Background and Objectives: Innovations in medical school training are essential for family physicians to enter practice confident in addressing the opioid epidemic and substance use disorders. The objective of this study was to evaluate the effectiveness of a distance-learning addiction medicine curriculum led by family medicine physicians for third-year medical students.
Methods: Our prospective cohort study of third-year medical students compared our educational model to a traditional curriculum. Our distance-learning collaboration employed videoconferencing and community experts to engage students across Minnesota in an addiction medicine curriculum. Students in a family medicine-focused 9-month longitudinal integrated curriculum (LIC) participated in this 16-session curriculum while embedded in a rural or urban underserved community for their core third-year clerkships. We evaluated program effectiveness through a knowledge and attitude self-assessment survey of student participants before and after the program compared to students in a traditional curriculum.
Results: The pre- and postsurvey response rates, respectively, were 22.8% for the control group and 98.4% for the ECHO (Extension for Community Healthcare Outcomes) group. Compared to classmates in a traditional curriculum, program participants reported significantly higher self-perceived ability managing addiction concerns upon completing this curriculum (mean score of 3.2 vs 2.2 on a 5-point Likert scale, P<.001).
Conclusions: Data from our LIC showed promise that the model can be effective in building confidence in students’ abilities to practice addiction medicine. Because of its broad reach and low cost, this form of medical education may be a key model for medical schools to respond to the opioid epidemic and better serve our patients.
Opioid overdose deaths have increased in the United States from 49,660 in 2019 to 71,238 in 2021. 1 Medication for opioid use disorder (MOUD) is an effective approach for opioid use disorder (OUD) that reduces mortality and morbidity in patients with OUD. 2-7
As of 2018, 57% of rural counties in the United States had no waivered providers of buprenorphine. 8, 9 Despite the recent removal of buprenorphine waiver requirements, barriers to treating OUD persist. Physicians not prescribing buprenorphine reported these barriers: colleague resistance, absent specialty backup, and low confidence managing OUDs. 10
Our inspiration stemmed from this unmet need and the scope-of-practice potential of family physicians. To improve access to addiction care, we applied an innovative education model rooted in the principles of Project ECHO (Extension for Community Healthcare Outcomes). 11, 12 ECHO’s design consists of a hub of specialists, typically from at-large academic institutions, who teach spokes of family physicians in surrounding underserved areas through videoconferences. 11 In opioid education, ECHO models have been associated with increased buprenorphine prescriptions and retention in OUD treatment. 12-21
ECHO is an established tool for expanding a family physician’s scope of practice, and educators are seeking to model ECHO in undergraduate medical education. 22 Our model moved the hub of expertise from an academic institution to a rural community, where two family physicians were content experts with experience implementing addiction medicine care within a family clinic. These experts taught ECHO seminars to medical students participating in two family medicine-focused longitudinal integrated clerkships (LICs): the Rural Physician Associate Program (RPAP) and the Metropolitan Physician Associate Program (MetroPAP). 23, 24 These LICs are 9-month family medicine experiences where third-year medical students are embedded in a community clinic.
We compared our ECHO curriculum to the addiction medicine exposure within traditional clerkships through the change in pre- and postcurriculum survey responses across three cohorts of students. The primary outcomes were student self-rating of skill level and attitudes surrounding addiction care.
Our prospective cohort study compared outcomes between the ECHO and traditional curriculums in third-year medical students. This project was submitted to the University of Minnesota’s Institutional Review Board and approval was deemed unnecessary.
Our study sample consisted of third-year medical students at the University of Minnesota across three academic years (2018-2021). The ECHO group included 131 RPAP and MetroPAP students who participated in 16 sessions of our videoconferencing addiction medicine curriculum delivered by community physician experts each academic year. One-hour interactive lessons consisting of 2/3 didactic lessons and 1/3 case discussions occurred over the lunch hour every other week (see Appendix A). The traditional curriculum group consisted of 583 third-year clerkship students not enrolled in RPAP or MetroPAP. This group received the standard third-year clerkship education covering addiction medicine, which consisted of two 90-minute didactic presentations and case-based online modules.
We evaluated program effectiveness through a 16-question survey regarding students’ self-assessment of their knowledge and attitudes before and after the program—a Kirkpatrick Level 1 type of evaluation. We based the knowledge self-assessment portion of this survey on the SCAN-ECHO questionnaire used by previous authors who studied ECHO in relation to addiction medicine training. 15 We based the survey of student attitudes on current barriers to practicing physicians when treating OUD. 10
We used two sample t tests to test for differences in the mean scores between the control group and the intervention group at each time point. These results are summarized in Tables 1 through 3, shown in the next section. In addition, we compared the change in scores for the intervention group to the change in scores for the control group using generalized estimating equations with a repeated subject statement to account for the paired nature of the data. We carried out all analyses using SAS 9.4 (SAS Institute), and a P value <.05 was considered statistically significant.
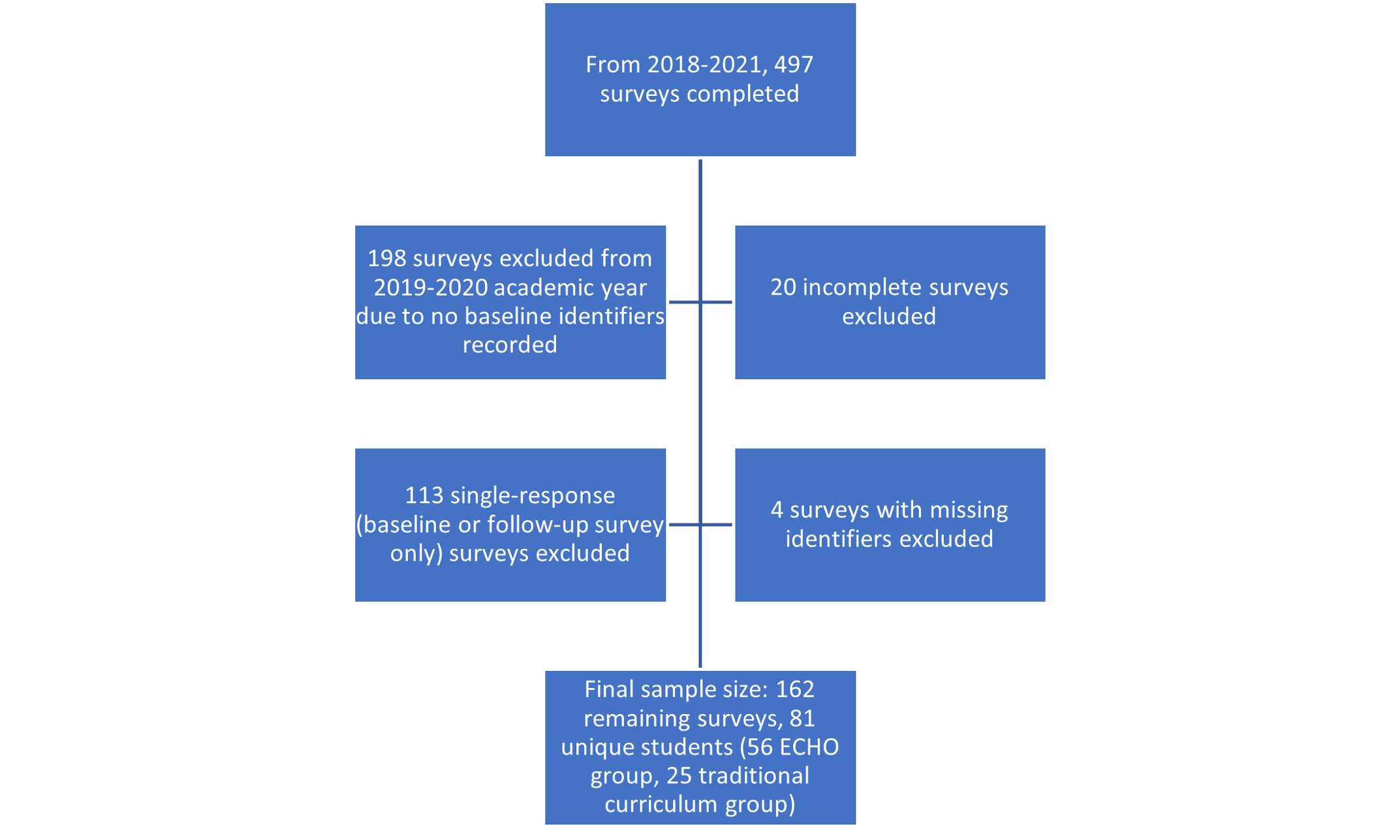
The pre- and postsurvey response rates were 98.4% for the ECHO group and 22.8% for the control group. We needed to exclude certain survey responses for reasons listed in Figure 1. We excluded responses from 2019-2020 because survey data did not include baseline identifiers. After exclusions, the final sample size included 56 ECHO students and 25 traditional clerkship students (ie, 112 and 50 survey responses, respectively). The ECHO and control groups shared similarities, including belonging to the same class in medical school and being assessed at the same time of year. Assessing for a difference in the change in each group negated the need for demographic matching. At the preintervention time point, the survey results revealed no statistically significant differences between the groups (Table 1).
|
Preintervention ability self-assessment
|
ECHO n=56 m ean (SD)
|
Traditional curriculum n=25 mean (SD)
|
P value
|
|
1. I am able to recognize opioid use disorder in patients.
|
2.6 (0.7)
|
2.7 (0.6)
|
.645
|
|
2. I can implement an addiction care plan.
|
1.9 (0.7)
|
1.8 (0.7)
|
.388
|
|
3. I can effectively use information from the prescription monitoring program.
|
1.9 (0.7)
|
1.9 (1.0)
|
.910
|
|
4. I can develop a care plan to effectively taper opioids for a patient.
|
1.8 (0.7)
|
1.8 (0.9)
|
.751
|
|
5. I can facilitate the development of a comprehensive addiction care program within a primary care clinic.
|
1.6 (0.7)
|
1.6 (0.7)
|
.867
|
|
6. I can engage a community in preventative or treatment strategies for opioid use disorder.
|
1.9 (0.8)
|
2.0 (0.9)
|
.612
|
|
7. I feel comfortable calculating conversion doses of commonly used opioids.
|
1.7 (0.8)
|
2.0 (1.3)
|
.289
|
|
8. I can assess and manage substance abuse comorbidities in patients with chronic pain.
|
1.8 (0.7)
|
1.8 (0.9)
|
.853
|
|
9. I can identify patients who may need a comprehensive, rehabilitative approach to pain treatment.
|
2.3 (0.9)
|
2.1 (1.0)
|
.357
|
|
10. I can assess and manage psychiatric comorbidities in patients with chronic pain.
|
2.0 (0.9)
|
1.8 (0.8)
|
.318
|
|
Mean score (Q1)
|
1.9 (0.6)
|
1.9 (0.7)
|
.941
|
Compared to the traditional clerkship, ECHO program participants reported significantly higher self-perceived ability in managing addiction concerns (mean score of 3.2 vs 2.2 on a 5-point Likert scale, P<.001; Table 2). Both groups reported strong beliefs that addiction medicine belongs in primary care, and these scores did not change over time (Table 3).
|
Postintervention ability self-assessment
|
ECHO n=56 mean (SD)
|
Traditional curriculum n=25 mean (SD)
|
P value
|
|
1. I am able to recognize opioid use disorder in patients.
|
3.6 (0.7)
|
3.1 (0.6)
|
.002
|
|
2. I can implement an addiction care plan.
|
2.9 (0.7)
|
2.2 (0.7)
|
<.001
|
|
3. I can effectively use information from the prescription monitoring program.
|
3.5 (0.7)
|
2.3 (1.0)
|
<.001
|
|
4. I can develop a care plan to effectively taper opioids for a patient.
|
2.8 (0.7)
|
2.0 (0.9)
|
<.001
|
|
5. I can facilitate the development of a comprehensive addiction care program within a primary care clinic.
|
2.8 (0.9)
|
1.8 (1.0)
|
<.001
|
|
6. I can engage a community in preventative or treatment strategies for opioid use disorder.
|
3.2 (0.9)
|
2.0 (0.9)
|
<.001
|
|
7. I feel comfortable calculating conversion doses of commonly used opioids.
|
3.0 (1.0)
|
1.9 (0.9)
|
<.001
|
|
8. I can assess and manage substance abuse comorbidities in patients with chronic pain.
|
3.2 (0.7)
|
2.2 (0.9)
|
<.001
|
|
9. I can identify patients who may need a comprehensive, rehabilitative approach to pain treatment.
|
3.4 (0.8)
|
2.7 (0.7)
|
<.001
|
|
10. I can assess and manage psychiatric comorbidities in patients with chronic pain.
|
3.2 (0.8)
|
2.3 (0.9)
|
<.001
|
|
Mean score (Q1)
|
3.2 (0.6)
|
2.2 (0.6)
|
<.001
|
|
Attitude assessment
|
Pooled change in response (ie, pre vs post)
|
|
ECHO (n=56) mean (SD)
|
Traditional curriculum (n=25) mean (SD)
|
P value
|
|
1. Primary care clinics have adequate resources to treat opioid addiction effectively.
|
0.0 (0.2)
|
-0.2 (0.3)
|
.600
|
|
2. Primary care can safely provide medication-assisted therapy (such as buprenorphine) for addiction.
|
0.5 (0.1)
|
0.3 (0.2)
|
.329
|
|
3. Primary care clinics have an obligation to provide medication-assisted therapy (such as buprenorphine) for addiction.
|
0.1 (0.2)
|
0.1 (0.1)
|
.875
|
|
4. I am likely to provide addiction treatment in my future practice.
|
-0.1 (0.2)
|
0.1 (0.2)
|
.408
|
|
5. I am likely to provide medication-assisted addiction treatment (such as buprenorphine) in my future practice.
|
-0.1 (0.2)
|
0.0 (0.2)
|
.476
|
|
6. If my practice does not yet provide medication-assisted addiction treatment, I plan to lead the development of a program.
|
-0.1 (0.2)
|
0.0 (0.2)
|
.469
|
|
Mean score (Q2)
|
0.0 (0.1)
|
0.1 (0.1)
|
.802
|
Our data showed that ECHO students reported greater confidence in addiction medicine training than traditional clerkship students. This finding demonstrates that our family physician-led curriculum was superior to a traditional curriculum in increasing self-perceived ability in third-year medical students to deliver addiction care. These results are consistent with prior ECHO model studies, which showed increased confidence in treating OUD. 13-16 In addition, the results demonstrated that attitudes among all students trended toward a belief that primary care has a duty to treat patients suffering from addiction.
The methodological weaknesses of the study included fewer responses among the control group and a lack of participant identifiers in year 2, which forced exclusion of that group from statistical analysis. In addition, we assessed self-perception of ability rather than an objective measure of competence, such as an exam.
Like ours, past ECHO projects have used specialist training to expand clinical care to areas of high need. The success of this curriculum is related to its longitudinal nature, use of real cases, and role-modeling of family medicine experts who successfully practice in addiction care. In future studies, adding a competency-based exam would allow for more objective outcomes data.
Acknowledgments
The authors acknowledge the assistance of Caroline Carlin, PhD, William Roberts, MD, Kurt Devine, MD, Heather Bell, MD, and Katie Stangl.
References
-
-
Ma J, Bao YP, Wang RJ, et al. Effects of medication-assisted treatment on mortality among opioids users: a systematic review and meta-analysis.
Mol Psychiatry. 2019;24(12):1,868-1,883.
doi:10.1038/s41380-018-0094-5
-
Ling W, Nadipelli VR, Aldridge AP, et al. Recovery from opioid use disorder (OUD) after monthly long-acting buprenorphine treatment: 12-month longitudinal outcomes from RECOVER, an observational study.
J Addict Med. 2020;14(5):e233-e240.
doi:10.1097/ADM.0000000000000647
-
Dupouy J, Palmaro A, Fatséas M, et al. Mortality associated with time in and out of buprenorphine treatment in french office-based general practice: A 7-year cohort study.
Ann Fam Med. 2017;15(4):355-358.
doi:10.1370/afm.2098
-
Sordo L, Barrio G, Bravo MJ, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies.
BMJ. 2017;357:j1550.
doi:10.1136/bmj.j1550
-
Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence.
Cochrane Database Syst Rev. 2014;(2):CD002207.
doi:10.1002/14651858.CD002207.pub4
-
Fullerton CA, Kim M, Thomas CP, et al. Medication-assisted treatment with methadone: assessing the evidence.
Psychiatr Serv. 2014;65(2):146-157.
doi:10.1176/appi.ps.201300235
-
-
Ghertner R. U.S. trends in the supply of providers with a waiver to prescribe buprenorphine for opioid use disorder in 2016 and 2018. Drug Alcohol Depend. 2019;204:107527. doi:10.1016/j.drugalcdep.2019.06.029
-
Andrilla CHA, Coulthard C, Larson EH. Barriers rural physicians face prescribing buprenorphine for opioid use disorder.
Ann Fam Med. 2017;15(4):359-362.
doi:10.1370/afm.2099
-
Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers.
N Engl J Med. 2011;364(23):2,199-2,207.
doi:10.1056/NEJMoa1009370
-
Zhou C, Crawford A, Serhal E, Kurdyak P, Sockalingam S. The impact of Project ECHO on participant and patient outcomes: a systematic review.
Acad Med. 2016;91(10):1,439-1,461.
doi:10.1097/ACM.0000000000001328
-
Anderson D, Zlateva I, Davis B, et al. Improving pain care with Project ECHO in community health centers.
Pain Med. 2017;18(10):1,882-1,889.
doi:10.1093/pm/pnx187
-
Carlin L, Zhao J, Dubin R, Taenzer P, Sidrak H, Furlan A. Project ECHO telementoring intervention for managing chronic pain in primary care: insights from a qualitative study.
Pain Med. 2018;19(6):1,140-1,146.
doi:10.1093/pm/pnx233
-
Ball S, Wilson B, Ober S, Mchaourab A. SCAN-ECHO for pain management: implementing a regional telementoring training for primary care providers.
Pain Med. 2018;19(2):262-268.
doi:10.1093/pm/pnx122
-
Tofighi B, Isaacs N, Byrnes-Enoch H, et al. Expanding treatment for opioid use disorder in publicly funded primary care clinics: exploratory evaluation of the NYC health + hospitals buprenorphine ECHO program.
J Subst Abuse Treat. 2019;106:1-3.
doi:10.1016/j.jsat.2019.08.003
-
Kawasaki S, Francis E, Mills S, Buchberger G, Hogentogler R, Kraschnewski J. Multi-model implementation of evidence-based care in the treatment of opioid use disorder in Pennsylvania.
J Subst Abuse Treat. 2019;106:58-64.
doi:10.1016/j.jsat.2019.08.016
-
Salvador J, Bhatt S, Fowler R, et al. Engagement with Project ECHO to increase medication-assisted treatment in rural primary care.
Psychiatr Serv. 2019;70(12):1,157-1,160.
doi:10.1176/appi.ps.201900142
-
Anderson JB, Martin SA, Gadomski A, et al. Project ECHO and primary care buprenorphine treatment for opioid use disorder: implementation and clinical outcomes.
Subst Abus. 2022;43(1):222-230.
doi:10.1080/08897077.2021.1931633
-
Gadomski A, Anderson J, Chung YK, Krupa N, Jenkins P. Full agonist opioid prescribing by primary care clinicians after buprenorphine training.
Subst Abus. 2022;43(1):69-75.
doi:10.1080/08897077.2020.1736709
-
Komaromy M, Duhigg D, Metcalf A, et al. Project ECHO (Extension for Community Healthcare Outcomes): a new model for educating primary care providers about treatment of substance use disorders.
Subst Abus. 2016;37(1):20-24.
doi:10.1080/08897077.2015.1129388
-
Jumreornvong O, Yang E, Race J, Appel J. Telemedicine and medical education in the age of COVID-19.
Acad Med. 2020;95(12):1,838-1,843.
doi:10.1097/ACM.0000000000003711
-
University of Minnesota Medical School. Rural Physician Associate Program (RPAP). Accessed September 10, 2021.
https://med.umn.edu/rpap
-



There are no comments for this article.