Background and Objectives: Previous research has described a waning interest among third-year students to employ empathetic practice along with decreased opportunity to develop empathic communication skills. In this study we sought to address this decline using the skill of noticing (ie, the capacity to attune to specific aspects of practice and interactions) as an intervention for third-year medical students.
Methods: We designed a qualitative study to address the following research question: How can a focused noticing tool encourage empathetic moments during the patient interview for third-year medical students? Eight third-year medical students used the Social Emotional Noticing Tool (SENT) during their 4-week family medicine rotation, then joined a focus group to share their experiences with SENT and articulate barriers and opportunities toward practicing empathy during clerkship.
Results: Student participants (a) described using the tool, including barriers and opportunities; (b) made connections between the practice of noticing using SENT and enacting empathy; and (c) emphasized how enacting empathy in their third year is largely influenced by interactions with clinical faculty.
Conclusions: The use of SENT helped students notice empathy or lack thereof. However, making connections between individual capacity for empathic interactions and the impact of positive or negative role models is necessary. Based on our findings, we encourage the need for shared responsibility among students, faculty and preceptors, and organizations.
The reported empathy decline of third-year medical students underlines a critical issue in the clerkship years: a waning interest among third-year students to employ empathetic practice along with decreased opportunity to develop empathic communication skills. 1-4 In this study we sought to address this decline using the skill of noticing as an intervention for third-year medical students. “Noticing” in this context is defined as the capacity to attune to specific aspects of practice and interactions.5, 6 By noticing patient clues, doctors are more engaged with and better able to care for patients.7 Other studies focused on empathy decline have largely been quantitative studies and self-reports.8-10 This qualitative study addressed the following question: How can a focused noticing tool encourage empathetic moments during the patient interview for third-year medical students?
This study took place during family medicine rotations for 170 third-year clerkship students at Michigan State University’s College of Human Medicine (MSUCHM). As a community-based medical school, students are assigned to campuses and clinical settings across the state of Michigan. Family medicine is one of the largest and most popular specialties at MSUCHM, providing an important and pivotal rotation for many students.
After receiving Institutional Review Board approval from Michigan State University, we emailed 170 third-year students to participate in the study through two rounds of recruitment. Eight students accepted and participated in a focus group. 11
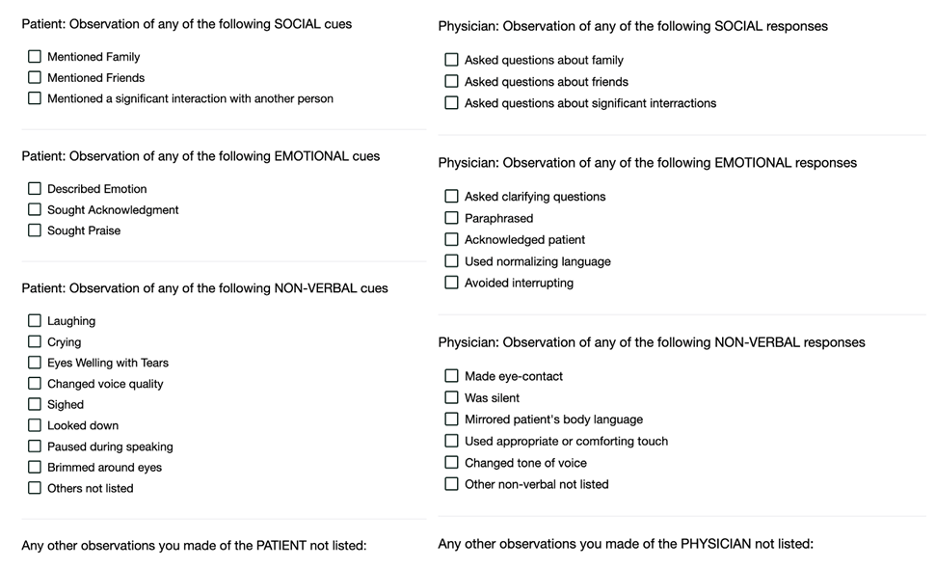
We developed a tool that could be used to support medical students’ skill of noticing by reviewing 23 articles on patient-physician interactions and empathetic communication as well as incorporating some worksheets and resources from Michigan State University (Table 1). We piloted the Social Emotional Noticing Tool (SENT) with the second author (MT), who was a second-year medical student at the time. SENT is intended to be used as a mechanism to support the skill of noticing and is not a measurement survey; therefore, we did not include a phase of validation for SENT.
|
Research article/source
|
Clues, words, behaviors
|
|
Suchman, Markakis, Beckman, Frankel (1997) 12
|
Praise opportunities Description of emotion Expression of emotion
|
|
Levinson, Gorawara-Bhat, Lamb (2000) 13
|
Mention of family Seeking acknowledgment Cries for help
|
|
Matthews, Suchman, Branch (1993) 14
|
Changes in voice quality Sigh Pauses Brimming of the eyes
|
|
Fortin (2019) 15
|
Patient-centered interviewing Silence Mirror patient body language NURS (naming, understanding, respecting, supporting)
|
|
Shapiro (2002) 16
|
Deep listening “Stay closer to the patient’s heart than to their face” Physician posture Being fully present Respect Nonjudgment Taking patient seriously
|
|
Roter, Hall (2006) 17
|
Gazing at patient Nonverbal emotion expressions
|
|
Arwheiler, Neumann, Goldblatt, Hahn, Scheffer (2014) 18
|
Recognizing psychosocial dimensions of care
|
|
Batt-Rawden, Chisolm, Flickinger (2013) 19
|
Patient-centered interviewing
|
|
Benbasset, Baumal (2004) 20
|
Patient-centered interviewing
|
|
Epstein (2003) 21
|
Habits of mind Mindful practices
|
|
Hale, Freed, Ricotta, Farris, Smith (2017) 22
|
Body language
|
|
Ishikawa, Hashimoto, Kinoshita, Yano (2010) 23
|
Nonverbal communication
|
|
Hsu, Saha, Korthuis et al (2012) 24
|
Dismissive Elicit more information Expressions of annoyance Talk about personal life
|
|
Larson (2005) 25
|
Parallel emotions
|
|
Levine, Ambady (2013) 26
|
Sitting close Nodding Making eye contact Open or closed body posture Exhibiting facial expressions
|
|
Lim, Moriarty, Huthwaite (2011) 27
|
Role modeling
|
|
Lorie, Reinero, Phillips, Zhang, Riess (2017) 28
|
Culture-based nonverbal expressions
|
|
Mast (2007) 29
|
Nonverbal
|
|
Molinuevo, Escorihuela, Fernández-Teruel, Tobeña, Torrubia (2011) 30
|
Patient-centered perspective Nonverbal emotion or expressions
|
|
Riess, Kraft-Todd (2014) 31
|
E.M.P.A.T.H.Y. (eye contact, muscles of facial expression, posture, affect, tone of voice, hearing the whole patient, your response)
|
|
Silvester, Patterson, Koczwara, Ferguson (2007) 32
|
Trust Open communication
|
|
Squier (1990) 33
|
Helping behaviors Facial expressions Tone of voice
|
|
Weissmann, Branch, Gracey, Haidet, Frankel (2006) 34
|
Role modeling
|
|
4-Cs*
|
Character, competence, connection, culture
|
|
SHARE*
|
Seek, help, assess, reach, evaluate
|
After observing a patient-physician interaction, students accessed SENT on their phones via Desire2Learn to make notations (Figure 1). Eight student participants completed SENT a minimum of six times during their 4-week family medicine rotation.
After all participants completed their family medicine rotation, they joined a focus group on Zoom. The focus group lasted approximately 75 minutes. The focus group was transcribed and then analyzed using an inductive and deductive coding schema.35, 36 Twenty-six independent codes were applied to the full transcript and then combined into three larger themes to produce final findings (Table 2).
|
Major
theme
|
Number
of responses,
n
(%)
|
|
Using the tool
|
11 (26)
|
|
Making connections
|
14 (34)
|
|
Reflecting on structural challenges
|
16 (39)
|
Our qualitative design offered students an opportunity to share more than just their experiences with SENT. It also offered them a chance to articulate barriers and opportunities.
Using the Tool
Participants described the benefits and barriers to using SENT. The benefits included increasing their ability to notice small moments and make noticing a habit. “The more I used it, I got to where I would notice. As time went on, I thought about it more just kind of naturally.” Students also expressed barriers. “I think one of the things I struggled with was trying to be present and engaging in the encounter while also observing and trying to check off these different behaviors.” Other participants noted the challenge of finding time to notice and use SENT.
Making Connections
Participants expressed how using SENT aided their ability to make connections between noticing and being empathetic. One participant shared, “I think I was trying to find more time to notice little things, things you might not pick up on . . . noticing those little subtle changes.” Noticing subtle changes helped some students also take more notice of how they were feeling. “At the end of the day, I would collect my thoughts and reflect on all of those encounters.” Taking these moments to reflect also exposed tensions—feeling the need to make change toward improving oneself. “I think it would be a good tool for students to use to recognize areas that they could improve, but that doesn’t mean that they’re going to put in the time.” One participant commented how SENT made her feel more aware of her failures as she strove to have empathetic interactions.
Reflecting on Structural Challenges
SENT supported students in identifying how other people or organizational cultures shaped empathy. “I think they’re [role models] critical. And I think that the lack of role models plays a huge part in it.” Another participant expressed this same sentiment, sharing, “I 100% agree. If I had to pick one thing over and over again, the role of our preceptors is absolutely the biggest.” All participants emphasized the power of seeing faculty demonstrate empathy, sharing that these enactments were perhaps the most valuable aspect in learning. “I just keep finding myself referring back to that positive role model and what they emulated during periods where I would struggle to empathize as much.”
Other participants shared the larger structural challenges of enacting empathy. “In some rotations you’re frowned upon for actually caring for the patient, and it almost like impacts you negatively with your reviews.” Additionally, participants identified feeling burnout and the decline of their own empathy, but also feeling uncertain about how to address their perceived decline. “Is it [the tool] helpful? It’s definitely helpful, but I’m not always hopeful about it. I’m not always hopeful that it’s going to make a huge difference. And I think those positive patient interactions that stick with you are critical.”
This study illuminated that teaching and learning in medical education is a dynamic process where both the learner and instructor play important roles.37 Although we initially focused on the specific practice of noticing, use of SENT highlighted much larger structural challenges. SENT aided students in identifying what was missing during the patient-physician encounter but did not provide any recommendations on what to do to fill these missing components of empathy—as one student stated, “helpful, but not hopeful.” This student’s comment emphasizes the need to investigate the mutual relationships, mentorship, and faculty interactions of teaching in clinical settings to deepen empathy.
Limitations also were present in our study. First, we struggled to recruit participants. From a cohort of 170, only eight students engaged over the entire duration of their family medicine rotation and the final focus group. Second, SENT was limited as a reflective and qualitative tool to engage in empathy. The routine use of SENT may in future studies be modified to be more reflective for students. Future iterations could include reflections on peer learning as a facilitator or barrier to empathy. Finally, although the SENT tool was primarily developed to enhance the skill of noticing, it also risked becoming a burden for participants and just another task to complete.
Supporting medical students’ display of empathy during clerkship years involves their own capacity and willingness to engage, and their capacity and willingness to demonstrate empathy toward those around them. 32, 38 Based on our findings, we encourage the need for shared responsibility among students, faculty and preceptors, and organizations. Continued qualitative examinations of empathy in third-year medical students also may deepen insights into why changes in empathy occur and how other factors (eg, relationships and school culture) shape the increase or decline of empathy.
This study was conducted through the generous support of the Blue Cross Blue Shield Foundation of Michigan.
The Generalist in Medical Education, November 11, 2023, Nashville, TN
Acknowledgments
The authors thank the students who so generously gave their time to participate in this study. The authors also thank Randi Stanulis, PhD, for early intellectual support of this study.
References
-
-
Neumann M, Edelhäuser F, Tauschel D, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents.
Acad Med. 2011;86(8):996-1009.
doi:10.1097/ACM.0b013e318221e615
-
Batt-Rawden SA, Chisolm MS, Anton B, Flickinger TE. Teaching empathy to medical students: an updated, systematic review.
Acad Med. 2013;88(8):1,171-1,177.
doi:10.1097/ACM.0b013e318299f3e3
-
Fields SK, Mahan P, Tillman P, Harris J, Maxwell K, Hojat M. Measuring empathy in healthcare profession students using the Jefferson Scale of Physician Empathy: health provider—student version.
J Interprof Care. 2011;25(4):287-293.
doi:10.3109/13561820.2011.566648
-
-
van Es EA. A framework for learning to notice student thinking. In: Sherin M, Jacobs V, Philipp R, eds. Mathematics Teacher Noticing: Seeing through Teachers’ Eyes. Routledge; 2011:164-181.
-
Raia F, Smith MS. Practitioners’ noticing and know-how in multi-activity practice of patient care and teaching and learning.
Cogn Instr. 2020;38(4):445-473.
doi:10.1080/07370008.2020.1782411
-
Chen D, Lew R, Hershman W, Orlander J. A cross-sectional measurement of medical student empathy.
J Gen Intern Med. 2007;22(10):1,434-1,438.
doi:10.1007/s11606-007-0298-x
-
Hojat M, Axelrod D, Spandorfer J, Mangione S. Enhancing and sustaining empathy in medical students.
Med Teach. 2013;35(12):996-1,001.
doi:10.3109/0142159X.2013.802300
-
-
Hall JN. Focus Groups: Culturally Responsive Approaches for Qualitative Inquiry and Program Evaluation. Myers Education Press; 2020.
-
-
Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings.
JAMA. 2000;284(8):1,021-1,027.
doi:10.1001/jama.284.8.1021
-
-
Fortin AH. Smith’s Patient Centered Interviewing: An Evidence-Based Method. 4th ed. McGraw-Hill Education; 2019.
-
-
Roter DL, Hall JA. Doctors Talking With Patients/Patients Talking With Doctors: Improving Communication in Medical Visits. 2nd ed. Praeger; 2006.
-
Batt-Rawden SA, Chisolm MS, Anton B, Flickinger TE. Teaching empathy to medical students: an updated, systematic review.
Acad Med. 2013;88(8):1,171-1,177.
doi:10.1097/ACM.0b013e318299f3e3
-
-
Epstein RM. Mindful practice in action (II): cultivating habits of mind.
Fam Syst Health. 2003;21(1):11-17.
doi:10.1037/h0089495
-
-
Ishikawa H, Hashimoto H, Kinoshita M, Yano E. Can nonverbal communication skills be taught?
Med Teach. 2010;32(10):860-863.
doi:10.3109/01421591003728211
-
Hsu I, Saha S, Korthuis PT, et al. Providing support to patients in emotional encounters: a new perspective on missed empathic opportunities.
Patient Educ Couns. 2012;88(3):436-442.
doi:10.1016/j.pec.2012.06.015
-
Larson EB, Yao X. Clinical empathy as emotional labor in the patient-physician relationship.
JAMA. 2005;293(9):1,100-1,106.
doi:10.1001/jama.293.9.1100
-
Levine CS, Ambady N. The role of non-verbal behaviour in racial disparities in health care: implications and solutions.
Med Educ. 2013;47(9):867-876.
doi:10.1111/medu.12216
-
-
Lorié Á, Reinero DA, Phillips M, Zhang L, Riess H. Culture and nonverbal expressions of empathy in clinical settings: A systematic review.
Patient Educ Couns. 2017;100(3):411-424.
doi:10.1016/j.pec.2016.09.018
-
Mast MS. On the importance of nonverbal communication in the physician-patient interaction.
Patient Educ Couns. 2007;67(3):315-318.
doi:10.1016/j.pec.2007.03.005
-
Molinuevo B, Escorihuela RM, Fernández-Teruel A, Tobeña A, Torrubia R. How we train undergraduate medical students in decoding patients’ nonverbal clues.
Med Teach. 2011;33(10):804-807.
doi:10.3109/0142159X.2011.588737
-
Riess H, Kraft-Todd G. E.M.P.A.T.H.Y.: a tool to enhance nonverbal communication between clinicians and their patients.
Acad Med. 2014;89(8):1,108-1,112.
doi:10.1097/ACM.0000000000000287
-
Silvester J, Patterson F, Koczwara A, Ferguson E. “Trust me...”: psychological and behavioral predictors of perceived physician empathy.
J Appl Psychol. 2007;92(2):519-527.
doi:10.1037/0021-9010.92.2.519
-
Squier RW. A model of empathic understanding and adherence to treatment regimens in practitioner-patient relationships.
Soc Sci Med. 1990;30(3):325-339.
doi:10.1016/0277-9536(90)90188-X
-
Weissmann PF, Branch WT, Gracey CF, Haidet P, Frankel RM. Role modeling humanistic behavior: learning bedside manner from the experts.
Acad Med. 2006;81(7):661-667.
doi:10.1097/01.ACM.0000232423.81299.fe
-
Hale AJ, Freed J, Ricotta D, Farris G, Smith CC. Twelve tips for effective body language for medical educators. Med Teach. 2017;39(9):914-919. doi:10.1080/0142159X.2017.1324140
-
Saldaña J. The Coding Manual for Qualitative Researchers. 3rd ed. SAGE; 2016.
-
Miles MB, Huberman AM, Saldaña J. Qualitative Data Analysis: A Methods Sourcebook. 3rd ed. SAGE; 2014.
-
-
Chaitoff A, Sun B, Windover A, et al. Associations between physician empathy, physician characteristics, and standardized measures of patient experience.
Acad Med. 2017;92(10):1,464-1,471.
doi:10.1097/ACM.0000000000001671



There are no comments for this article.