
doi: 10.1186/s12939-016-0494-6
-
Fassiotto M, Flores B, Victor R, et al. Rank Equity Index: measuring parity in the advancement of underrepresented populations in academic medicine.
Acad Med. 2020;95(12):1,844-1,852.
doi: 10.1097/ACM.0000000000003720
-
Kaplan SE, Raj A, Carr PL, Terrin N, Breeze JL, Freund KM. Race/ethnicity and success in academic medicine: findings from a longitudinal multi-institutional study.
Acad Med. 2018;93(4):616-622.
doi: 10.1097/ACM.0000000000001968
-
Yu PT, Parsa PV, Hassanein O, Rogers SO, Chang DC. Minorities struggle to advance in academic medicine: 1 12-y review of diversity at the highest levels of America’s teaching institutions.
J Surg Res. 2013;182(2):212-218.
doi: 10.1016/j.jss.2012.06.049
-
Zambrana RE, Williams DR. The intellectual roots of current knowledge on racism and health: relevance to policy and the national equity discourse.
Health Aff (Millwood). 2022;41(2):163-170.
doi: 10.1377/hlthaff.2021.01439
-
Ahmed A, Kaushal A. Cruz T, Kobuse Y, Wang K. Why is there a higher rate of impostor syndrome among BIPOC? December 8, 2020.
doi: 10.5281/ZENODO.4310477
-
-
-
-
Campbell KM, Hudson BD, Tumin D. Releasing the net to promote minority faculty success in academic medicine.
J Racial Ethn Health Disparities. 2020;7(2):202-206.
doi: 10.1007/s40615-020-00703-z
-
Robles J, Anim T, Wusu MH, et al. An approach to faculty development for underrepresented minorities in medicine.
South Med J. 2021;114(9):579-582.
doi: 10.14423/SMJ.0000000000001290
-
Amaechi O, Foster KE, Tumin D, Campbell KM. Addressing the gate blocking of minority faculty.
J Natl Med Assoc. 2021;113(5):517-521.
doi: 10.1016/j.jnma.2021.04.002
-
Zambrana RE. Toxic Ivory Towers: The Consequences of Work Stress on Underrepresented Minority Faculty. Rutgers University Press; 2018.
-
Smith R, Johnson A, Targan A, Piggott C, Kvach E. Taking our own temperature: using a residency climate survey to support minority voices.
Fam Med. 2022;54(2):129-133.
doi: 10.22454/FamMed.2022.344019
-
Foster KE, Johnson CN, Carvajal DN, et al. Dear White people.
Ann Fam Med. 2021;19(1):66-69.
doi: 10.1370/afm.2634



There are no comments for this article.