Background and Objectives: Impostor phenomenon (IP) can be described as feelings of inadequacy that exist despite apparent success. Although IP may be related to multiple important outcomes in physicians, it has not been examined among residency program directors (PDs).
Methods: The seven-item Leary Impostorism Scale (LIS) was added to the 2021 Council of Academic Family Medicine Educational Research Alliance (CERA) PD survey. In addition to standard questions, we surveyed PDs about their likelihood to leave their role, whether they started their PD role due to an unexpected transition, their beliefs concerning workplace evaluations relative to self-assessed performance, and their perceived support in completing PD responsibilities.
Results: Of the 257 PDs included in the survey (response rate approximately 41%), 28% (N=71) reported no IP. IP did not statistically differ across gender or race. LIS scores were lower among Hispanic/Latino respondents, but only 8% of our sample (N=20) identified as Hispanic/Latino. LIS scores did not significantly differ by PD likelihood to leave their position or for PDs starting their position due to a sudden transition. Respondents who felt that evaluations overestimated actual performance had higher LIS scores, as did those with lower levels of perceived support in completing administrative responsibilities and those with less time in their PD role.
Conclusions: Most PD respondents did not report high levels of IP. Short duration of PD role, lack of programmatic support, and negative self-evaluations were correlated with higher levels of IP. Future research should examine interventions or resources to help those with IP thrive.
Impostor phenomenon (IP) describes an intense experience of intellectual and professional fraudulence, often experienced in high-achieving individuals. 1, 2 Given the intensity of medical culture, IP has been examined in medical professionals and trainees and is associated with higher burnout, more anxiety and depression, and lower self-compassion and self-esteem. 3-5 IP has been found to occur in almost a quarter of male and half of female medical students. 5, 6 Studies have suggested that IP is more prevalent in females and individuals identifying as underrepresented in medicine (URiM). 2, 7, 8
A limitation of IP research is that the majority of studies examine individuals in training or early in their medical careers. Recent qualitative research highlights IP as a challenging component of professional identity formation in early-career physicians, 9 suggesting that IP may lessen as professional identities solidify. Similarly, a quantitative study showed that IP among attending surgeons is lower than among residents. 10 However, no studies have exclusively evaluated IP among physician leaders such as residency program directors (PDs), 6, 10 which is critical data given PDs’ significant influence in medical education. For PDs, career-related variables, such as suddenly transitioning into a new role or lack of organizational support, may influence IP, as could individuals’ interpretation of workplace feedback. 11-13 This study aimed to quantify the prevalence of IP in family medicine residency PDs and to examine associations with demographic and career experience variables.
This project was part of a study conducted by the Council of Academic Family Medicine Educational Research Alliance (CERA) and was approved by the American Academy of Family Physicians Institutional Review Board in September 2021. Survey data were collected between September and October 2021. 14
Our study used the seven-item Leary Impostorism Scale (LIS), which measures feelings of being an impostor or fraud using first-person statements on a five-point scale from 1=“Not at all characteristic of me” to 5=“Extremely characteristics of me.” 15 The LIS correlates with other IP measures, has good construct validity, has intermediate content validity and interpretability, and has intermediate to strong internal consistency. 15, 16, 17 Additionally, we developed four questions to capture PD career experiences.
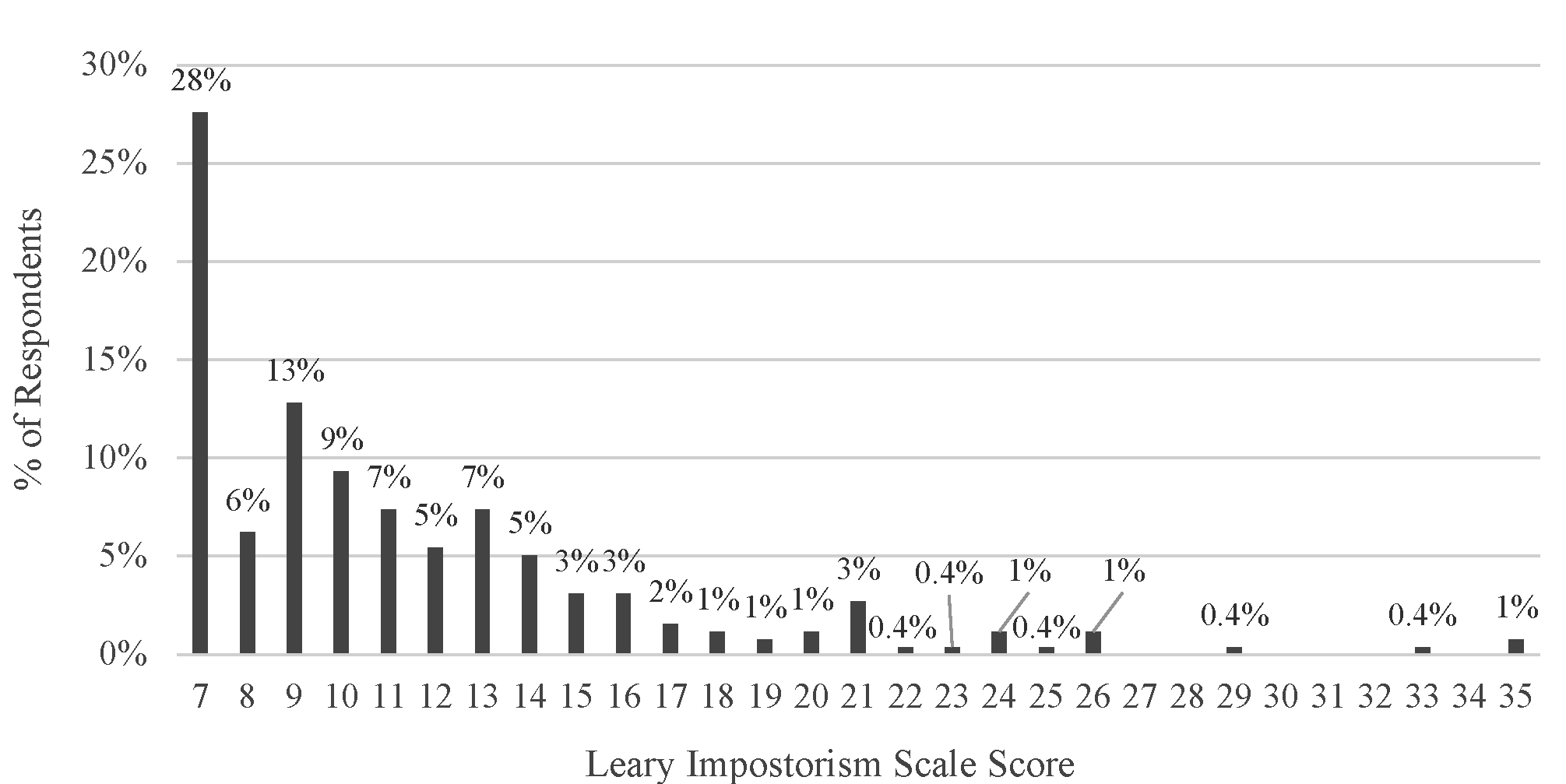
We excluded respondents who did not complete the LIS questions. By summing responses to the questions, we calculated one LIS score per respondent,. LIS scores range from 7 to 35 and were analyzed on a continuum. We considered a score of 7 (minimum possible) to reflect no IP. Due to ordinal, nonnormally distributed data, we used Mann-Whitney U tests (α=0.05) to compare LIS scores across PD demographic and career-related variables.
CERA identified 631 PDs, of whom 275 (44%) responded to the survey. Of those, 18 (6.5%) were excluded for not completing the LIS questions. Our study included responses from 257 PDs, representing 41% of all PDs identified by CERA (Table 1). The average LIS score was 11.4, the median was 10, the range was 7 to 35, the distribution was right-skewed, and 28% of respondents (N=71) reported no IP (Figure 1).
|
|
% (n) of respondents
|
|
Gender
Male
Female
Other or unspecified
|
52 (133)
46 (119)
2 (5)
|
|
Ethnicity
Hispanic/Latino
Non-Hispanic/Latino
Unspecified
|
8 (20)
89 (230)
3 (7)
|
|
Race
Non-White
White
Unspecified
|
15 (38)
79 (203)
6 (16)
|
|
Total years as a program director
<1 year
1 to <4 years
4 to <10 years
10+ years
Unspecified
|
6 (16)
33 (86)
35 (90)
25 (63)
1 (2)
|
|
Type of residency program
Community
University/military
Other or unspecified
|
81 (208)
17 (44)
2 (5)
|
|
Residency size
<19
19-31
>31
|
43 (110)
42 (107)
16 (40)
|
|
Size of the community the residency is located in
Less than 30,000
30,000 to 74,999
75,000 to 149,000
150,000 to 499,999
500,000 to 1 million
More than 1 million
Unspecified
|
11 (27)
13 (34)
22 (57)
26 (68)
12 (30)
15 (39)
1 (2)
|
|
Percentage of current faculty that identify as underrepresented in medicine
0%
<5%
6%-10%
11%-20%
21%-30%
31%-50%
>50%
Unspecified
|
23 (58)
16 (42)
16 (42)
18 (47)
8 (21)
9 (23)
8 (21)
1 (3)
|
The four questions we developed to capture PD career experiences are shown in Table 2. LIS scores did not differ by gender or race. Hispanic/Latino PDs had significantly lower LIS scores, indicating lower IP, compared to non-Hispanic/Latino PDs. However, only 8% of respondents (N=20) identified as Hispanic/Latino. Sixteen percent of respondents (N=42) indicated that they were likely to leave their position within the next year. LIS scores did not differ across those likely to leave versus those neutral or unlikely to leave. Nearly half of respondents (49%, N=125) started their role due to an unexpected transition, and LIS scores did not differ across those with versus without a sudden transition. Seven percent of responding PDs (N=17) agreed that evaluations overestimated their actual performance and had higher LIS scores compared to those who felt neutral or disagreed. Nearly half of respondents (45%, N=116) reported not having all the support they needed to complete their responsibilities, and they had higher LIS scores compared to those who felt neutral or well-supported. LIS scores were higher for respondents who had spent less time in their PD role (<4 years vs 4+ years).
|
|
% (n) of respondents
|
Leary Impostorism Scale m edian (IQR)
|
Leary Impostorism Scale a verage (SD)
|
P value*
|
|
Demographic-related variables**
|
|
|
|
|
|
Gender
Male
Female
|
53 (133)
47 (119)
|
10 (7-13)
10 (8-14)
|
10.8 (4.1)
12.1 (6.2)
|
.29
|
|
Ethnicity
Hispanic/Latino
Non-Hispanic/Latino
|
8 (20)
92 (230)
|
7 (7-9)
10 (8-13)
|
8.6 (2.6)
11.6 (4.9)
|
.001
|
|
Race
Non-White
White
|
16 (38)
84 (203)
|
10 (8-13)
10 (7-13)
|
11.8 (6.3)
11.4 (4.9)
|
.85
|
|
Career experience-related variables
|
|
|
|
|
|
I am likely to leave my position as program director within the next 12 months.
Likely or highly likely
Neutral, unlikely, or highly unlikely
|
16 (42)
84 (215)
|
10 (8-13.8)
10 (7-13)
|
12.3 (6.9)
11.2 (4.5)
|
.69
|
|
I started my role as program director due to a sudden or unexpected transition.
Agreed or strongly agreed
Neutral, disagreed, or strongly disagreed
|
49 (125)
51 (132)
|
10 (7-13)
10 (7.8-13)
|
11.3 (5.3)
11.5 (5.1)
|
.70
|
|
I feel that informal feedback and/or summative evaluation overestimate my actual performance as program director.
Agreed or strongly agreed
Neutral, disagreed, or strongly disagreed
|
7 (17)
93 (240)
|
14 (11-21)
10 (7-13)
|
15.7 (5.0)
11.1 (5.1)
|
<.001
|
|
I have as much support as I need to complete all my program director responsibilities.
Neutral, agreed, or strongly agreed
Disagreed or strongly disagreed
|
55 (141)
45 (116)
|
9 (7-12)
11 (9-14)
|
10.6 (4.6)
12.4 (5.7)
|
.001
|
|
Total years as a program director
<4 years
4+ years
|
40 (102)
60 (153)
|
11 (8-15)
9 (7-13)
|
12.8 (6.0)
10.6 (4.4)
|
.002
|
Our study found a lower prevalence of IP in PDs compared to prior studies of IP in medical trainees and medical students.3, 6 While 72% of PDs in our study (N=186) had an LIS score higher than the minimum possible score of 7, indicating some level of IP, a much smaller subgroup of PDs reported IP levels at the upper end of the LIS. We also found higher levels of IP in PDs who had spent less than 4 years in their role. Those findings suggest that IP may diminish as PDs gain experience and spend more time in professional roles. A qualitative study of professional identity formation among early career physicians also supports this interpretation; the researchers described IP as a part of a developmental process of learning to “fit in” to a professional role. 9
PDs in our study who reported inadequate support had higher IP than those who perceived adequate support. This effect could relate to an external locus of control or stress from societal or institutional expectations. 18, 19 Additionally, respondents who felt that evaluations overestimated their actual performance reported higher levels of IP. Qualitative research has suggested that this occurs “at the extreme end of the spectrum of self-doubt.”7 This finding may be amplified by perfectionistic tendencies. 20 Despite these findings, only 16% of respondents (N=42) reported planning to leave their position within the next year, indicating that the current average PD term may be longer than previously reported. 21
Several of our findings contradict existing literature. Unlike previous research correlating IP, burnout, and leaving a role, we did not find higher IP among PDs likely to leave their position. 22 While previous research has reported correlation between IP and sudden transitions in starting a new role, we did not find this correlation among PDs. 11 We found no difference in IP across gender, in contrast to prior studies showing higher IP in women, but consistent with one study showing no difference in IP across gender in business managers. 2, 7, 20 Hispanic/Latino PDs reported lower levels of IP, which was surprising given the additional challenges faced by URiM physicians. 8 Our findings suggest that individuals in PD roles may have different characteristics than previously studied medical students and residents. 6, 7
Our study had several limitations. While our response rate was similar to prior CERA studies, our results may not generalize to PDs who did not respond or to other medical specialties. The number of residency PDs is constantly changing, so we could not report the exact representativeness of our sample. All data is self-reported and cross-sectional. Our data was limited to information collected within the 2021 CERA survey.
PDs have considerable responsibilities and influence on medical trainees; therefore, understanding the unique challenges and needs of this population is important. This study provided novel evidence that the prevalence of IP may be lower among experienced family medicine PDs than among physicians earlier in their careers. However, while IP may be a component of professional identity formation, seeking to understand a subgroup of individuals experiencing IP at a higher level or for a longer duration than their peers may be beneficial. Future research should examine associations between IP and institutional support for PDs, self-evaluations, and length of time in the PD role. 23 Further work is also needed to determine optimal interventions and resources to help address IP.
Presentations
This study was presented at the 2023 STFM Annual Spring Conference in Tampa, Florida, April 30-May 2, 2023.
References
-
Clance PR, OToole MA. The imposter phenomenon: an internal barrier to empowerment and achievement.
Women Ther. 1987;6(3):51-64.
doi:10.1300/J015V06N03_05
-
Clance PR, Imes SA. The imposter phenomenon in high achieving women: dynamics and therapeutic intervention.
Psychotherapy. 1978;15(3):241-247.
doi:10.1037/h0086006
-
Villwock JA, Sobin LB, Koester LA, Harris TM. Impostor syndrome and burnout among American medical students: a pilot study.
Int J Med Educ. 2016;7:364-369.
doi:10.5116/ijme.5801.eac4
-
Rosenthal S, Schlussel Y, Yaden MB, et al. Persistent impostor phenomenon is associated with distress in medical students.
Fam Med. 2021;53(2):118-122.
doi:10.22454/FamMed.2021.799997
-
-
Gottlieb M, Chung A, Battaglioli N, Sebok-Syer SS, Kalantari A. Impostor syndrome among physicians and physicians in training: A scoping review.
Med Educ. 2020;54(2):116-124.
doi:10.1111/medu.13956
-
. Bravata DM, Watts SA, Keefer AL, et al. Prevalence, predictors, and treatment of impostor syndrome: a systematic review.
J Gen Intern Med. 2020;35(4):1,252-1,275.
doi:10.1007/s11606-019-05364-1
-
Sturges D. Imposter phenomenon and underrepresented minorities: what physician assistant educators need to know.
J Physician Assist Educ. 2018;29(2):126-128.
doi:10.1097/JPA.0000000000000194
-
Stelling V, Brianna E, Andersen CA, et al. Fitting in while standing out: professional identity formation, imposter syndrome, and burnout in early career faculty physicians.
Acad Med. 2023;98(4):514-520.
doi:10.1097/ACM.0000000000005049
-
Leach PK, Nygaard RM, Chipman JG, Brunsvold ME, Marek AP. Impostor phenomenon and burnout in general surgeons and general surgery residents.
J Surg Educ. 2019;76(1):99-106.
doi:10.1016/j.jsurg.2018.06.025
-
LaDonna KA, Ginsburg S, Watling C. “Rising to the level of your incompetence”: what physicians’ self-assessment of their performance reveals about the imposter syndrome in medicine.
Acad Med. 2018;93(5):763-768.
doi:10.1097/ACM.0000000000002046
-
Mcdowell WC, Iii WLG, Geho PR. The impact of self-efficacy and perceived organizational support on the imposter phenomenon. Am J Manag. 2015;15(3):23-29.
-
-
Seehusen DA, Mainous AG III, Chessman AW. Creating a centralized infrastructure to facilitate medical education research.
Ann Fam Med. 2018;16(3):257-260.
doi:10.1370/afm.2228
-
Leary MR, Patton KM, Orlando AE, Funk WW. The impostor phenomenon: self-perceptions, reflected appraisals, and interpersonal strategies.
J Pers. 2000;68(4):725-756.
doi:10.1111/1467-6494.00114
-
Freeman KJ, Houghton S, Carr SE, Nestel D. Measuring impostor phenomenon in healthcare simulation educators: a validation of the clance impostor phenomenon scale and leary impostorism scale.
BMC Med Educ. 2022;22(1):139.
doi:10.1186/s12909-022-03190-4
-
Mak KKL, Kleitman S, Abbott MJ. Impostor phenomenon measurement scales: a systematic review.
Front Psychol. 2019;10:671.
doi:10.3389/fpsyg.2019.00671
-
Parkman A. The imposter phenomenon in higher education: incidence and impact. J High Educ Theory Pract. 2016;16(1):51-60.
-
Sauer EM. The Imposter Phenomenon: Locus of Control, Sex, Level of Education, Generation Status, Age and Race in a College Population. Master’s thesis. Ball State University; 1991.
-
Rohrmann S, Bechtoldt MN, Leonhardt M. Validation of the impostor phenomenon among managers.
Front Psychol. 2016;7:821.
doi:10.3389/fpsyg.2016.00821
-
-
-
Rivera N, Feldman EA, Augustin DA, Caceres W, Gans HA, Blankenburg R. Do I belong here? Confronting imposter syndrome at an individual, peer, and institutional level in health professionals.
MedEdPORTAL. 2021;17:11166.
doi:10.15766/mep_2374-8265.11166



There are no comments for this article.