Background and Objectives: Only 20% of family physicians report providing long-acting reversible contraception (LARC). Clinician-related barriers include confidence and comfort with LARC counseling and insertion/removal, and limited availability and uptake. Training during residency may address barriers and increase access/availability of LARC to support reproductive autonomy. We sought to determine the impact of block scheduling LARC clinics on resident comfort and confidence with LARC counseling and insertion/removal.
Methods: LARC block schedules were established in a Midwest family medicine residency’s primary clinic (FMC) and in a federally qualified health center rotation clinic. Baseline and end-of-study surveys, compared by Mann-Whitney U and Wilcoxon signed-rank tests, were used to assess comfort and confidence with counseling and inserting LARC. The number of LARC devices placed at the FMC were collected for the intervention year and the year prior.
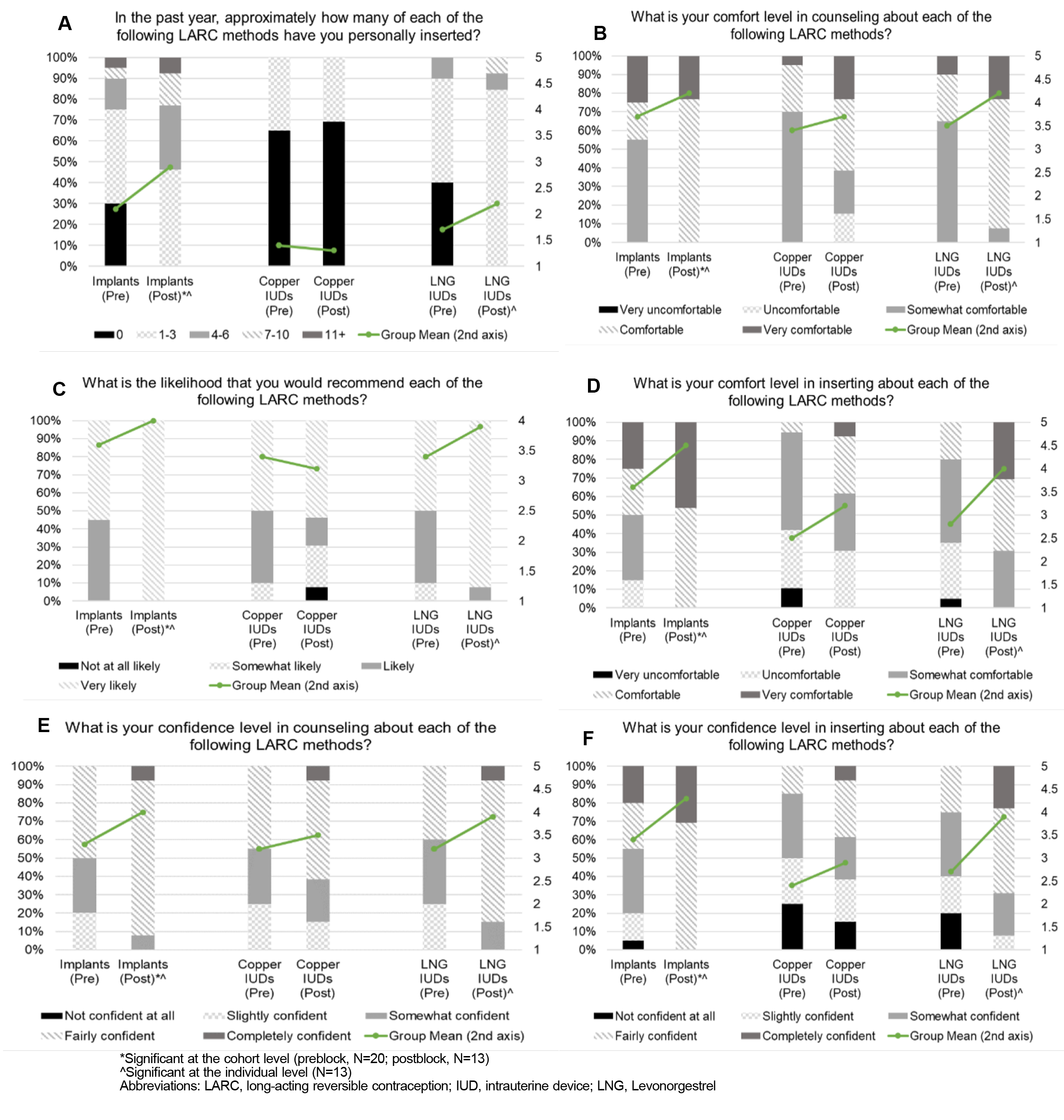
Results: Twenty of 30 residents completed the baseline survey; 13 completed the end-of-study survey. At the group and individual levels, comfort increased for counseling on Levonorgestrel (LNG) intrauterine devices (IUDs) and for inserting implants and LNG IUDs. Individual comfort increased for copper IUDs. Resident willingness to recommend LARC increased, and more devices were placed during the intervention year than the year prior in the FMC (all: P<.05).
Conclusions: Block scheduling of LARC clinics was associated with increased residents’ comfort and confidence with counseling and placement of implants (LNG IUDs) and with an increase in LARCs placed at one clinic. Changes to scheduling may be an effective educational strategy that may increase access/availability to LARC.
The rate of unintended pregnancy in the United States is 45%, and risks of morbidity and mortality through delayed/missed prenatal care and reproductive autonomy limitations are of concern. 1-5 One underused option for women is long-acting reversible contraception (LARCs), including contraceptive implants (or implants, hereafter), copper intrauterine devices [IUDs], and Levonorgestrel IUDs (LNGs), as an effective option to prevent unintended pregnancy. 6-8 While LARCs are effective, only 10.4% of women who use contraception report using LARCs. 9 Clinician-related barriers include lack of education and hands-on training; comprehensive training for health care professionals is needed to increase LARC accessibility/availability. 10-12
Family physicians (FPs) can lead efforts to prevent unintended pregnancy by counseling about and providing LARCs. Approximately 20% of US FPs place LARCs, while 82% report providing women’s health services. 13 Increasing LARC access through FPs may begin in residency. Family medicine (FM) residents reported less comfort in providing counseling and inserting LARCs (18-47%) compared to obstetrics/gynecology (OB/Gyn) residents (83-86%). 14 FM residents desire education and training about contraceptive care, 15 and that training leads to increased access/availability of contraceptive services in their future practices. 16, 17
Block scheduling (ie, designating clinic time for specific activities) has been reported to be effective for separating residents’ didactic and clinical activities 18, 19 as well as for guaranteed preceptor supervision. This study explored whether block scheduling of LARC clinics within an FM residency led to changes in (1) comfort with and confidence in LARC counseling and placement, and (2) number of LARC devices placed.
LARC Block Clinics
This study was performed in a single Midwestern FM residency program (30 residents) between July 1, 2019, and June 30, 2020, at two clinical sites (one FMC and one federally qualified health center rotation clinic [FQHC]). Prior to the intervention, lack of preceptor availability sometimes prevented residents from performing LARC procedures. Block scheduling ensured that a trained preceptor was guaranteed to be available. During the intervention period, one half-day (FMC) and two half-day (FQHC) LARC block clinics were held each month with a dedicated preceptor. All LARC-related appointments (eg, insertion and removal procedures), including residents’ continuity patients, were offered during the blocks.
Data Collection and LARC Training
Residents were invited to complete an online survey about LARC in July 2019 (pre, beginning of academic year) and June 2020 (post, end of academic year). Thirteen questions addressed training; comfort and confidence with counseling and placement; and approximate number of LARCs placed in the past year. The number of devices placed at FMC was recorded for the year preceding and during the intervention, but similar data was not available for FQHC. The American Academy of Family Physicians Institutional Review Board approved the study under exempt category 2.
Standard LARC didactic training was not modified during the study. All residents participated in a procedure workshop on IUD counseling and insertion/removal as well as in sponsored implant insertion/removal training by one certified faculty trainer. In addition to procedures, training addressed informed consent, patient autonomy, alternative contraception, and side effects of LARCs.
Statistical Analyses
We performed group- and individual-level analyses. We used proportions tests to compare pre/post demographics and number of LARC devices placed. We used Mann-Whitney U tests to compare groups for nonpaired analyses. We used Wilcoxon signed-rank tests to compare the same resident at the beginning and the end for paired analyses. Analyses were completed using SPSS 25 (IBM; α=0.05).
Group Demographics
Twenty of 30 (67%) program residents completed the baseline survey, and 13 (43%) completed the postsurvey (Table 1). No significant changes in the demographics occurred between the baseline survey and the end of the LARC training.
|
Resident demographics
|
|
|
Baseline (N=20)
|
Posttraining (N=13)
|
Nonresponders (N=10)
|
|
|
n (%)
|
n (%)
|
n (%)
|
|
Gender
|
|
Male
|
5 (25.0)
|
3 (23.1)
|
5 (50.0)
|
|
Female
|
15 (75.0)
|
10 (76.9)
|
5 (50.0)
|
|
Age (years)
|
|
26-30
|
8 (40.0)
|
5 (38.5)
|
Unknown
|
|
31-35
|
9 (45.0)
|
7 (53.8)
|
Unknown
|
|
36-40
|
3 (15.0)
|
1 (7.7)
|
Unknown
|
|
Program year
|
|
Year 1
|
9 (45.0)
|
6 (46.2)
|
1 (10.0)
|
|
Year 2
|
7 (35.0)
|
4 (30.8)
|
3 (30.0)
|
|
Year 3
|
4 (20.0)
|
3 (23.1)
|
6 (60.0)
|
|
Devices placed (FMC only; includes placement by faculty)
|
|
Device type
|
July 2018–June 2019 (N=59)
|
July 2019–June 2020 (N=128)
|
Significance
|
|
Implants
|
27
|
59
|
<.001*
|
|
Copper IUDs
|
9
|
11
|
.824
|
|
LNG IUDs
|
23
|
58
|
<.001*
|
Device Placement and LARC Recommendation
For group self-reported placement, implants (P=.040) placed increased over the study period but not LNGs; while for individuals, implant (P=.011) and LNG (P=.020) placements increased (Figure 1A). FMC clinic-level device numbers (including faculty and resident placements) indicated significantly more implants and LNGs placed during the study (both P<.001;).
Postintervention, residents indicated that they were more likely to recommend implants (P=.030) and LNGs at the group (P=.040) and individual (P=.005; Figures 1B and 1C) levels.
Comfort and Confidence Changes Over Time
Comfort in counseling for LNGs increased for the group (P=.006) and individuals (P=.033). Comfort in inserting implants and LNGs also increased for the group (P=.020; P=.001, respectively) and individuals (P=.022, P=.004, respectively). Comfort in inserting copper IUDs, however, increased only for individuals (P=.046). Confidence in counseling for implants and LNGs increased for the group (P=.022, P=.013, respectively) and individuals (P=.030, P=.015, respectively). Finally, confidence in inserting implants and LNGs increased for the group (P=.020, P=.001, respectively) and individuals (P=.005, P=.004, respectively; Figures 1D, 1E, 1F).
High-quality, safe contraceptive management is part of full-spectrum comprehensive care. Most FPs reported providing women’s health services, but a minority reported providing LARCs. 13 Lack of LARC availability has been linked to a shortage of trained clinicians. 10, 11, 12 Like their OB/Gyn peers, FPs must be provided exposure to and opportunities for LARC training during residency. Interventions in residencies demonstrated that LARC education led to both improved comfort with LARCs and increased access/availability for patients. 14, 16, 17 We examined the effect of block scheduling LARC procedure clinics to provide residents with opportunities to place/remove LARCs.
Residents self-reported inserting more LARCs and having increased comfort and confidence, indicating that block scheduling may have increased opportunities for residents to perform LARC procedures. 18, 19 Residents indicated that they were more likely to recommend implants and LNGs postblock scheduling. These findings indicate that block scheduling for LARC during residency may not only lead to increased access/availability for patients during residency but also in the residents’ future practices. 20-22 Our subjective findings are consistent with previous literature showing increased education and access/availability leading to more LARC placement. 14, 16, 17
Limitations
Small sample size and attrition (due to graduating residents) limit generalizability of these findings. LARC devices placed at the FMC may reflect devices placed by attending physicians in addition to residents, and no device number data was available from FQHC. These gaps prevent assessing the number of resident device placements during the block scheduling and the impact on accessibility/availability of LARCs to residents’ patients. However, our findings establish an important premise on which to base hypotheses for larger-scale investigations. Unfortunately, we did not ask specifically about LARC removals, although residents were trained in LARC removal procedures, which also occurred during the blocks. The COVID-19 pandemic affected the intervention; however, we still noted the improvement in training outcomes and increases in LARC device placement. Outcomes would have been expected to be negatively impacted by lockdowns limiting in-person delivery of care.
In a single residency with residents rotating at two clinical sites, we demonstrated that block scheduling LARC procedures increased residents’ self-reported LARC exposure and their comfort and confidence in counseling and inserting implants and LNGs. One clinical site saw a significant increase in LARC placements. Shifts in clinical scheduling structure in residencies may increase LARC hands-on training for residents, potentially leading to an increase in FPs offering LARC in practice and, ultimately, to increased LARC access for women cared for by FPs.
References
-
Aztlan-James EA, McLemore M, Taylor D. Multiple unintended pregnancies in U.S. women: a systematic review.
Women's Health Issues. 2017;27(4):407-413.
doi: 10.1016/j.whi.2017.02.002
-
Gipson JD, Koenig MA, Hindin MJ. The effects of unintended pregnancy on infant, child, and parental health: a review of the literature.
Stud Fam Plann. 2008;39(1):18-38.
doi:10.1111/j.1728-4465.2008.00148.x
-
Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. Selected Practice Recommendations for Contraceptive Use. Centers for Disease Control and Prevention; 2016.
-
-
Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008-2011.
N Engl J Med. 2016;374(9):843-852.
doi:10.1056/NEJMsa1506575
-
Harper CC, Rocca CH, Thompson KM, et al. Reductions in pregnancy rates in the USA with long-acting reversible contraception: a cluster randomised trial. Lancet. 2015;386(9993):562-568. doi:10.1016/S0140-6736(14)62460-0
-
Prescott GM, Matthews CM. Long-acting reversible contraception: a review in special populations.
Pharmacotherapy. 2014;34(1):46-59.
doi:10.1002/phar.1358
-
Bahamondes L, Fernandes A, Monteiro I, Bahamondes MV. Long-acting reversible contraceptive (LARCs) methods.
Best Pract Res Clin Obstet Gynaecol. 2020;66:28-40.
doi:10.1016/j.bpobgyn.2019.12.002
-
-
Phillips J, Sandhu P. Barriers to implementation of long-acting reversible contraception: A systematic review.
J Am Assoc Nurse Pract. 2018;30(4):236-243.
doi:10.1097/JXX.0000000000000019
-
Potter J, Santelli JS. Contraceptive counseling for adolescents.
Womens Health (Lond Engl). 2015;11(6):737-741.
doi:10.2217/whe.15.75
-
Britton A, Connolly A. Long-acting reversible methods of contraception: unified training.
J Fam Plann Reprod Health Care. 2014;40(2):80-81.
doi:10.1136/jfprhc-2013-100792
-
Chelvakumar M, Jabbarpour Y, Coffman M, Jetty A, Glazer Shaw J. Long-acting reversible contraception (LARC) provision by family physicians: low but on the rise.
J Am Board Fam Med. 2019;32(1):10-12.
doi:10.3122/jabfm.2019.01.180215
-
Davis SA, Braykov NP, Lathrop E, Haddad LB. Familiarity with long-acting reversible contraceptives among obstetrics and gynecology, family medicine, and pediatrics residents: results of a 2015 national survey and implications for contraceptive provision for adolescents.
J Pediatr Adolesc Gynecol. 2018;31(1):40-44.
doi:10.1016/j.jpag.2017.09.007
-
-
-
Pace LE, Dolan BM, Tishler LW, Gooding HC, Bartz D. Incorporating long-acting reversible contraception into primary care: a training and practice innovation.
Women's Health Issues. 2016;26(2):131-134.
doi: 10.1016/j.whi.2015.09.004
-
Bordley J, Agustin AG, Ahmed MA, et al. Restoration of resident sleep and wellness with block scheduling.
Med Educ. 2017;51(12):1,241-1,249.
doi:10.1111/medu.13392
-
DeWaters AL, Loria H, Mayo H, Chisty A, Nguyen OK. The impact of block ambulatory scheduling on internal medicine residencies: a systematic review.
J Gen Intern Med. 2019;34(5):731-739.
doi:10.1007/s11606-019-04887-x
-
Harper CC, Blum M, de Bocanegra HT, et al. Challenges in translating evidence to practice: the provision of intrauterine contraception.
Obstet Gynecol. 2008;111(6):1,359-1,369.
doi:10.1097/AOG.0b013e318173fd83
-
Coutinho AJ, Levin Z, Petterson S, Phillips RL Jr, Peterson LE. Residency program characteristics and individual physician practice characteristics associated with family physician scope of practice.
Acad Med. 2019;94(10):1,561-1,566.
doi:10.1097/ACM.0000000000002838
-
Phillips RL Jr, Holmboe ES, Bazemore AW, George BC. Purposeful imprinting in graduate medical education: opportunities for partnership. Fam Med. 2021;53(7):574-577. doi:10.22454/FamMed.2021.264013



There are no comments for this article.