Continuity of care has been an identifying characteristic of family medicine since its inception and is an essential ingredient for high-functioning health care teams. Many benefits, including the quadruple aim of enhancing patient experience, improving population health, reducing costs, and improving care team well-being, are ascribed to continuity of care. In 2023, the Accreditation Council for Graduate Medical Education (ACGME) added two new continuity requirements—annual patient-sided continuity and annual resident-sided continuity—in family medicine training programs.
This article reviews continuity of care as it applies to family medicine training programs. We discuss the various types of continuity and issues surrounding the measurement of continuity. A generally agreed upon definition of patient-sided and resident-sided continuity is presented to allow programs to begin to collect the necessary data. Especially within resident training programs, intricacies associated with maintaining continuity of care, such as empanelment, resident turnover, and scheduling, are discussed. The importance of right-sizing resident panels is highlighted, and a mechanism for accomplishing this is presented.
The recent ACGME requirements represent a cultural shift from measuring resident experience based on volume to measuring resident continuity. This cultural shift forces family medicine training programs to adapt their various systems, policies, and procedures to emphasize continuity. We hope this manuscript’s review of several facets of contuinuity, some unique to training programs, helps programs ensure compliance with the ACGME requirements.
A 1948 Life magazine photo essay titled “Country Doctor” highlighted continuity of care when W. Eugene Smith photographed Dr Ceriani delivering babies, examining children, performing emergency surgery, and caring for the dying in rural Colorado. 1 Two decades later, family medicine became the 20th recognized medical specialty. 2 To this day, family medicine differentiates itself from other specialties by emphasizing personalized care delivered over the entire lifespan of patients. 3-6
For decades, primary care proponents have held that continuity of care is an essential ingredient for high-functioning health care systems. 7, 8 With continuity of care as a key characteristic of family medicine, the 2023 revision of the Accreditation Council for Graduate Medical Education (ACGME) requirements for graduate education in family medicine added two new continuity requirements: annual patient-sided continuity and annual resident-sided continuity (IV.C.3.c.5.b.ii). 9 While much of the continuity of care literature pertains to individual patient continuity, this is not what ACGME is referring to by “patient-sided continuity.” Instead, the council is referring to an aggregation of continuity for a panel of patients cared for by a resident. A better term might be “panel continuity.” Resident-sided continuity refers to what percentage of visits a primary care clinician has with patients on their own panel. This is often termed “provider continuity” and is typically available as a performance metric within EHRs.
These new requirements represent a dramatic culture shift in resident training from the previous emphasis on volume of encounters to the current emphasis on continuity of care. Many systems and parameters, such as patient empanelment, size of resident panels, balance between training in the family medicine practice (FMP) and required rotations, and scheduling of visits, will need to adapt to the new culture.
The focus of this manuscript is to synthesize the literature on continuity of care, put ACGME requirements into context, provide an understanding of the complexities surrounding continuity of care within residency training, and suggest some potential mechanisms for residencies to meet these new ACGME requirements.
The Oxford English Dictionary defines continuity as “the unbroken and consistent existence or operation of something over a period of time.” The existance of a doctor-patient relationship over time is often referred to as continuity of care. The Institute of Medicine takes this one step further by stating that continuity of care is longitudinal care coupled with effective and timely communication of health information. 10
While the concept of continuity seems intuitive, arriving at a consensus definition of continuity and a conceptual framework that explains its supposed benefits is surprisingly difficult. 7, 11, 12
Haggerty et al defined three types of continuity: informational, managerial, and relational. 12 Saultz extended this to include longitudinal, interpersonal, geographic, and familial continuity. 3 We reorganized and summarized these domains of continuity in Table 1.
|
1. Informational continuity links care between episodes and providers. It consists of the written medical documentation plus the often-unwritten patient context, values, and goals of care. Informational continuity is maintained when a primary care physician reviews the medical record to determine when a previous episode of gout occurred and what medications were used to treat it. It is also maintained when a consulting neurologist reviews the medical record provided by the primary care physician when evaluating a patient’s unilateral weakness. However, informational continuity does not imply a relationship with the patient. A lot can be known about a patient by reading their chart without ever meeting them.
|
|
2. Managerial continuity occurs when several medical professionals cooperate to provide care for a patient. This domain is especially apparent in chronic disease management and mental health care when multidisciplinary teams develop care plans for their patient. It is sometimes referred to as interdisciplinary or team-based continuity.
|
|
3. Relational continuity is found when one clinician provides care for a patient over time, connecting their past, present, and future. However, the relationship need not be cradle-to-grave. Relationship continuity can be found in the hospital if the admitting physician continues to care for the patient all the way through discharge, or if the nursing home clinician continues to follow the same residents. Relational continuity often results in unwritten informational continuity.
|
|
a. Longitudinal continuity is the most simplistic relationship form and is typically found in most family medicine and primary care practices. In common parlance, it simply implies that a single clinician provides care for the patient over time. Saultz defined it a bit more precisely and broadly as a “pattern of health care interaction that occurs in the same place, with the same medical record, and with the same professionals” allowing for a growth of knowledge about a patient over time.3
|
|
b. Interpersonal continuity is a special type of longitudinal continuity where the patient and doctor develop a partnership characterized by implicit knowledge, trust, and respect that facilitates good communication. This is the ultimate form of continuity sought by primary care medical home practices.
|
|
4. Family continuity implies the same clinician taking care of multiple family members, often from multiple generations (ie, grandfather, mother, daughter/son). That clinician possesses knowledge about the health care problems of other family members, which may impact the care of the current patient. Unfortunately, most electronic health records do not support family member linking.
|
|
5. Geographic continuity occurs when the same clinician cares for the patient in multiple locations or environments (ie, hospital, home, skilled nursing facility). The rise of hospitalists and the move away from Dr Ceriani’s full spectrum practice to the outpatient-only family physician has lowered geographic continuity.
|
Benefits of Continuity
Continuity of care can impact the quadruple aim of enhancing patient experience, improving population health, reducing costs, and improving care team well-being. 13 While we are not aware of any studies showing continuity of care to be harmful, beneficial associations are only sometimes observed. Demonstrated benefit may depend heavily on the exact measure of continuity chosen and the unique underlying medical practice characteristics of the population studied. 14
Continuity of care is generally associated with better patient satisfaction. In one systematic review, subjective measures of continuity were associated with greater patient satisfaction, but various objective measures of longitudinal continuity were not reliably associated with greater patient satisfaction. 15 However, interpersonal continuity was found to be associated with greater patient satisfaction in 19 of 22 studies. 16 And another review found that five of seven studies examining continuity of care had a positive association with patient satisfaction. 17
Numerous studies have demonstrated that continuity of care improves population health. Having more primary care physicians per capita, presumably providing continuity of care, raises life expectancy more than an equivalent number of additional specialists. 18 According to one systematic review, continuity of care provided a mortality benefit in nine of 12 studies. 19 Various measurements of continuity of care also are associated with improved chronic disease management and improved preventative services, especially during brief acute visits. 20-22, 23 However, the relationship between continuity of care and chronic disease management is not always universal. 24
Continuity of care also directly impacts the cost of care, mainly via reduced utilization. In a study of Medicare beneficiaries with chronic diseases, increased continuity of care reduced the total cost of care by reducing usage of acute care facilities. 25 A review of 22 studies found that interpersonal continuity reduced cost or utilization in 35 of 41 variables studied. 26 Continuity of care is associated with reduced emergency department use, less frequent hospitalization, and fewer readmissions. 21, 27-32 Those with the most fragmented care appear to be at the highest risk of emergency department use and subsequent hospitalization. 30, 33 However, simply having a regular source of care, defined as having more than 50% of visits with same provider group, was not associated with fewer hospitalizations. 34
Clinician well-being also may be tied to continuity of care and vice versa. One study demonstrated that family physicians exhibiting greater geographic continuity, that is engaging in practice beyond their principal site (eg, at the hospital or labor and delivery), were less likely to suffer burnout. 35 Turnover of primary care physicians, often driven by burnout, has been shown to reduce patient continuity and is estimated to cost nearly $1 billion in excess US health care expenditures annually. 36 However, physicians working part-time reported greater job satisfaction and often had superior patient satisfaction despite the obvious impact on continuity. 37, 38
Patient Preferences
Despite advantages to continuity of care, patients may not always value or seek it. While all patients seem to recognize the value of continuity of care for wellness visits and chronic disease management, many patients value access over continuity for acute visits, leading to the rise of retail clinics. 39, 40 Multimorbidity patients with a higher chronic disease burden increasingly value continuity even for acute visits. 40 Systems of care should take into account these differing patient preferences.
Measurement of Continuity
Little agreement exists on a standardized measure for continuity. 3, 6, 15, 41, 42 In a review, Jee et al found 32 different measures of continuity and grouped them into five broad categories of measurement: density of visits, dispersion of visits, sequence of visits, duration of relationships, and subjective patient estimates. 42 Most of these attempt to quantify longitudinal continuity, and the first three categories rely on patterns of visits that can be obtained from widely available health care claims databases. 3, 43 Whether claims-based measures of continuity match patient perceptions of continuity is subject to debate. 44 Few accepted measures of family or geographic continuity exist. 3 Visit entropy has been proposed as a measure of managerial continuity in team-based care environments because it is able to detect and quantify organized visit patterns produced by team-based care. 6, 14
Perhaps the most widely accepted and well-known measure of continuity, defined in 1975 by Breslau and Reeb, is usual provider continuity (UPC). 45 It is expressed as the proportion of visits with the patient’s primary (or most frequent) clinician divided by the total number of visits over a period of time, typically one year. 45 UPC is intuitive to understand, simple to calculate, and yields a well-bounded percentage with 0% representing no continuity and 100% representing perfect continuity.
Common Issues With Continuity Metrics
Technical issues and performance characteristics, however, make UPC and other related continuity metrics less than ideal measures of longitudinal or interpersonal continuity. 6, 14 First, many healthy patients may not require a health care visit in a given year, yielding an undefined divided by zero condition. 6, 46 Second, UPC and other metrics often are highly skewed distributions with many patients having either zero or almost perfect continuity, making analysis with traditional statistical methods difficult. 6, 14, 43 Third, for the typically small number of health care visits that a patient has in a given year, UPC results in a much more discrete distribution than expected. 14 For instance, three visits results in only four possible values for UPC (1.00, 0.67, 0.33, 0). Finally, UPC is unable to distinguish the increased interpersonal continuity produced by multiple visits over time with the same clinician (ie, 1/1 is the same as 5/5). 14
The Rise of the Patient-Centered Medical Home
Medicine has changed dramatically in the 75 years since the days of Dr Ceriani, and the electronic health records, polymerase chain reaction tests, and handheld ultrasound devices present in today’s physician offices would be completely foreign to him. With advances in technology such as magnetic resonance imaging and robotic surgery and increasing knowledge concentration, medicine has become more complex, more specialized, and more fragmented, and involves more multidisciplinary health care providers. 14, 33, 39, 47 Today’s emphasis is on convenience and team-based care. 39, 48 In spite of this, patients still desire a relationship with their physician. 14, 40, 49, 50 In response, the patient-centered medical home movement seeks to replicate the responsibility and coordination of care that used to be provided by the traditional 1:1 longitudinal continuity relationship like Dr Ceriani’s practice. 51 Unfortunately, most continuity metrics fail to recognize the managerial continuity produced by patient-centered medical homes. In fact, UPC penalizes this type of planned and organized referral practice by assigning it a lower continuity score and failing to differentiate it from an unplanned visit pattern. 14 As a result, UPC may not be as capable of detecting the beneficial effects of continuity as more sophisticated measures. 20, 30
Telemedicine
The use of telemedicine and virtual visits expanded rapidly during the COVID-19 pandemic. 52 In a study of patients with diabetes, higher continuity of care was associated with improved hemoglobin A1c testing, and greater telemedicine use mediated about 39% of this relationship. 53 Thus, an association triad of increased continuity, greater use of telemedicine, and improved outcomes appears to exist. However, telemedicine visits with continuity may not be directly measured in some of the current models.
CONTINUITY IN THE FAMILY MEDICINE RESIDENCY PRACTICE
Though the 2023 revision of ACGME’s requirements for graduate education in family medicine added two new continuity requirements (ie, annual patient-sided continuity and annual resident-sided continuity [IV.C.3.c.5.b.ii]), 9 the specific definition and calculation of these new continuity requirements was not addressed, perhaps because of the uncertainty surrounding definitions and measurements detailed earlier. Furthermore, no citations were provided for the 30% and 40% continuity requirement for postgraduate year (PGY)-2 and PGY-3 residents, respectively. A review conducted in 2018 reported a median UPC continuity of 56% among residency clinics reporting continuity in the medical literature. 54 However, that was not a representative sample and was probably a gross overestimation of actual resident clinic continuity because it included only residencies conducting studies on continuity and publishing their results (subject to publication bias and survivor bias). Due to a number of factors, including resident rotation scheduling and turnover, continuity is usually lower in resident clinics than in nonteaching practices. 55
This new requirement represents a dramatic culture shift in the FMP from the previous emphasis on volume of encounters to the current emphasis on continuity of care. Many localized systems and parameters, such as patient empanelment, size of resident panels, balance between FMP training and required rotations, and scheduling of visits, significantly impact continuity across all family medicine residencies.
Resident and Panel Continuity
Based on information presented at various medical education conferences, most educators appear to assume that ACGME is referring to a variation of UPC when they speak of patient-sided and resident-sided continuity. This was confirmed in a frequently asked questions document the council released in July 2023, showing examples of how to calculate patient-sided and resident-sided continuity. 56 UPC (and its derivatives) was the most common type of continuity reported in a scoping review of 34 articles looking at the continuity reported by residency clinics. 54
A continuity visit is defined as a resident conducting a visit in the FMP with a patient on their panel. Resident-sided continuity (CR) can be defined as the number of continuity visits divided by the total number of visits performed by the resident in the FMP. Just like UPC, the result will range between 0 and 1 for each resident. Resident-sided continuity, or provider continuity (as it is sometimes called), is a measure of how often a given resident sees their own patients and is often found as a performance metric in EHRs.
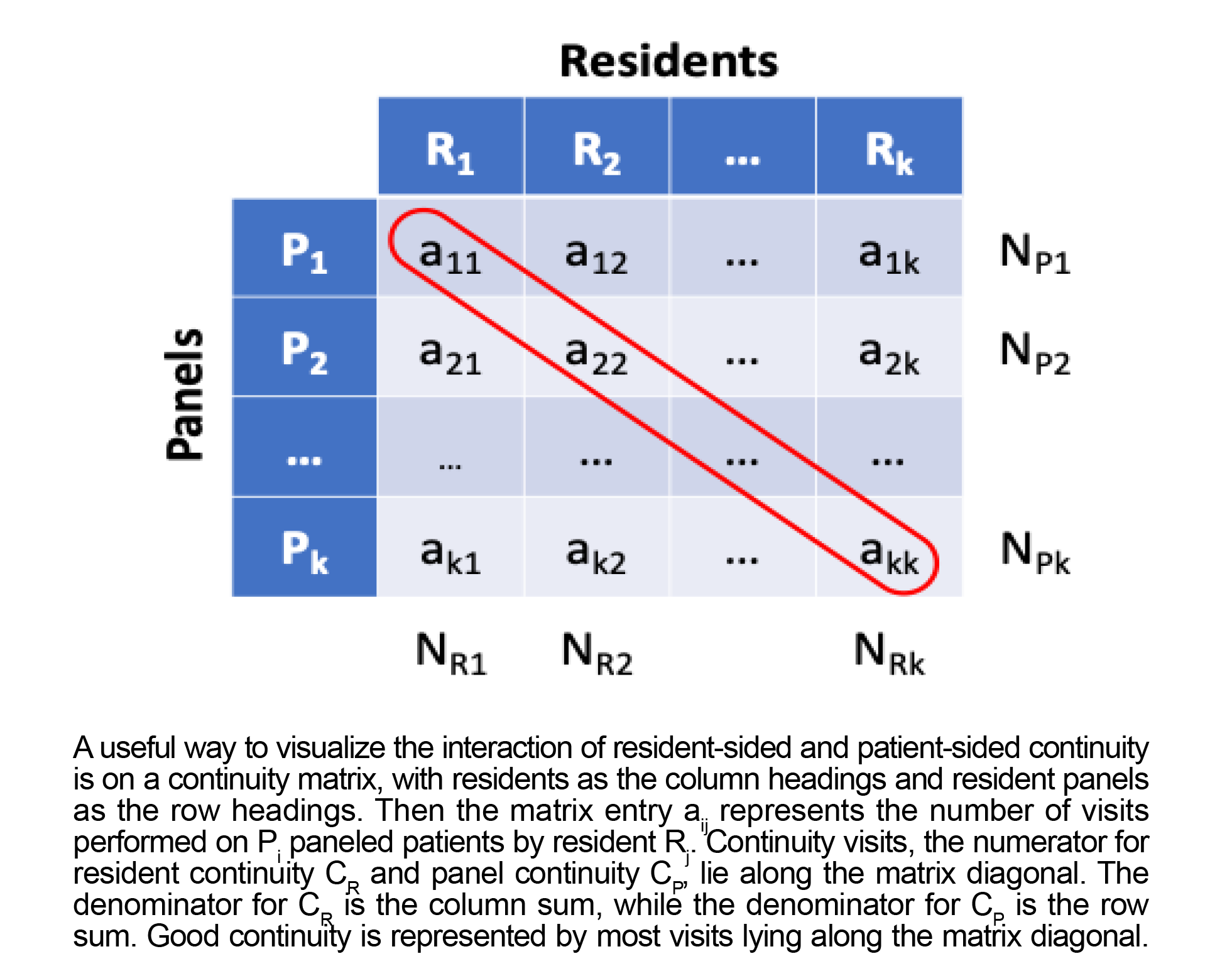
Likewise, patient-sided continuity (CP) can be defined as the number of continuity visits divided by the total number of FMP visits made by patients on a resident’s panel. Because this is an aggregated measure, we prefer the term “panel continuity” to avoid confusion with individual patient-level measures of continuity. Panel continuity (CP) will also range from 0 to 1 for each resident panel. The mathematical formulas for resident-sided continuity (CR) and patient-sided continuity (CP) are shown in Figure 1. Figure 2 shows a unique way to visualize the interaction of these two different types of continuity on a matrix.
Empanelment and Data
Empanelment, an essential component of population health management, is the process of assigning patients to a responsible clinician or care team. 57 Most EHRs provide a mechanism for empanelment by recording the primary care clinician. To calculate continuity, residents must have patient panels and be listed as the patient’s primary care clinician. How residencies choose to make this assignment is subject to local procedures, but experts recommend the four-cut method shown in Table 2. 58 Using an algorithm based on the four-cut method, a large internal medicine residency improved continuity through the reassignment process. 59
|
Situation
|
Action
|
|
1. Patients who saw only one clinician
|
Assign them to that clinician.
|
|
2. Patients who saw one clinician predominantly
|
Assign them to that clinician.
|
|
3. Patients who were seen by more than one clinician equally
|
Assign them to the first, last, or most recent general/annual exam clinician (any standard criteria can be used).
|
|
4. For the remaining patients
|
Ask the patient or clinicians who the primary clinician should be.
|
One thing that is unique to residency training is the annual graduation of resident physicians, which results in panel reassignment. In a typical family medicine residency, approximately one-third of the patients will require reassignment annually (more if the panel size grows throughout training). This process affects up to 1 million patients in the United States annually. 60 In the case of a clinic-first model, with approximately equal time in the FMP throughout residency, reassigning a graduating resident’s panel to an incoming PGY1 resident is trivial. However, even in this situation, the program director may wish to engage in panel management as per ACGME requirements to balance the ages, genders, and medical complexity of panels. If time in clinic is unequally divided between the various stages of resident training, the issue becomes much more complex and involves rebalancing all panels using some combination of the four-cut method and the right-sizing equation (shown in the next section). Optimizing panel size helps maximize resident and panel continuity.
Resident continuity (CR) is usually readily available within commercial EHRs as a metric provided to every clinician. However, panel continuity (CP) is often more challenging to obtain because many EHRs do not directly support the concept. The process tends to be more manual in nature, requiring pulling all EHR visit information for each empaneled patient. Then the raw visit information is linked to the patient data model containing the assigned primary clinician, and continuity visits and total visits are counted and summed by patient for each resident. Institutions may need to work with their information technology or EHR vendor to develop a solution. Stating that this is an ACGME requirement may help obtain the resources needed.
Right-Sizing Panels
Extensive literature is available on panel size for primary care clinicians and the effect that mismatched panel size can have on patient outcomes and physician burnout. 61-65 Less information exists about optimal panel size for residencies. Anecdotal evidence presented at medical education conferences and some published reports have placed the family medicine PGY3 panel size at 300 to 400 patients. 60 Traditionally, family medicine residencies grow panel size throughout training; more recently, however, some programs have experimented with equal panel size across all years of training.
Despite a lack of information about optimal panel size in residency, one can still rely on the laws of supply and demand to calculate a right-sized panel. The following equation is key:
(days in clinic/yr)(visits per day)=(panel size)(mean visits per patient/yr)
The left side of the equation represents the supply of visits or capacity of a clinician. The right side represents patient demand. Looking at historical data for the practice over the past year can usually produce an accurate estimate of the mean visits per patient per year. In our experience, relying on national or even institutional data from other practice sites can be misleading because practice patterns are highly localized, causing mean outpatient visits to vary significantly. For example, data from the Veterans Administration has shown significant geographic variation in the rate of outpatient visits. 66 Tools exist to help program directors manage panel size (eg, https://www.aafp.org/pubs/fpm/blogs/inpractice/entry/right_sized_patient_panel.html).
When panels are appropriately balanced, both resident and panel continuity can be maximized simultaneously. If an oversupply or excess capacity occurs, these appointment slots will likely be filled by noncontinuity patients, resulting in poor resident continuity (CR). Conversely, if demand exceeds supply, paneled patients cannot access their primary clinician, and panel continuity (CP) suffers. Mathematically, the lower bound for resident continuity (CR) is inversely proportional to the number of residents in a program, and the lower bound for panel continuity (CP) is the proportion of time the resident spends in clinic divided by the total time all residents spend in clinic. This means that panel continuity goals will be easier to achieve if residents spend more time in clinic. Likewise, larger programs will have more inherent difficulty meeting resident continuity goals and thus will need to actively and strategically manage visit scheduling.
Strategies to Optimize Resident and Panel Continuity in the FMP
Optimizing continuity in a resident practice highlights tensions between the FMP and inpatient, specialty, and away rotation schedules. Additionally, institutional pressures to prioritize appointment fill rates, provide access, and improve patient satisfaction and convenience all affect the ability to achieve continuity within the FMP. To address these challenges, a multipronged approach is needed, including right-sizing patient panels, as described earlier. This also could include novel resident scheduling paradigms to ensure consistency of resident presence in the FMP, such as those proposed in the clinic-first approach. 67 In addition, residency staff may need to educate institutional leadership, scheduling staff, and patients to explain why sacrificing fill rates and convenience to prioritize continuity is necessary.
Resident Absences and Staff Panels
All primary care clinics deal with providers being absent for illness, vacation, family and parental leave, and other reasons, but residency clinics encounter a number of scheduling challenges at a higher frequency than most clinics. In addition to core required rotations that usually allow for some FMP clinic time in a given week, residency clinics often have to account for residents being away for elective rotations, scheduled off-site rotations, duty hours from overnight call, and other absences. Residency programs need to develop local strategies that take into account their provider mix and their clinic access needs. Some possible solutions include adjusting or implementing guidelines on which rotations may be interrupted by vacation or how many days of vacation may occur during FMP, scheduling patients empaneled to absent residents on faculty or advanced practice providers’ calendars rather than on other residents’ schedules, and altering the rotation schedule. One program that changed the rotation schedule by implementing clinic-first principles saw increased resident-sided continuity for all residents and increased patient-sided continuity for PGY1s. 68
Maintaining staff practices in the FMP is a necessary evil. Per ACGME requirements, faculty are required to “see patients within that FMP” (II.B.2.g) and to role model “broad spectrum family medicine care” (II.B.1.c). 9 However, when faculty see resident patients, they decrease panel continuity. Likewise, if faculty members have panels, resident continuity decreases when residents see those patients. Such visits should be minimized.
Recent changes in ACGME requirements shift the focus of family medicine residency training from counting the volume of visits that residents see during their training to emphasizing resident and patient-facing continuity. This cultural shift will force family medicine residencies to measure continuity metrics and understand how various systems, policies, and procedures impact continuity. While family medicine as a specialty continues to embrace continuity, local factors and the unique aspects of a training program make achieving continuity within family medicine residencies particularly challenging. From the perspective of a family medicine residency, this manuscript has discussed the underlying concepts of continuity of care unique to residencies, reviewed measurement of resident-sided and patient-sided (or panel-sided) continuity, and provided recommendations on optimizing continuity for continued ACGME compliance.
Funding was provided by the Department of Family Medicine, Mayo Clinic Small Grants Program (<$10k).
References
-
Smith WE. Country doctor. Life. 1948;25.
-
-
Saultz JW. Defining and measuring interpersonal continuity of care.
Ann Fam Med. 2003;1(3):134-143.
doi:10.1370/afm.23
-
Starfield B. Family medicine should shape reform, not vice versa. Fam Pract Manag. 2009;16(4):6-7.
-
Dai M, Pavletic D, Shuemaker JC, Solid CA, Phillips RL Jr. Measuring the value functions of primary care: physician-level continuity of care quality measure.
Ann Fam Med. 2022;20(6):535-540.
doi:10.1370/afm.2880
-
Garrison GM, Bania B. Visit entropy: comparing a novel method to existing continuity of care measures.
Eur J Pers Cent Healthc. 2015;3(3):343-351.
doi:10.5750/ejpch.v3i3.1002
-
-
Bodenheimer T, Ghorob A, Willard-Grace R, Grumbach K. The 10 building blocks of high-performing primary care.
Ann Fam Med. 2014;12(2):166-171.
doi:10.1370/afm.1616
-
-
Donaldson MS, Yordy KD, Lohr KN, Vanselow NA, eds. Primary Care: America’s Health in a New Era. National Academies Press; 1996.
-
-
Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review.
BMJ. 2003;327(7425):1,219-1,221.
doi:10.1136/bmj.327.7425.1219
-
Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider.
Ann Fam Med. 2014;12(6):573-576.
doi:10.1370/afm.1713
-
Garrison GM, Dilger BT. Quantifying organization of care in a complex healthcare environment.
J Eval Clin Pract. 2020;26(5):1,548-1,551.
doi:10.1111/jep.13392
-
Adler R, Vasiliadis A, Bickell N. The relationship between continuity and patient satisfaction: a systematic review.
Fam Pract. 2010;27(2):171-178.
doi:10.1093/fampra/cmp099
-
Saultz JW, Albedaiwi W. Interpersonal continuity of care and patient satisfaction: a critical review.
Ann Fam Med. 2004;2(5):445-451.
doi:10.1370/afm.91
-
van Walraven C, Oake N, Jennings A, Forster AJ. The association between continuity of care and outcomes: a systematic and critical review.
J Eval Clin Pract. 2010;16(5):947-956.
doi:10.1111/j.1365-2753.2009.01235.x
-
Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of primary care physician supply with population mortality in the United States, 2005-2015.
JAMA Intern Med. 2019;179(4):506-514.
doi:10.1001/jamainternmed.2018.7624
-
Baker R, Freeman GK, Haggerty JL, Bankart MJ, Nockels KH. Primary medical care continuity and patient mortality: a systematic review.
Br J Gen Pract. 2020;70(698):e600-e611.
doi:10.3399/bjgp20X712289
-
Dilger BT, Gill MC, Lenhart JG, Garrison GM. Visit entropy associated with diabetic control outcomes.
J Am Board Fam Med. 2019;32(5):739-745.
doi:10.3122/jabfm.2019.05.190026
-
Cabana MD, Jee SH. Does continuity of care improve patient outcomes? J Fam Pract. 2004;53(12):974-980.
-
Matulis JC III, Schilling JJ, North F. Primary care provider continuity is associated with improved preventive service ordering during brief visits for acute symptoms.
Health Serv Res Manag Epidemiol. 2019;6.
doi:10.1177/2333392819826262
-
Alazri M, Heywood P, Neal RD, Leese B. Continuity of care: literature review and implications. Sultan Qaboos Univ Med J. 2007;7(3):197-206.
-
Gill JM, Mainous AG III, Diamond JJ, Lenhard MJ. Impact of provider continuity on quality of care for persons with diabetes mellitus.
Ann Fam Med. 2003;1(3):162-170.
doi:10.1370/afm.22
-
Hussey PS, Schneider EC, Rudin RS, Fox DS, Lai J, Pollack CE. Continuity and the costs of care for chronic disease.
JAMA Intern Med. 2014;174(5):742-748.
doi:10.1001/jamainternmed.2014.245
-
Saultz JW, Lochner J. Interpersonal continuity of care and care outcomes: a critical review.
Ann Fam Med. 2005;3(2):159-166.
doi:10.1370/afm.285
-
Ionescu-Ittu R, McCusker J, Ciampi A, et al. Continuity of primary care and emergency department utilization among elderly people.
CMAJ. 2007;177(11):1,362-1,368.
doi:10.1503/cmaj.061615
-
Knight JC, Dowden JJ, Worrall GJ, Gadag VG, Murphy MM. Does higher continuity of family physician care reduce hospitalizations in elderly people with diabetes?
Popul Health Manag. 2009;12(2):81-86.
doi:10.1089/pop.2008.0020
-
Menec VH, Sirski M, Attawar D, Katz A. Does continuity of care with a family physician reduce hospitalizations among older adults?
J Health Serv Res Policy. 2006;11(4):196-201.
doi:10.1258/135581906778476562
-
Garrison GM, Keuseman R, Bania B, Robelia P, Pecina J. Visit entropy associated with hospital readmission rates.
J Am Board Fam Med. 2017;30(1):63-70.
doi:10.3122/jabfm.2017.01.160186
-
Gill JM, Mainous AG III, Nsereko M. The effect of continuity of care on emergency department use.
Arch Fam Med. 2000;9(4):333-338.
doi:10.1001/archfami.9.4.333
-
Gill JM, Mainous AG III. The role of provider continuity in preventing hospitalizations.
Arch Fam Med. 1998;7(4):352-357.
doi:10.1001/archfami.7.4.352
-
Kern LM, Seirup JK, Rajan M, Jawahar R, Stuard SS. Fragmented ambulatory care and subsequent healthcare utilization among Medicare beneficiaries. Am J Manag Care. 2018;24(9):e278-e284
-
Gill JM. Can hospitalizations be avoided by having a regular source of care? Fam Med. 1997;29(3):166-171.
-
Weidner AKH, Phillips RL Jr, Fang B, Peterson LE. Burnout and scope of practice in new family physicians.
Ann Fam Med. 2018;16(3):200-205.
doi:10.1370/afm.2221
-
Sinsky CA, Shanafelt TD, Dyrbye LN, Sabety AH, Carlasare LE, West CP. Health care expenditures attributable to primary care physician overall and burnout-related turnover: a cross-sectional analysis.
Mayo Clin Proc. 2022;97(4):693-702.
doi:10.1016/j.mayocp.2021.09.013
-
Bodenheimer T, Haq C, Lehmann W. Continuity and access in the era of part-time practice.
Ann Fam Med. 2018;16(4):359-360.
doi:10.1370/afm.2267
-
Panattoni L, Stone A, Chung S, Tai-Seale M. Patients report better satisfaction with part-time primary care physicians, despite less continuity of care and access.
J Gen Intern Med. 2015;30(3):327-333.
doi:10.1007/s11606-014-3104-6
-
Rohrer JE, Angstman KB, Garrison GM, Maxson JA, Furst JW. Family medicine patients who use retail clinics have lower continuity of care.
J Prim Care Community Health. 2013;4(2):150-153.
doi:10.1177/2150131912471683
-
Ehman KM, Deyo-Svendsen M, Merten Z, Kramlinger AM, Garrison GM. How preferences for continuity and access differ between multimorbidity and healthy patients in a team care setting.
J Prim Care Community Health. 2017;8(4):319-323.
doi:10.1177/2150131917704556
-
Rogers J, Curtis P. The concept and measurement of continuity in primary care.
Am J Public Health. 1980;70(2):122-127.
doi:10.2105/AJPH.70.2.122
-
Jee SH, Cabana MD. Indices for continuity of care: a systematic review of the literature.
Med Care Res Rev. 2006;63(2):158-188.
doi:10.1177/1077558705285294
-
Pollack CE, Hussey PS, Rudin RS, Fox DS, Lai J, Schneider EC. Measuring care continuity: a comparison of claims-based methods.
Med Care. 2016;54(5):e30-e34.
doi:10.1097/MLR.0000000000000018
-
Bentler SE, Morgan RO, Virnig BA, Wolinsky FD. Do claims-based continuity of care measures reflect the patient perspective?
Med Care Res Rev. 2014;71(2):156-173.
doi:10.1177/1077558713505909
-
-
Garrison GM, Traverse CR, Fish RG. A case study of visit-driven preventive care screening using clinical decision support: the need to redesign preventive care screening.
Health Serv Res and Manag Epidemiol. 2016;3.
doi:10.1177/2333392816650344
-
Wright M, Mainous AG III. Can continuity of care in primary care be sustained in the modern health system?
Aust J Gen Pract. 2018;47(10):667-669.
doi:10.31128/AJGP-06-18-4618
-
Mitchell JD, Haag JD, Klavetter E, et al. Development and implementation of a team-based, primary care delivery model: challenges and opportunities.
Mayo Clin Proc. 2019;94(7):1,298-1,303.
doi:10.1016/j.mayocp.2019.01.038
-
Turner D, Tarrant C, Windridge K, et al. Do patients value continuity of care in general practice? An investigation using stated preference discrete choice experiments.
J Health Serv Res Policy. 2007;12(3):132-137.
doi:10.1258/135581907781543021
-
Waibel S, Henao D, Aller MB, Vargas I, Vázquez ML. What do we know about patients’ perceptions of continuity of care? a meta-synthesis of qualitative studies.
Int J Qual Health Care. 2012;24(1):39-48.
doi:10.1093/intqhc/mzr068
-
Rosenthal TC. The medical home: growing evidence to support a new approach to primary care.
J Am Board Fam Med. 2008;21(5):427-440.
doi:10.3122/jabfm.2008.05.070287
-
Ye S, Kronish I, Fleck E, et al. Telemedicine expansion during the COVID-19 pandemic and the potential for technology-driven disparities.
J Gen Intern Med. 2021;36(1):256-258.
doi:10.1007/s11606-020-06322-y
-
Tierney AA, Payán DD, Brown TT, Aguilera A, Shortell SM, Rodriguez HP. Telehealth use, care continuity, and quality: diabetes and hypertension care in community health centers before and during the COVID-19 pandemic.
Med Care. 2023;61(suppl 1):S62-S69.
doi:10.1097/MLR.0000000000001811
-
Walker J, Payne B, Clemans-Taylor BL, Snyder ED. Continuity of care in resident outpatient clinics: a scoping review of the literature.
J Grad Med Educ. 2018;10(1):16-25.
doi:10.4300/JGME-D-17-00256.1
-
Fortuna RJ, Garfunkel L, Mendoza MD, et al. Factors associated with resident continuity in ambulatory training practices.
J Grad Med Educ. 2016;8(4):532-540.
doi:10.4300/JGME-D-15-00755.1
-
-
Kivlahan C, Pellegrino K, Grumbach K, et al. Calculating Primary Care Panel Size. University of California; January 2017.
-
Weber R, Murray M. The right-sized patient panel: a practical way to make adjustments for acuity and complexity. Fam Pract Manag. 2019;26(6):23-29.
-
Wajnberg A, Fishman M, Hernandez CR, Kweon SY, Coyle A. Empanelment in a resident teaching practice: a cornerstone to improving resident outpatient education and patient care.
J Grad Med Educ. 2019;11(2):202-206.
doi:10.4300/JGME-D-18-00423.3
-
Compton R, Sebring A, Dalrymple S, Rollins LK. Engaging family medicine residents in a structured patient panel reassignment process.
Fam Med. 2021;53(4):300-304.
doi:10.22454/FamMed.2021.272274
-
Angstman KB, Horn JL, Bernard ME, et al. Family medicine panel size with care teams: impact on quality.
J Am Board Fam Med. 2016;29(4):444-451.
doi:10.3122/jabfm.2016.04.150364
-
Green LV, Savin S, Murray M. Providing timely access to care: what is the right patient panel size?
Jt Comm J Qual Patient Saf. 2007;33(4):211-218.
doi:10.1016/S1553-7250(07)33025-0
-
Dahrouge S, Hogg W, Younger J, Muggah E, Russell G, Glazier RH. Primary care physician panel size and quality of care: a population-based study in Ontario, Canada.
Ann Fam Med. 2016;14(1):26-33.
doi:10.1370/afm.1864
-
Altschuler J, Margolius D, Bodenheimer T, Grumbach K. Estimating a reasonable patient panel size for primary care physicians with team-based task delegation.
Ann Fam Med. 2012;10(5):396-400.
doi:10.1370/afm.1400
-
Hong CS, Atlas SJ, Chang Y, et al. Relationship between patient panel characteristics and primary care physician clinical performance rankings.
JAMA. 2010;304(10):1,107-1,113.
doi:10.1001/jama.2010.1287
-
Ashton CM, Petersen NJ, Souchek J, et al. Geographic variations in utilization rates in Veterans Affairs hospitals and clinics.
N Engl J Med. 1999;340(1):32-39.
doi:10.1056/NEJM199901073400106
-
Gupta R, Barnes K, Bodenheimer T. Clinic first: 6 actions to transform ambulatory residency training.
J Grad Med Educ. 2016;8(4):500-503.
doi:10.4300/JGME-D-15-00398.1
-
Paul KJ, Hidaka BH, Ford P, Morris C. Measuring greater patient-provider continuity in a clinic-first family medicine residency curriculum.
Perm J. 2021;25().
doi:10.7812/TPP/20.290




There are no comments for this article.