Background and Objectives: Workforce diversity in primary care is critical for improved health outcomes and mitigation of inequities. However, little is known about the racial and ethnic identities, training histories, and practice patterns of family physicians who provide abortions.
Methods: Family physicians who graduated from residency programs with routine abortion training from 2015 through 2018 completed an anonymous electronic cross-sectional survey. We measured abortion training, intentions to provide abortion, and practice patterns, and examined differences between underrepresented in medicine (URM) and non-URM physicians using χ2 tests and binary logistic regression.
Results: Two hundred ninety-eight respondents completed the survey (39% response rate), 17% of whom were URM. Similar percentages of URM and non-URM respondents had abortion training and had intended to provide abortions. However, fewer URMs reported providing procedural abortion in their postresidency practice (6% vs 19%, P=.03) and providing abortion in the past year (6% vs 20%, P=.023). In adjusted analyses, URMs were less likely to have provided abortions after residency (OR=.383, P=.03) and in the past year (OR=.217, P=.02) compared to non-URMs. Of the 16 noted barriers to provision, few differences were evident between groups on the indicators measured.
Conclusions: Differences in postresidency abortion provision existed between URM and non-URM family physicians despite similar training and intentions to provide. Examined barriers do not explain these differences. Further research on the unique experiences of URM physicians in abortion care is needed to then consider which strategies for building a more diverse workforce should be employed.
Workforce diversity is critical for improved health outcomes and mitigation of health disparities. 1 Physicians who are currently and historically racially and/or ethnically underrepresented in medicine (URM), 2 especially those in primary care, are more likely than non-URM physicians to practice in underresourced areas and to serve marginalized patients, who are disproportionately from communities of color. 3, 4 In addition, racial and ethnic concordance between patients and physicians, especially in primary care, is associated with improved patient experience, 5 increased trust and intention to adhere to treatment recommendations, 6, 7 and higher rates of preventive care. 8 However, only 11% of all physicians and 7.7% of academic medical faculty 9 identify as Black/African American, Latino/a/x American, Indian/Alaska Native, or Native Hawaiian/Pacific Islander, the groups that are underrepresented in medicine, compared to the general population. 2 The percentage of URM physicians within family medicine is slightly higher, with 12.5% of practicing family physicians 10 and 18% of family medicine residents identifying as URM. 11
Abortion care is an important component of full spectrum primary care. While data exist for abortion patients, showing that in 2014 at least 56% of patients who accessed abortion were from underrepresented groups, 12 little data exist about the racial and ethnic identities of abortion providers. One study of practicing obstetrics and gynecology (OB/GYN) physicians found no relationship between race and ethnicity and abortion provision, 13 while a study among abortion-trained OB/GYN residents found that Asian and Latino/a/x residents had the highest rates of intention to provide abortions and Black residents had the lowest rates. 14 However, no data exist about the racial and/or ethnic identities of current abortion providers of any specialty, including family medicine. Additionally, little is known about the professional trajectories of URM physicians with respect to sexual and reproductive health care (SRH) generally and abortion services in particular. Because many patients prefer to access abortion within primary care settings, 15-17 increasing numbers of family physicians are being trained in abortion,18, 19 and URM primary care physicians are more likely to practice in disadvantaged communities, 3 a better understanding of the characteristics of abortion providers within family medicine is crucial.
To begin to address the notable knowledge gap, particularly in the context of increasing restrictions on abortion, the objectives of this study were to assess the training histories and practice patterns of family physicians with access to abortion training during residency and to examine differences between URM and non-URM physicians. Specifically, our study aimed to explore differences in abortion training, intention to provide, and current abortion provision.
Study Design, Participants, and Instrument
For this cross-sectional study, we recruited practicing family physicians who graduated from 24 residency programs receiving funding and technical assistance from Reproductive Health Education in Family Medicine (RHEDI). 1 As part of standard residency training, residencies with RHEDI training cover medication and first-trimester procedural abortion, as well as full-spectrum SRH. We invited graduates who completed residency between 2015 and 2018 to complete an anonymous electronic 72-item survey that was pretested with a small group of RHEDI program alumni who completed residency prior to 2015. The survey included items about respondent demographics, abortion and other SRH training during residency, and current provision of SRH services, including abortion, contraception, miscarriage management, pregnancy options counseling, and abortion options counseling. The survey also asked respondents to report their intentions to provide abortion at graduation from medical school and residency, whether they had considered providing abortion once in practice, and which, if any, barriers to abortion provision they had encountered.
Recruitment Procedures
We recruited participants from October 2020 through December 2020, drawing primarily on RHEDI’s existing database of physicians who graduated from residencies with RHEDI programs. We approached 763 potential respondents; most (621) directly received a recruitment email that included an individualized web-based survey link. Additionally, some residency faculty assisted in disseminating the survey to their alumni. In addition to the initial invitation, we sent reminder emails at 2-week intervals to those who had not completed the survey. Over the course of the 12-week recruitment period, we sent supplemental recruitment materials via postal mail to those potential participants for whom mailing addresses were known. For those graduates whose email addresses bounced, we undertook internet research and outreach to their residency programs to identify their current contact information. Participants received a $40 gift card electronically as compensation for their time. At the introduction to the survey, we included a consent statement; consent was therefore implied by completion of the survey. This study was approved by the Montefiore Medical Center Institutional Review Board.
Analysis
We exported data from the secure Key Survey website into SPSS for analysis. Using the Association of American Medical Colleges’ definition of URM, 2 we assessed outcome variables by URM vs non-URM. Participants who specified that they were African American/Black, first-generation African, African Caribbean, African Latino, Latino/a/x, Native American/Alaska Native, or Native Hawaiian/other Pacific Islander all were classified as URM, while those who chose only White/Caucasian were categorized as non-URM. For those who selected Asian, a follow-up question on specific countries of origin allowed us to distinguish between those currently categorized as URM from four Southeast and refugee Asian countries (Vietnam, Cambodia, Indonesia, and Laos) and the remainder of those in the Asian group, who were not URM. Those who selected multiple race and ethnicity options were categorized as URM if any of the options they selected fell into the URM group.
Outcome variables included abortion training, previous intention to provide abortions, and current abortion provision in any setting. In addition to examining descriptive statistics for variables of interest, we used χ2 tests to examine the statistical significance of differences in outcome variables between URMs and non-URMs, and we used logistic regression for multivariate analysis. For multivariate analysis, we included a priori those variables in our model that previous research led us to hypothesize would have a relationship with abortion provision 20-22 and/or those significantly associated with provision on a bivariate level. 23 Statistical significance was set at 2-sided α=.05, and all analysis was conducted in SPSS version 27.
Respondent Demographics, Practice Characteristics, and Patient Population
Two hundred ninety-eight family physicians completed the survey (39% response rate). We found no significant differences between responders and nonresponders in terms of year of residency graduation, although response rates were higher among respondents who completed residency in the Northeast and West compared to those who did so in the South and Midwest (data not shown.) We excluded 12 respondents not providing clinical care in the United States and 3 not providing adequate information to determine their URM status. Of the 283 remaining respondents, 16.6% (n=47) identified as URM. We found no significant differences between URMs and non-URMs with respect to gender, region of the country, primary practice setting, urban/rural status, and faculty status (Table 1). URM physicians saw a higher proportion of patients covered by Medicaid; while a slightly higher proportion practiced at federally qualified health centers (FQHCs), that difference was not statistically significant when comparing a primary practice setting of an FQHC to all other settings (P=.066).
|
|
Non-URM graduates (n=236), % (n)
|
URM graduates (n=47), % (n)
|
P value
|
|
Race and ethnicity
White
Asian American
Latino/a/x
Black/African American*
Native American/Alaska Native
Pacific Islander/Native Hawaiian
Mixed race
|
...
80 (189)
19 (44)
...
...
...
...
1 (3)
|
...
...
9 (4)
38 (18)
30 (14)
2 (1)
2 (1)
19 (9)
|
<.001
|
|
Gender
Cisgender male
Cisgender female
Transgender or nonbinary
|
...
25.8 (61)
72.4 (171)
1.7 (4)
|
...
29.8 (14)
70.2 (33)
0
|
.591
|
|
Current region of practice**
Northeast
Midwest
South
West
|
(n=230)
28.3 (65)
6.5 (15)
11.7 (27)
53.5 (123)
|
(n=45)
26.7 (12)
11.1 (5)
11.1 (5)
51.1 (23)
|
.759
|
|
Primary practice environment
Urban
Suburban
Rural
|
...
50.8 (120)
34.3 (81)
14 (35)
|
...
53.2 (25)
25.5 (12)
21.3 (10)
|
.370
|
|
Primary practice setting
Family medicine/primary care (not FQHC)
Family medicine/community health (eg, FQHC)
Private practice***
Inpatient hospital
Dedicated abortion clinic
Other
|
...
42.4 (100)
34.7 (82)
5.9 (14)
4.2 (10)
1.3 (3)
11.4 (27)
|
...
34 (16)
48.9 (23)
0
2.1(1)
0
14.9 (7)
|
.220
|
|
Payer mix
50% or more of physician’s patients are on Medicaid
20% or more of physician’s patients are uninsured
|
...
47 (111)
57.6 (136)
|
...
63.8 (30)
66 (31)
|
...
.035
.289
|
|
Faculty at a residency program
|
37.7 (89)
|
38.3 (18)
|
.940
|
|
Trained in medication abortion during residency*** (n=282)
|
85.5 (201)
|
83.0 (39)
|
.654
|
|
Trained in procedural abortion during residency
|
79.7 (188)
|
76.6 (36)
|
.637
|
|
Trained in any type of abortion during residency*** (n=281)
|
87.2 (205)
|
84.8 (39)
|
.653
|
Abortion Training During Residency
While all respondents trained at residency programs with routine integrated abortion training, not all accessed both medication abortion and procedural abortion training, or even any abortion training at all. The percentage of respondents who completely opted out of abortion training was similar between groups, with 13.3% of non-URM and 14% of URMs doing so. Abortion training rates were similar between the two groups as well (Table 1).
Intention to Provide Abortion
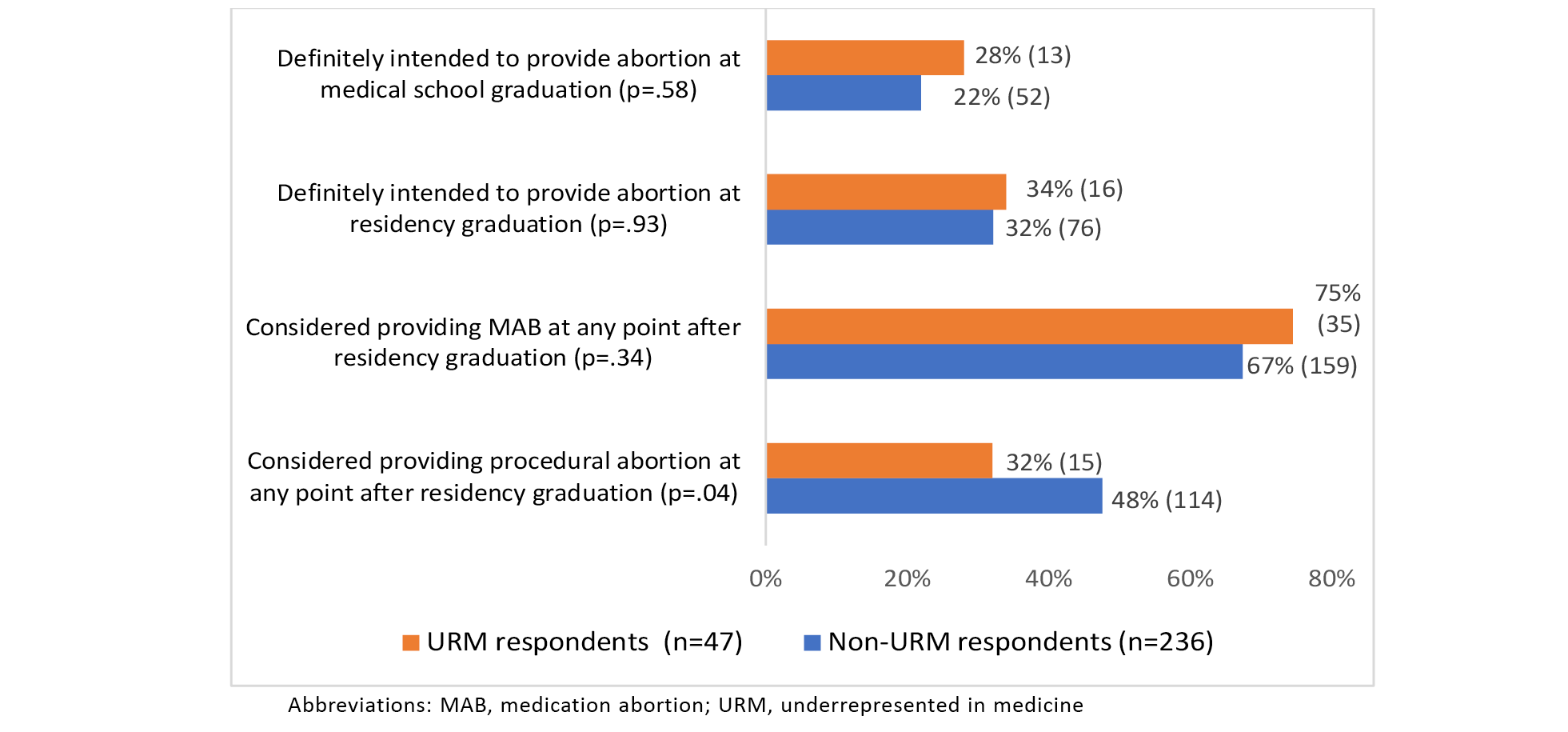
We found no statistically significant differences between URMs and non-URMs in their recalled intention to provide abortions at medical school graduation or at residency graduation (Figure 1). While both groups considered providing medication abortion after residency graduation at similar rates, those in the URM group were significantly less likely to have considered providing procedural abortion after residency.
Abortion Provision After Residency
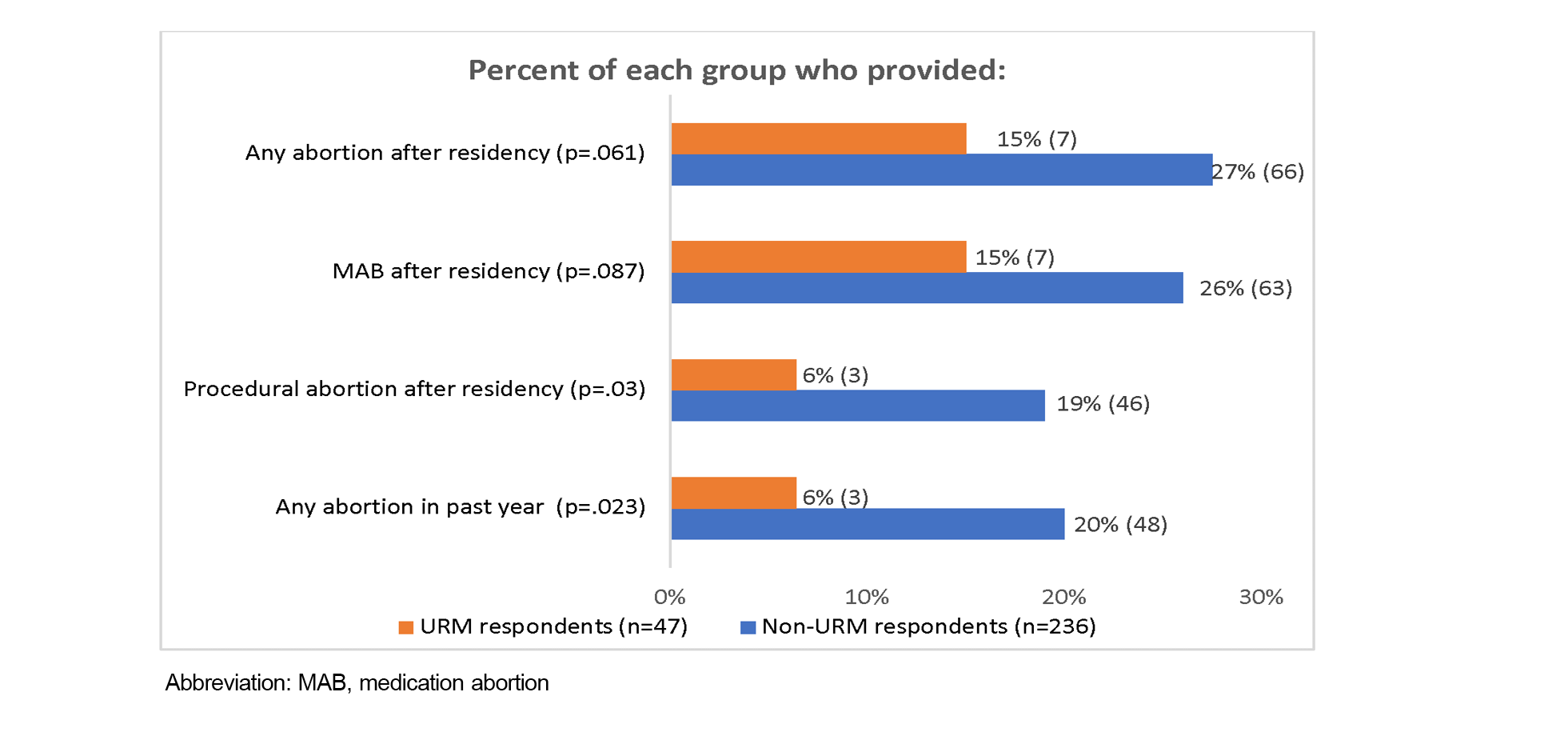
In all categories of provision, URM respondents were less likely to have provided abortions than their non-URM colleagues. URM respondents reported significantly lower rates of abortion provision in the past 12 months than non-URM respondents (6% vs 20%; P=.023). Rates were particularly low for procedural abortion provision after residency graduation (6% vs 19%, P=.03; Figure 2).
Multivariate Analysis
Using binary logistic regression, we examined abortion provision while accounting for factors including URM status, gender, region, urbanity setting, and faculty status because these were statistically associated with provision during bivariate analysis. We also accounted for the degree to which physicians’ patients were on Medicaid because that was significantly different between the two groups. In addition, we included other important demographic factors (ie, practice region, primary practice setting) a priori that were not significantly associated on a bivariate level in multivariate analyses because we recognized that they were important factors to consider given existing regional and practice limitations on abortion provision, although those ultimately were not part of a best-fit model.
In the adjusted logistic regression analysis, we still found that URMs remained less likely to provide abortion, by 61% (Table 2) compared to non-URM respondents. Additionally, being in a suburban area, practicing in the Northeast and West regions, and not being faculty were all significantly associated with a lower likelihood of abortion provision after residency graduation.
We also used a binary logistic regression model to examine the relationship of any abortion provision in the past year with the same demographic factors. In this model, URMs were also less likely to provide abortion in the past year, by 78% (Table 2) compared to non-URM respondents. Respondents in nonurban settings and nonresidency faculty were also significantly less likely to provide abortion in the past year.
|
A: Adjusted Associations Between Abortion Provision After Residency and Demographic and Practice Factors
|
|
Demographic characteristic*
|
Abortion provision after residency, % (n)
|
Adjusted odds ratio (OR)
|
Confidence interval (CI)
|
P value
|
|
URM status
*Non-URM (n=236)
URM (n=47)
|
...
28 (66)
14.9 (7)
|
0.38
|
0.15–0.96
|
.04
|
|
Gender
*Cisgender male (n=85)
Cisgender female, trans, and gender nonconforming (n=241)
|
...
16.5 (14)
26.1 (63)
|
1.82
|
0.88–3.77
|
.107
|
|
Current region of practice
*South and Midwest (n=59)
Northeast and West (n=259)
|
...
32.2 (19)
20.8 (54)
|
0.40
|
0.19–0.88
|
.015
|
|
Urbanity of practice setting
*Urban (n=157)
Suburban (n=108)
Rural (n=61)
|
...
32.5 (51)
13.9 (15)
18 (11)
|
...
...
0.29
0.83
|
...
...
0.13–0.65
0.35–1.96
|
...
...
.002 .678
|
|
Faculty status
*Currently faculty at a residency program (n=121)
Not faculty at a residency program (n=205)
|
...
37.2 (45)
15.6 (32)
|
0.32
|
0.17–0.60
|
<.001
|
|
Percent of physician’s patients covered by Medicaid
*Less than 50% covered by Medicaid (n=172)
More than 50% covered by Medicaid (n=154)
|
...
18.6 (32)
29.2 (45)
|
1.19
|
0.639–2.22
|
.581
|
|
B: Adjusted Associations Between Abortion Provision in the Past Year and Demographic and Practice Factors
|
|
Demographic characteristic
|
Abortion provision in the past year, % (n)
|
Adjusted odds ratio (OR)
|
Confidence interval (CI)
|
P value
|
|
URM status
*Non-URM (n=236)
URM (n=47)
|
...
20.3 (48)
6.4 (3)
|
0.22
|
(0.06–0.77)
|
.018
|
|
Gender
*Cisgender male (n=85)
Cisgender female, trans, & gender nonconforming (n=241)
|
...
11.8 (10)
17.4 (42)
|
1.47
|
(0.64–3.36)
|
.366
|
|
Current region of practice
*South and Midwest (n=59)
Northeast and West (n=259)
|
...
22 (13)
13.9 (36)
|
0.44
|
(0.19–1.01)
|
. 052
|
|
Urbanity of practice setting
*Urban (n=157)
Suburban (n=108)
Rural (n=61)
|
...
24.2 (38)
7.4 (8)
9.8 (6)
|
...
...
0.22
0.70
|
...
...
(0.08–0.60)
(0.25–1.95)
|
...
...
.003
.487
|
|
Faculty status
*Currently faculty at a residency program (n=121)
Not faculty at a residency program (n=205)
|
...
26.4 (32)
9.8 (20)
|
0.28
|
0.14–0.58
|
<.001
|
|
Percent of physician’s patients covered by Medicaid
*Less than 50% covered by Medicaid (n=172)
More than 50% covered by Medicaid(n=154)
|
...
12.2 (21)
20.1 (31)
|
0.17
|
(0.55–2.27)
|
.759
|
Barriers to Abortion Provision
We also compared the percentages of URM and non-URM respondents who indicated encountering each of the individual barriers listed in Table 3 for both medication and procedural abortion provision. Only respondents who considered providing each type of abortion were asked about these barriers (n=164 for medication abortion; n=129 for procedural abortion). Overall barriers were similar for URM and non-URM providers; but for medication abortion, a higher percentage of URM respondents noted that they encountered barriers including, “Feeling I don’t have adequate skills to provide abortion,” “Administrative, staff, or colleague resistance,” and “Difficulty arranging backup for complications.” While the latter two barriers were not statistically significant, differences between groups were more than 15%.
|
Provision barriers
|
Those who considered providing medication abortion (n=164)
|
Those who considered providing procedural abortion (n=129)
|
|
% Non-URM (n=159)
|
% URM (n=35)
|
P value
|
% Non-URM (n=114)
|
% URM (n=15)
|
P value
|
|
Perception of inadequate skills
|
34.6
|
54.3
|
.03
|
41.2
|
46.7
|
.89
|
|
Concern for personal/family safety
|
18.2
|
0
|
.01
|
21.9
|
6.7
|
.17
|
|
Administrative/staff/colleague resistance
|
45.9
|
62.9
|
.07
|
43.0
|
46.7
|
.79
|
|
State-specific regulations
|
18.2
|
5.7
|
.07
|
20.2
|
0
|
.06
|
|
Difficulty arranging backup for complications
|
30.8
|
45.7
|
.09
|
28.1
|
20.0
|
.51
|
|
Difficulty getting credentialed
|
20.1
|
20.0
|
.99
|
26.3
|
6.7
|
.09
|
|
Religious affiliation of the employing institution
|
18.2
|
8.6
|
.16
|
14.9
|
6.7
|
.39
|
|
Reimbursement issues
|
14.4
|
17.2
|
.69
|
13.2
|
0
|
.13
|
|
Noncompete clauses
|
19.5
|
20.0
|
.95
|
14.6
|
20.0
|
.61
|
|
Difficulties obtaining needed equipment
|
37.1
|
42.9
|
.53
|
29.8
|
26.7
|
.80
|
|
Lack of support staff training
|
53.5
|
62.8
|
.31
|
42.1
|
26.7
|
.25
|
|
Difficulty obtaining malpractice/liability insurance
|
16.3
|
14.3
|
.76
|
17.5
|
20.0
|
.81
|
|
Concern for family’s acceptance in the community
|
13.8
|
5.7
|
.19
|
15.8
|
6.7
|
.35
|
|
Limited time to integrate abortion
|
48.4
|
45.7
|
.77
|
37.7
|
46.7
|
.50
|
|
Lack of support network
|
33.3
|
34.3
|
.91
|
26.3
|
20.0
|
.60
|
|
Not a practice priority
|
49.1
|
54.3
|
.57
|
30.7
|
46.7
|
.21
|
This study revealed differences in postresidency abortion provision between URM and non-URM family physicians who received abortion training during residency. Despite similar training histories and intentions to provide abortions postresidency, URMs were significantly less likely to have provided any abortions in the past year and any procedural abortions postresidency compared to their non-URM colleagues. While other differences did not attain statistical significance, clinically relevant trends reflect that URMs also are less likely to provide abortions in general and medication abortions specifically after residency compared to their non-URM colleagues. Furthermore, this association held true in multivariate regression, strengthening the notion that physician race and ethnicity may have bearing on abortion provision.
Reported barriers to abortion provision did not adequately explain reasons for the discrepancies noted between URMs and non-URMs, but they did provide areas for further investigation. URM respondents reported significantly higher self-perceived inadequate medication abortion skills, despite training histories similar to non-URMs. Research demonstrating that URMs often experience a lack of or inadequate mentorship 24-26 may provide some insight into why URMs may have low self-efficacy in abortion provision. Additionally, while not statistically significant, URMs were more likely to report administrative, colleague, or staff resistance and difficulties arranging colleague support for complications. This finding may also be particularly relevant because a robust body of research has demonstrated that URMs experience significant racial and ethnic discrimination, including micro- and macroaggressions, during training and in the workplace. 27-29 Moreover, professional integration and feelings of belonging are lower among URMs in academia. 30, 31 These cumulative challenges may impact URM physicians’ negotiation of professional relationships, particularly in the already contentious sociopolitical context of abortion provision.
While URM respondents had notably lower rates of procedural abortion provision, this might be explained by their lower rates of having considered it or by the fact that a higher proportion of URM respondents stated that procedural abortion was not a practice priority. Yet the unique professional obstacles experienced by URMs may impede both consideration and provision of procedural abortion, which requires different technical skills, mentorship, clinical support, and negotiation of professional relationships 32 that are distinct from those needed for medication abortion provision. Moreover, the stigma and stress of providing abortion care, especially procedural abortion care, is well-documented. Abortion providers face harassment, increased burnout, threats to their safety, and social stigma in their communities. 33-35 These factors, in combination with the unique stressors and professional obstacles that URM physicians already face, may dissuade some from taking on the additional challenges that accompany procedural abortion provision.
Importantly, these data also demonstrated that respondents not associated with residency programs were less likely to provide abortion postresidency. This could be compounded by the fact that rates of URMs in academic medicine in general have increased only modestly over the past 4 decades and remain low at 7.7%, 9 likely due to inadequate recruitment and retention procedures. 36 Similarly, the significant lack of URMs in academic medicine contributes to a dearth of URM role models and mentors 24, 37, 38 who provide abortion and are often not available for URM trainees to emulate and learn from. Although we found no differences between the groups in our sample with respect to their residency associations, the known shortcomings of recruitment and retention of URMs in academic medicine may have implications for abortion provision by URM physicians.
Notably, data also revealed that respondents in the South and Midwest, where abortion restrictions are most common, were more likely to provide abortion than those in the Northeast and West. This may be because of the potential for saturation of abortion providers in the Northeast and West compared to the South and Midwest. In addition, respondents from the South and Midwest may be among few providers and are responding to the need for more abortion access in those regions. 23 However, the low numbers of respondents from these regions limit conclusions drawn from this data.
A higher (though not significantly so) proportion of URM respondents reported practicing in FQHCs. This finding was not surprising because URMs across primary care specialties are disproportionally likely to work in underserved communities, 10 and URMs are overrepresented in the federally funded National Health Service Corps, with a third of 2019 fellows categorized as URM. 39 While we initially thought that these differences, in combination with the Hyde Amendment’s prohibition on abortion care at federally funded sites, 40 might be contributing to the lower rates of abortion provision among URMs in our sample, our analysis suggested that this is unlikely. Working in an FQHC as one’s primary practice setting was not associated with any significant differences in abortion provision in bivariate analysis and did not improve the fit of the multivariate models. Although FQHCs can provide abortion services by separating out federal funding from other funding streams, 41 another possible explanation for the differences in postresidency employment settings might be considered. More early-career URM physicians overall may be placed in settings where abortion provision is restricted, and that factor may contribute to differences in the broader physician population.
Limitations
One limitation of the study is the moderately small sample size. In addition, the response rate was lower than ideal. As a result, the total study sample included low numbers of URMs. Notwithstanding, the proportion of URMs in this sample is consistent with national data about the percentage of family medicine residents who are URM. 11 Additionally, while the response rate was low, it was consistent with typical rates for physicians on online surveys. 42-44 Those in the sampling frame who provided abortion possibly were more likely to respond to the survey invitation, but we have little information on the nonresponders. We were not able to report differences between responders and nonresponders in gender, current geographic region, and URM status.
Finally, the reported barriers to abortion provision did not fully explain the differences in provision between URM and non-URM respondents. We believe that this is likely because professional barriers that are known to be more common among URMs (eg, experiences of professional racial and ethnic discrimination, inadequate mentorship, poor professional integration) were not explored in this study.
To our knowledge, this study is the first to explore differences in abortion provision between URM and non-URM family physicians. Factors such as inadequate mentorship, career-related racial and ethnic discrimination, and poor professional integration may compound the existing sociopolitical challenges of abortion provision. Measuring these factors with qualitative or mixed-methods approaches is needed to generate more knowledge about the specific barriers URMs face in abortion provision. However, the issue of racial and ethnic underrepresentation persists across medicine in general; to address this, family medicine colleagues have proposed and developed a variety of strategies. These include URM-focused mentorship and leadership development programs, 45, 46 targeted recruitment approaches, and programs that foster retention and professional integration with a focus on creating an institutional culture of antiracism. 36, 47, 48 Moreover, intentional efforts to develop URM leadership and shift power to effect institutional change have been proposed as methods of creating a more diverse workforce in medicine and elsewhere. 37, 38, 49 Many of these strategies could be employed to increase numbers of URMs in family medicine abortion provision in order to build a truly diverse workforce providing essential reproductive health services.
References
-
Saha S, Arbelaez JJ, Cooper LA. Patient-physician relationships and racial disparities in the quality of health care.
Am J Public Health. 2003;93(10):1,713-1,719. doi:
10.2105/AJPH.93.10.1713
-
-
Jetty A, Hyppolite J, Eden AR, Taylor MK, Jabbarpour Y. Underrepresented minority family physicians more likely to care for vulnerable populations.
J Am Board Fam Med. 2022;35(2):223-224.
doi:10.3122/jabfm.2022.02.210280
-
Silver JK, Bean AC, Slocum C, et al. Physician workforce disparities and patient care: a narrative review.
Health Equity. 2019;3(1):360-377.
doi:10.1089/heq.2019.0040
-
Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race.
Ann Intern Med. 2003;139(11):907-915.
doi:10.7326/0003-4819-139-11-200312020-00009
-
Takeshita J, Wang S, Loren AW, et al. Association of racial/ethnic and gender concordance between patients and physicians with patient experience ratings.
JAMA Netw Open. 2020;3(11):e2024583.
doi:10.1001/jamanetworkopen.2020.24583
-
Street RL Jr, O’Malley KJ, Cooper LA, Haidet P. Understanding concordance in patient-physician relationships: personal and ethnic dimensions of shared identity.
Ann Fam Med. 2008;6(3):198-205.
doi:10.1370/afm.821
-
Alsan, M, Garrick, O, Graziani, GC.
Does diversity matter for health? experimental evidence from Oakland. National Bureau of Economic Research working paper 24787. August 2019.
https://www.nber.org/papers/w24787
-
-
Xierali IM, Nivet MA. The racial and ethnic composition and distribution of primary care physicians.
J Health Care Poor Underserved. 2018;29(1):556-570.
doi:10.1353/hpu.2018.0036
-
Xierali IM, Hughes LS, Nivet MA, Bazemore AW. Family medicine residents: increasingly diverse, but lagging behind underrepresented minority population trends. Am Fam Physician. 2014;90(2):80-81.
-
Jerman J, Jones RK, Onda T. Characteristics of U.S. abortion patients in 2014 and changes since 2008. 2016. https://www.guttmacher.org/report/characteristics-us-abortion-patients-2014
-
Stulberg DB, Dude AM, Dahlquist I, Curlin FA. Abortion provision among practicing obstetrician-gynecologists.
Obstet Gynecol. 2011;118(3):609-614.
doi:10.1097/AOG.0b013e31822ad973
-
Brown KS, Steinauer JE, Turk J, Landy U, Jackson AV. Racial diversity in abortion education and intention to provide abortion in postresidency practice: data from the Ryan Program.
Am J Obstet Gynecol. 2020;222(3):271 e1-271 e8.
doi:10.1016/j.ajog.2019.09.009
-
Godfrey EM, Rubin SE, Smith EJ, Khare MM, Gold M. Women’s preference for receiving abortion in primary care settings.
J Womens Health (Larchmt). 2010;19(3):547-553.
doi:10.1089/jwh.2009.1454
-
Wu JP, Godfrey EM, Prine L, Andersen KL, MacNaughton H, Gold M. Women’s satisfaction with abortion care in academic family medicine centers. Fam Med. 2015;47(2):98-106.
-
Summit AK, Casey LM, Bennett AH, Karasz A, Gold M. “I don’t want to go anywhere else”: patient experiences of abortion in family medicine. Fam Med. 2016;48(1):30-34.
-
Summit AK, Gold M. The effects of abortion training on family medicine residents’ clinical experience. Fam Med. 2017;49(1):22-27.
-
Herbitter C, Greenberg M, Fletcher J, Query C, Dalby J, Gold M. Family planning training in US family medicine residencies. Fam Med. 2011;43(8):574-581.
-
Srinivasulu S, Maldonado L, Prine L, Rubin SE. Intention to provide abortion upon completing family medicine residency and subsequent abortion provision: a 5-year follow-up survey.
Contraception. 2019;100(3):188-192.
doi:10.1016/j.contraception.2019.05.011
-
Block A, Dehlendorf C, Biggs MA, McNeil S, Goodman S. Postgraduate experiences with an advanced reproductive health and abortion training and leadership program. Fam Med. 2017;49(9):706-713.
-
Goodman S, Shih G, Hawkins M, et al. A long-term evaluation of a required reproductive health training rotation with opt-out provisions for family medicine residents. Fam Med. 2013;45(3):180-186.
-
Summit A, Gold M. Abortion provision by family physicians after integrated opt-out training in residency.
Fam Med. Published online 2023.
doi: 10.22454/FamMed.2023.526561
-
Rodríguez JE, Campbell KM, Mouratidis RW. Where are the rest of us? Improving representation of minority faculty in academic medicine.
South Med J. 2014;107(12):739-744.
doi:10.14423/SMJ.0000000000000204
-
Beech BM, Calles-Escandon J, Hairston KG, Langdon SE, Latham-Sadler BA, Bell RA. Mentoring programs for underrepresented minority faculty in academic medical centers: a systematic review of the literature.
Acad Med. 2013;88(4):541-549.
doi:10.1097/ACM.0b013e31828589e3
-
Carvajal D, L. R. Factors associated with the imposter syndrome among family medicine faculty.
Annals of Family Medicine. 2022;20(Sup 1)2,677.
doi: 10.1370/afm.20.s1.2677
-
Zambrana RE, Harvey Wingfield A, Lapeyrouse LM, et al. Blatant, subtle, and insidious: URM faculty perceptions of discriminatory practices in predominantly White institutions.
Sociol Inq. 2017;87(2):207-232.
doi:10.1111/soin.12147
-
Campbell KM. The diversity efforts disparity in academic medicine.
Int J Environ Res Public Health. 2021;18(9):4,529.
doi:10.3390/ijerph18094529
-
Rodríguez JE, Campbell KM, Pololi LH. Addressing disparities in academic medicine: what of the minority tax?
BMC Med Educ. 2015;15(1):6.
doi:10.1186/s12909-015-0290-9
-
Forrester A. Why I stay—The other side of underrepresentation in academia.
N Engl J Med. 2020;383(4):e24.
doi:10.1056/NEJMpv2022100
-
Walters K, Maliszewski Lukszo C, Evans-Campbell T, Burciaga Valdez R, Zambrana R. ‘Before they kill my spirit entirely’: insights into the lived experiences of American Indian Alaska Native faculty at research universities.
Race Ethn Educ. 2019;22(5):610-633.
doi:10.1080/13613324.2019.1579182
-
Summit AK, Lague I, Dettmann M, Gold M. Barriers to and enablers of abortion provision for family physicians trained in abortion during residency.
Perspect Sex Reprod Health. 2020;52(3):151-159.
doi:10.1363/psrh.12154
-
Freedman L.
Willing and Unable: Doctors’ Constraints in Abortion Care. Vanderbilt University Press; 2010.
doi:10.2307/j.ctv17vf79f
-
Harris LH, Debbink M, Martin L, Hassinger J. Dynamics of stigma in abortion work: findings from a pilot study of the Providers Share Workshop.
Soc Sci Med. 2011;73(7):1062-1070.
doi:10.1016/j.socscimed.2011.07.004
-
-
Emery CR, Boatright D, Culbreath K. Stat! An action plan for replacing the broken system of recruitment and retention of underrepresented minorities in medicine. September 2018.
NAM Perspectives.
doi: 10.31478/201809a
-
Campbell KM, Hudson BD, Tumin D. Releasing the net to promote minority faculty success in academic medicine.
J Racial Ethn Health Disparities. 2020;7(2):202-206.
doi:10.1007/s40615-020-00703-z
-
Campbell KM, Rodríguez JE. Addressing the minority tax: perspectives from two diversity leaders on building minority faculty success in academic medicine.
Acad Med. 2019;94(12):1854-1857.
doi:10.1097/ACM.0000000000002839
-
-
-
-
Barnhart BJ, Reddy SG, Arnold GK. Remind me again: physician response to web surveys: the effect of email reminders across 11 opinion survey efforts at the American Board of Internal Medicine from 2017 to 2019.
Eval Health Prof. 2021;44(3):245-259.
doi:10.1177/01632787211019445
-
Cunningham CT, Quan H, Hemmelgarn B, et al. Exploring physician specialist response rates to web-based surveys.
BMC Med Res Methodol. 2015;15(1):32.
doi:10.1186/s12874-015-0016-z
-
Matteson KA, Anderson BL, Pinto SB, Lopes V, Schulkin J, Clark MA. Surveying ourselves: examining the use of a web-based approach for a physician survey.
Eval Health Prof. 2011;34(4):448-463.
doi:10.1177/0163278710391086
-
Coe C, Piggott C, Davis A, et al. Leadership pathways in academic family medicine: focus on underrepresented minorities and women.
Fam Med. 2020;52(2):104-111.
doi:10.22454/FamMed.2020.545847
-
Robles J, Anim T, Wusu MH, et al. An approach to faculty development for underrepresented minorities in medicine.
South Med J. 2021;114(9):579-582.
doi:10.14423/SMJ.0000000000001290
-
Kalet A, Libby AM, Jagsi R, et al. Mentoring underrepresented minority physician-scientists to success.
Acad Med. 2022;97(4):497-502.
doi:10.1097/ACM.0000000000004402
-
Amaechi O, Foster KE, Tumin D, Campbell KM. Addressing the gate blocking of minority faculty.
J Natl Med Assoc. 2021;113(5):517-521.
doi:10.1016/j.jnma.2021.04.002
-
Foster KE, Johnson CN, Carvajal DN, et al. Dear White people.
Ann Fam Med. 2021;19(1):66-69.
doi:10.1370/afm.2634



There are no comments for this article.