Background and Objectives: The family medicine (FM) approach to health care across the life span is well-suited to providing care for persons living with autism spectrum disorder (ASD). Little is known about ASD curricula in FM residency training and the characteristics of FM residency programs that prepare their residents to care for persons with this disorder.
Methods: Our study questions were part of a larger omnibus survey by the Council of Academic Family Medicine Educational Research Alliance (CERA) with data collection from November 16 to December 18, 2022, from FM residency program directors (PDs). ASD curricula were investigated using 10 questions, with descriptive analyses and nonparametric comparisons between program variables and ASD curriculum.
Results: The response rate was 42.18%, with FM PDs reporting that their programs were preparing residents in the care of youth (71.53%) and adults (68.33%) with ASD, but to a lesser extent (58.89%) in facilitating transitions of care. Programs with faculty champions, access to published curricula, sufficient patients with ASD, and engagement of interprofessional faculty reported a higher proportion of resident preparedness. PDs of community-based programs were most confident in their ability to teach ASD care and transitions of care.
Conclusions: Most FM PDs modestly agreed that they are preparing residents to provide care to patients with ASD and their families. PDs of programs with greater access to resources (ie, published curriculum, faculty champions, sufficient patients with ASD, interprofessional faculty experts) believed that their residents were more prepared. Community-based FM educators may help lead the way in providing models for care and education in this regard.
Autism spectrum disorder (ASD) is a lifelong neurodevelopmental disorder characterized by deficits in social communication and restricted, repetitive patterns of behavior, interests, or activities.1 Currently, the estimated prevalence is one in 36 children in the United States.2 ASD impacts not only the child, but the entire family. 3 Individuals with ASD face challenges in navigating community systems 4 and health care transitions.5 Primary care providers and the patient-centered medical home have a key role in the early identification of ASD symptoms and facilitation of the process of diagnosis and intervention. 6
Family medicine (FM) has a broad-spectrum approach to health care across the life span, including an emphasis on biopsychosocial and context-oriented models of care. 7 Furthermore, FM cares for a high proportion of children in rural and remote areas 8 where the greatest disparity in diagnostics and services exists for children with ASD. 9
Despite the mandatory block rotation 10 where ASD and other developmental conditions are covered, pediatric trainees have reported insufficient knowledge about ASD 11 and lower competence in caring for youth with ASD.12 In the latter study, FM clinicians reported less self-assessed competency around ASD than their pediatric colleagues, 12 and in yet another study, FM providers reported limited knowledge and insufficient skills and tools for providing health care to pediatric and adult patients with ASD. 13
Among autism curricular materials are the American Academy of Pediatric’s autism toolkit14 and the Centers for Disease Control and Prevention’s “Learn the signs. Act early” program.15 Autism Case Training is a developmental-behavioral pediatrics curriculum that offers online content and video case-based instruction. 16 Such programs have shown short-term improvements in pediatric residents’ knowledge and self-assessed competence regarding ASD. 17 Internationally, Garg et al has suggested a case-based curriculum addressing early identification and ongoing surveillance of children with ASD, mainly for use with primary care providers. 18
We explored the state of ASD curricula nationally in FM residency training. We hypothesized that program directors (PDs) would report higher levels of resident preparedness for ASD care when their programs:
-
Were in larger, university-based settings;
-
Had a sufficient volume of patients with lived experiences of ASD;
-
Used published curricular materials; and
-
Had subspecialist collaborations and faculty champions.
Measurement
Our study questions were part of a larger omnibus survey conducted by the Council of Academic Family Medicine Educational Research Alliance (CERA).19 We formulated our questions following a comprehensive literature review and made revisions based on feedback from FM physicians who were not part of the survey group as well as from the CERA steering committee. The CERA steering committee evaluated questions for consistency with the overall subproject aim, readability, and existing evidence of reliability and validity. CERA pretested with FM educators who were not part of the target population. Following pretesting, we modified questions for flow, timing, and readability. The ASD curricular component consisted of 10 questions and included Likert-like single-response and multiple-response formats, along with specific examples of available curricula (see Appendix).
Sampling
The project was approved by the American Academy of Family Physicians Institutional Review Board in November 2022. Data was collected from November 16 to December 18, 2022. The sampling frame for the survey was all US FM program directors accredited by the Accreditation Council for Graduate Medical Education as identified by the Association of Family Medicine Residency Directors.
Data Collection and Response
CERA staff emailed invitations to participate in the survey and the survey itself using the online program SurveyMonkey (SurveyMonkey Inc). Four weekly follow-up emails encouraged nonrespondents to participate; a fifth reminder arrived 2 days before the survey closed. The mailing list included 722 PDs. Nine email addresses were undeliverable, and 35 programs did not meet the criteria for participation (the programs were less than 3 years old), reducing the sample size to 678. CERA received 286 completed surveys, with an overall response rate of 42.18% (286/678).
Analysis
We conducted descriptive statistical analysis (frequency and percentage, mean and standard deviation, when appropriate) on each item. The nonparametric Fisher’s exact test and the two-sample t test were conducted for analyzing the association between the program variables (type, size, number of residents) and three outcome variables (domains of care) addressing the quality of ASD curriculum. The outcome variables were (1) “My program does an excellent job of preparing residents to deliver care to children and adolescents with ASD and their families”; (2) “My program does an excellent job of preparing residents to deliver care to adults with ASD and their families”; and (3) “My program does an excellent job of preparing residents to facilitate transitions of care for young adults with ASD from pediatric specialties to FM care. In the variables, we used the word “excellent” to reflect the personal perception of the FM PD about the quality of the program. Therefore, excellence is self-identified and holistic in interpretation, taking into account established competencies seen in the actions of residents and graduates of the program. If a variable was significantly associated with any of the domains, a pairwise proportion test was conducted for the post hoc analysis with the Bonferroni adjustment to test the agreement. We assessed all the tests using the P value compared with a 5% level of significance. We performed all analyses using SAS version 9.4 (SAS Institute, Inc).
PD respondents self-reported as 50.7% female, 68.5% White/Caucasian, and 17.5% underrepresented groups in medicine. On average, PDs had served for 6.72 years (SD=6.25 yrs). They represented mostly community-based, university-affiliated programs with the largest proportion having between 19 and 31 residents in the program. Table 1 provides descriptive statistics of the sample.
|
Characteristic
|
Description
|
n (%)
|
|
Type of residency program
|
University-based
|
41 (14.34)
|
|
Community-based/university-affiliated
|
164 (57.34)
|
|
Community-based/nonaffiliated
|
69 (24.13)
|
|
Military
|
4 (1.40)
|
|
Other (please specify)
|
8 (2.80)
|
|
Approximate community size of program location
|
Less than 30,000
|
31 (10.84)
|
|
30,000 to 74,999
|
42 (14.69)
|
|
75,000 to 149,000
|
57 (19.93)
|
|
150,000 to 499,999
|
67 (23.43)
|
|
500,000 to 1 million
|
41 (14.34)
|
|
More than 1 million
|
48 (16.78)
|
|
Number of residents in program
|
<19
|
113 (39.65)
|
|
19–31
|
126 (44.21)
|
|
>31
|
46 (16.14)
|
|
Gender
|
Female/woman
|
145 (50.70)
|
|
Male/man
|
135 (47.20)
|
|
Gender queer/gender nonconforming
|
0
|
|
Nonbinary
|
0
|
|
Chose not to disclose
|
6 (2.10)
|
|
Race and ethnicity
|
American Indian/Alaska Native/Indigenous
|
3 (1.05)
|
|
Asian
|
33 (11.54)
|
|
Black/African American
|
18 (6.29)
|
|
Hispanic/Latino/of Spanish Origin
|
20 (6.99)
|
|
Middle Eastern/North African
|
4 (1.4)
|
|
Native Hawaiian/other Pacific Islander
|
0
|
|
White
|
196 (68.53)
|
|
Chose not to disclose
|
12 (4.2)
|
|
Self-identified as URM
|
Yes
|
50 (17.54)
|
|
No
|
235 (82.46)
|
Overall, PDs agreed that their program was preparing residents in the care of youth (71.53%) and adults (68.33%) with ASD, but to a lesser extent (58.89%) in facilitating transitions of care for young adults with ASD from pediatric providers to FM care. The preparedness for care of children/adolescents with ASD was not significantly different than for adults with ASD (P=.212).
Table 2 shows that approximately 43% of PDs indicated that they never used or did not have access to a published ASD curriculum, while another 11% reported having no awareness of the curriculum. Of survey participants, 61.57% reported that they did not have sufficient patients living with ASD to provide clinical teaching about ASD. While more than half (54%) engaged interprofessional or interdisciplinary faculty (eg, developmental-behavioral pediatric clinician, psychologist, behavioral health educator) to deliver educational content on ASD to FM residents, 83% reported having no FM faculty champion.
|
View
|
Rating
|
n
(%)
|
|
Preparation
|
|
My program does an excellent job of preparing residents to deliver care to children and adolescents with ASD and their families.
|
Strongly agree
|
21 (7.47)
|
|
Moderately agree
|
59 (21.00)
|
|
Slightly agree
|
121 (43.06)
|
|
Slightly disagree
|
48 (17.08)
|
|
Moderately disagree
|
27 (9.61)
|
|
Strongly disagree
|
5 (1.78)
|
|
My program does an excellent job of preparing residents to deliver care to adults with ASD and their families.
|
Strongly agree
|
15 (5.34)
|
|
Moderately agree
|
58 (20.64)
|
|
Slightly agree
|
119 (42.35)
|
|
Slightly disagree
|
49 (17.44)
|
|
Moderately disagree
|
30 (10.68)
|
|
Strongly disagree
|
10 (3.56)
|
|
My program does an excellent job of preparing residents to facilitate transitions of care for young adults with ASD from pediatric specialties to FM care.
|
Strongly agree
|
14 (5.19)
|
|
Moderately agree
|
40 (14.81)
|
|
Slightly agree
|
105 (38.89)
|
|
Slightly disagree
|
65 (24.07)
|
|
Moderately disagree
|
33 (12.22)
|
|
Strongly disagree
|
13 (4.81)
|
|
Resources
|
|
My program uses published standardized curricular materials, such as the ASD toolkit “Learn the signs. Act early” program or Autism Case Training (ACT).
|
Often
|
36 (12.81)
|
|
Sometimes
|
92 (32.74)
|
|
Never
|
64 (22.78)
|
|
Do not have a curriculum
|
59 (21.00)
|
|
Not aware of these materials
|
30 (10.68)
|
|
My program engages interprofessional or interdisciplinary faculty to deliver educational content on ASD to FM residents.
|
Yes
|
153 (54.64)
|
|
No
|
55 (19.64)
|
|
I don't know
|
11 (3.93)
|
|
No access to ASD specialists
|
61 (21.79)
|
|
My program has an FM faculty champion who delivers educational content on ASD to FM residents.
|
Yes
|
47 (16.97)
|
|
No
|
230 (83.03)
|
|
My program has sufficient patients living with ASD to provide excellent clinical teaching about ASD.
|
Strongly agree
|
13 (4.63)
|
|
Moderately agree
|
29 (10.32)
|
|
Slightly agree
|
66 (23.49)
|
|
Slightly disagree
|
72 (25.62)
|
|
Moderately disagree
|
66 (23.49)
|
|
Strongly disagree
|
35 (12.46)
|
|
FM faculty role-model the health care of persons living with ASD in our clinical setting.
|
Strongly agree
|
23 (8.24)
|
|
Moderately agree
|
53 (19.00)
|
|
Slightly agree
|
99 (35.48)
|
|
Slightly disagree
|
44 (15.77)
|
|
Moderately disagree
|
43 (15.41)
|
|
Strongly disagree
|
17 (6.09)
|
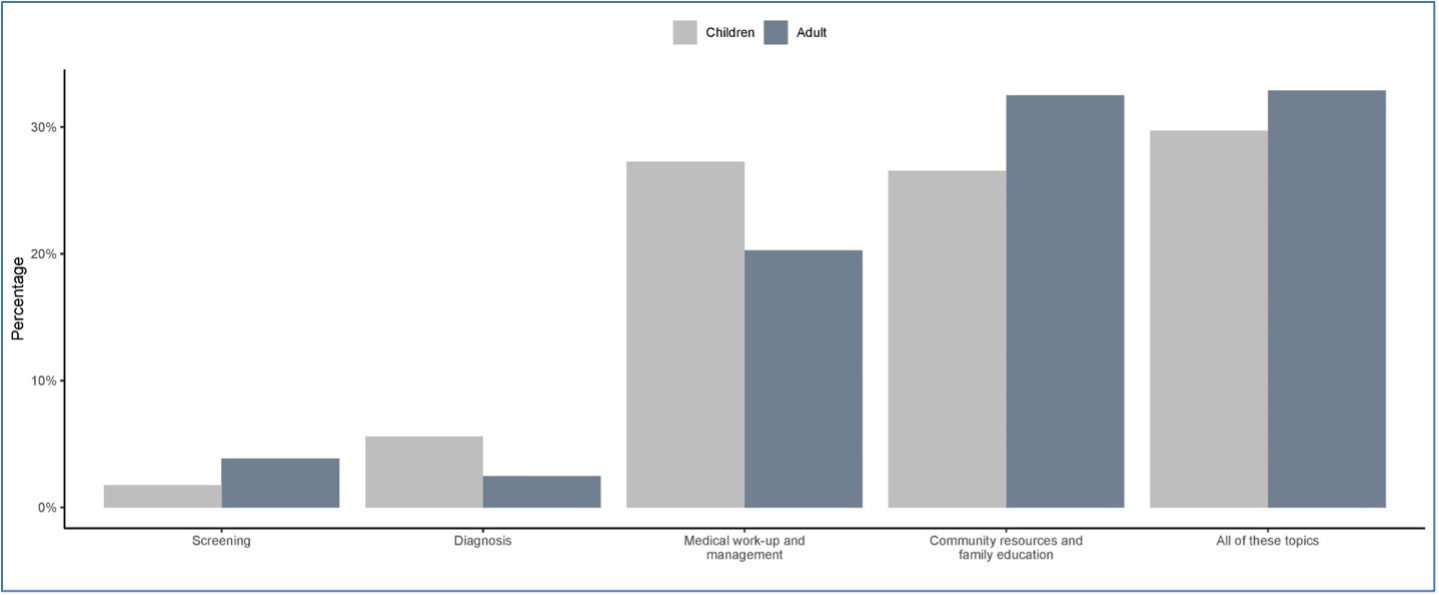
With regard to reported gaps in ASD curriculum, 95.34% and 95.00% of PDs reported significant gaps in curriculum for adult care and for children/adolescents, respectively. Figure 1 shows that educational gaps in all curricular domains, with only diagnosis and medical workup/management having a higher reported gap in youth compared to adults.
Table 3 reports program characteristics by preparedness of residents to deliver care to youth and adults with ASD and to help with transitions of care. Among program variables, only the type of program was significant for all three domains of preparedness (ie, youth, adult, and transition). In post hoc analyses, university programs were significantly less prepared compared to community-based/nonaffiliated programs in all three preparedness domains (P=.005, .007, and .020, respectively). Compared to community-based/university-affiliated programs, university programs also were lower in preparedness in the youth domain (P=.0443). We found no significant difference in preparedness for care of adults and aiding in transitions (P=.0749 and .4820, respectively).
|
Program characteristic
|
My program does an excellent job of preparing residents to . . .
|
|
. . . deliver care to children and adolescents with ASD and their families.
|
. . . deliver care to adults with ASD and their families.
|
. . . accept transitions of care of young adults with ASD and their families from pediatric specialty care.
|
|
Agree, n (%)
|
Disagree, n (%)
|
Agree, n (%)
|
Disagree, n (%)
|
Agree, n (%)
|
Disagree, n (%)
|
|
Type of residency program
|
P =.008
|
P =.017
|
P =.042
|
|
University-based
|
20 (51.28)
|
19 (48.72)
|
19 (48.72)
|
20 (51.28)
|
17 (44.74)
|
21 (55.26)
|
|
Community-based/nonaffiliated
|
55 (82.09)
|
12 (17.91)
|
53 (79.10)
|
14 (20.90)
|
49 (73.13)
|
18 (26.87)
|
|
Community-based/university affiliated
|
119 (73.01)
|
44 (26.99)
|
113 (69.33)
|
50 (30.67)
|
96 (58.90)
|
67 (41.10)
|
|
Military
|
2 (50.00)
|
2 (50.00)
|
2 (50.00)
|
2 (50.00)
|
3 (75.00)
|
1 (25.00)
|
|
Other
|
5 (62.50)
|
3 (37.50)
|
5 (62.50)
|
3 (37.50)
|
4 (50.00)
|
4 (50.00)
|
|
Size of the community
|
P =.600
|
P =.700
|
P =.600
|
|
Less than 30,000
|
22 (70.97)
|
9 (29.03)
|
23 (74.19)
|
8 (25.81)
|
20 (64.52)
|
11 (35.48)
|
|
30,000 to 74,999
|
30 (73.17)
|
11 (26.83)
|
28 (68.29)
|
13 (31.71)
|
22 (55.00)
|
18 (45.00)
|
|
75,000 to 149,999
|
34 (61.82)
|
21 (38.18)
|
36 (65.45)
|
19 (34.55)
|
31 (56.36)
|
24 (43.64)
|
|
150,000 to 499,999
|
49 (73.13)
|
18 (26.87)
|
45 (67.16)
|
22 (32.84)
|
39 (58.21)
|
28 (41.79)
|
|
500,000 to 1 million
|
31 (77.50)
|
9 (22.50)
|
31 (77.50)
|
9 (22.50)
|
29 (72.50)
|
11 (27.50)
|
|
More than 1 million
|
35 (74.47)
|
12 (25.53)
|
29 (61.70)
|
18 (38.30)
|
28 (59.57)
|
19 (40.43)
|
|
Number of residents
|
P =.700
|
P =.400
|
P =.900
|
|
<19
|
82 (73.87)
|
29 (26.13)
|
80 (72.07)
|
31 (27.93)
|
66 (60.00)
|
44 (40.00)
|
|
19–31
|
87 (70.73)
|
36 (29.27)
|
83 (67.48)
|
40 (32.52)
|
76 (61.79)
|
47 (38.21)
|
|
>31
|
31 (67.39)
|
15 (32.61)
|
28 (60.87)
|
18 (39.13)
|
27 (58.70)
|
19 (41.30)
|
Table 4 demonstrates that programs with any of the studied resources (ie, engagement of interprofessional faculty, faculty champions, sufficient patients with ASD, FM faculty role-modeling care, use of standardized curricular materials) reported higher resident preparedness for all three domains than programs without those resources.
|
My program does an excellent job of preparing residents to . . .
|
|
Program characteristic
|
. . . deliver care to children and adolescents with ASD and their families
|
. . . deliver care to adults with ASD and their families
|
. . . accept transitions of care of young adults with ASD and their families from pediatric specialty care
|
|
|
Agree, n (%)
|
Disagree, n (%)
|
Agree, n (%)
|
Disagree, n (%)
|
Agree, n (%)
|
Disagree, n (%)
|
|
Engagement of interprofessional faculty who deliver educational content on ASD
|
P =.016
|
P =.008
|
P =.001
|
|
Yes
|
121 (79.08)
|
32 (20.92)
|
117 (76.47)
|
36 (23.53)
|
108 (70.59)
|
45 (29.41)
|
|
No
|
35 (63.64)
|
20 (36.36)
|
30 (54.55)
|
25 (45.45)
|
24 (44.44)
|
30 (55.56)
|
|
I don’t know
|
7 (63.64)
|
4 (36.36)
|
6 (54.55)
|
5 (45.45)
|
4 (36.36)
|
7 (63.64)
|
|
No access to ASD specialists
|
37 (60.66)
|
24 (39.34)
|
38 (62.30)
|
23 (37.70)
|
32 (52.46)
|
29 (47.54)
|
|
FM faculty champion delivering educational content on ASD
|
P =.023
|
P =.006
|
P =.001
|
|
Yes
|
40 (85.11)
|
7 (14.89)
|
40 (85.11)
|
7 (14.89)
|
39 (82.98)
|
8 (17.02)
|
|
No
|
158 (68.70)
|
72 (31.30)
|
149 (64.78)
|
81 (35.22)
|
127 (55.46)
|
102 (44.54)
|
|
Sufficient patients living with ASD to provide excellent clinical teaching
|
P <.001
|
P <.001
|
P <.001
|
|
Strongly agree
|
13 (100.00)
|
0
|
13 (100.00)
|
0
|
12 (92.31)
|
1 (7.69)
|
|
Moderately agree
|
26 (89.66)
|
3 (10.34)
|
25 (86.21)
|
4 (13.79)
|
24 (82.76)
|
5 (17.24)
|
|
Slightly agree
|
58 (87.88)
|
8 (12.12)
|
57 (86.36)
|
9 (13.64)
|
52 (78.79)
|
14 (21.21)
|
|
Slightly disagree
|
50 (69.44)
|
22 (30.56)
|
47 (65.28)
|
25 (34.72)
|
40 (55.56)
|
32 (44.44)
|
|
Moderately disagree
|
42 (63.64)
|
24 (36.36)
|
39 (59.09)
|
27 (40.91)
|
33 (50.77)
|
32 (49.23)
|
|
Strongly disagree
|
12 (34.29)
|
23 (65.71)
|
11 (31.43)
|
24 (68.57)
|
8 (22.86)
|
27 (77.14)
|
|
FM faculty role-modeling the health care of persons living with ASD in clinical setting
|
P <.001
|
P =.001
|
P =.001
|
|
Strongly agree
|
22 (95.65)
|
1 (4.35)
|
21 (91.30)
|
2 (8.70)
|
19 (82.61)
|
4 (17.39)
|
|
Moderately agree
|
46 (86.79)
|
7 (13.21)
|
47 (88.68)
|
6 (11.32)
|
45 (84.91)
|
8 (15.09)
|
|
Slightly agree
|
74 (74.75)
|
25 (25.25)
|
72 (72.73)
|
27 (27.27)
|
67 (68.37)
|
31 (31.63)
|
|
Slightly disagree
|
29 (65.91)
|
15 (34.09)
|
26 (59.09)
|
18 (40.91)
|
21 (47.73)
|
23 (52.27)
|
|
Moderately disagree
|
22 (51.16)
|
21 (48.84)
|
18 (41.86)
|
25 (58.14)
|
10 (23.26)
|
33 (76.74)
|
|
Strongly disagree
|
6 (35.29)
|
11 (64.71)
|
6 (35.29)
|
11 (64.71)
|
5 (29.41)
|
12 (70.59)
|
|
Use of published standardized curricular materials
|
P =.001
|
P =.002
|
P =.001
|
|
Often
|
32 (88.89)
|
4 (11.11)
|
32 (88.89)
|
4 (11.11)
|
31 (86.11)
|
5 (13.89)
|
|
Sometimes
|
72 (78.26)
|
20 (21.74)
|
65 (70.65)
|
27 (29.35)
|
58 (63.74)
|
33 (36.26)
|
|
Never
|
34 (53.13)
|
30 (46.88)
|
33 (51.56)
|
31 (48.44)
|
25 (39.06)
|
39 (60.94)
|
|
Do not have a curriculum
|
46 (77.97)
|
13 (22.03)
|
43 (72.88)
|
16 (27.12)
|
38 (64.41)
|
21 (35.59)
|
|
Not aware of these materials
|
17 (56.67)
|
13 (43.33)
|
19 (63.33)
|
11 (36.67)
|
17 (56.67)
|
13 (43.33)
|
When comparing university to nonuniversity programs for resources, we found no significant difference in collaboration with specialists (P=.9), having an FM faculty champion (P=.2), having adequate patients (P>.9), having faculty role-model care (P=.5), or using curricular materials (P=.3).
Family medicine is uniquely able to provide care across the life span to individuals living with ASD and their families, and to assist in the transition of persons with ASD from pediatric to adult practices. Our study of US FM residency PDs revealed confidence in their ability to prepare residents to provide care to both pediatric and adult patients with ASD, with less confidence in preparing them for transitions of care. Programs that engaged interprofessional faculty and had FM faculty champions reported being better able to prepare residents for the care of patients with ASD; unfortunately, more than 80% of programs reported having no FM faculty champion. Through their knowledge and expertise, clinical champions help integrate evidence-based practice in clinical settings. 20
Programs with adequate clinic populations of persons living with ASD reported better training for residents about the care of those patients. Despite the prevalence of ASD in the United States, more than 60% reported an inadequate population of patients with ASD in their community. Whether this finding reflects a problem with patients’ access to care or a lack of physician awareness of patients with ASD in their communities is unclear. Limited clinical exposure has been cited as a barrier in educating residents on the care of other populations as well and is often a reflection of lack of faculty expertise in a domain as opposed to the actual absence of these persons in the community. 21
Our study revealed low levels of resident preparedness in addressing transitions of care for ASD populations. ECHO (Extension for Community Healthcare Outcomes) Autism is a hub-and-spoke model connecting primary care providers with local/regional/national content specialists in a case-based format that allows knowledge and skill enhancement for professionals in local communities to deliver evidence-based care to children with ASD and their families, 22 particularly in rural and underserved communities. ECHO can elevate prospective champions through continuing professional development while enhancing patient- and community-level health outcomes. 23 The model has been used with transition-age youth and young adults with ASD and has shown improvement in primary care providers’ self-efficacy for care of persons with ASD, including navigating the transition process, managing co-occurring conditions, and accessing resources.24 FM clinicians could look toward regional models (eg, specialty medical homes, partnerships with pediatricians) for approaches that can be adapted to fit their own community’s needs. 25
Only about one-third of PDs reported use of published ASD curricula. While not a substitute for developing faculty champions, asynchronous online learning modules 26 could be used to emphasize the significant prevalence of ASD in children and adults, introduce participants to national programs, recommend strategies for identifying local ASD resources, and describe models of care to support patients with ASD across the life span.
Our study found that community-based/nonaffiliated practices are most confident in their ability to prepare residents for the care of pediatric and adult patients with ASD as well as transitions of care, even though they did not differ from university programs in engaging resources or availability of champions. This finding may be due to university programs having access to greater numbers of pediatric physicians and ASD specialists, while community clinicians tend to independently manage care for patients with ASD. This possibility is borne out by the distribution of various pediatric subspecialists involved in the diagnosis and care of individuals with ASD (ie, neurology, psychiatry, developmental-behavioral pediatrics). 27, 28
Limitations of our study included a cross-sectional survey format and a constrained length of the survey. These factors limited our ability to explore more information about curricula, types of resources, and the nature of specialist collaborations. In addition, the response rate, while respectable, may have resulted in an overestimation of preparedness. Information on the nonresponder group was not available, which affects generalizability of findings and may reflect a volunteer selection bias. Also, we did not survey FM residents about their perceptions of preparedness in caring for this patient population; that would be a future direction.
Family medicine physicians are experts in continuity of care and are well-suited to provide the care needed by persons living with ASD and their families. Most FM program directors agreed that they were preparing residents to provide care to patients with ASD and their families, although nearly all identified significant gaps in their ASD curricula. Programs with greater access to resources (ie, published curriculum, faculty champions, sufficient patients with ASD, interprofessional faculty experts) believed that their residents were more prepared. Community-based FM educators, who reported the most confidence in their residents’ preparedness, may provide a model. Because ASD is more prevalent than FM educators may realize, programs should use curricular materials, develop faculty champions, and create models of care to support those living with ASD as they age.
Financial Support
This study was supported by the Council of Academic Family Medicine Research Alliance.
References
-
-
Maenner MJ, Shaw KA, Baio J, et al. Prevalence of autism spectrum disorder among children aged 8 Years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2016.
MMWR Surveill Summ. 2020;69(4):1-12.
doi:10.15585/mmwr.ss6904a1
-
Karst JS, Van Hecke AV. Parent and family impact of autism spectrum disorders: a review and proposed model for intervention evaluation.
Clin Child Fam Psychol Rev. 2012;15(3):247-277.
doi:10.1007/s10567-012-0119-6
-
van Schalkwyk GI, Volkmar FR. Autism spectrum disorders: challenges and opportunities for transition to adulthood.
Child Adolesc Psychiatr Clin N Am. 2017;26(2):329-339.
doi:10.1016/j.chc.2016.12.013
-
Zablotsky B, Rast J, Bramlett MD, Shattuck PT. Health care transition planning among youth with ASD and other mental, behavioral, and developmental disorders.
Matern Child Health J. 2020;24(6):796-804.
doi:10.1007/s10995-019-02858-6
-
Hyman SL, Levy SE, Myers SM, et al; Council on Children With Disabilities, Section on Developmental and Behavioral Pediatrics. Identification, evaluation, and management of children with autism spectrum disorder.
Pediatrics. 2020;145(1):e20193447.
doi:10.1542/peds.2019-3447
-
-
Makaroff LA, Xierali IM, Petterson SM, Shipman SA, Puffer JC, Bazemore AW. Factors influencing family physicians’ contribution to the child health care workforce.
Ann Fam Med. 2014;12(5):427-431.
doi:10.1370/afm.1689
-
Antezana L, Scarpa A, Valdespino A, Albright J, Richey JA. Rural trends in diagnosis and services for autism spectrum disorder.
Front Psychol. 2017;8:590.
doi:10.3389/fpsyg.2017.00590
-
-
Austriaco K, Aban I, Willig J, Kong M. Contemporary trainee knowledge of autism: how prepared are our future providers?
Front Pediatr. 2019;7:165.
doi:10.3389/fped.2019.00165
-
Golnik A, Ireland M, Borowsky IW. Medical homes for children with autism: a physician survey.
Pediatrics. 2009;123(3):966-971.
doi:10.1542/peds.2008-1321
-
Zerbo O, Massolo ML, Qian Y, Croen LA. A study of physician knowledge and experience with autism in adults in a large integrated healthcare system.
J Autism Dev Disord. 2015;45(12):4,002-4,014.
doi:10.1007/s10803-015-2579-2
-
Bridgemohan C, Kaufman B, Johnson DM, Shulman LH, Zuckerman KE. Autism: Caring for Children With Autism Spectrum Disorders: A Practical Resource Toolkit for Clinicians. 3rd ed. American Academy of Pediatrics; 2019.
-
Daniel KL, Prue C, Taylor MK, Thomas J, Scales M. ‘Learn the signs. Act early’: a campaign to help every child reach his or her full potential.
Public Health. 2009;123(suppl 1):e11-e16.
doi:10.1016/j.puhe.2009.06.002
-
-
Major NE, Peacock G, Ruben W, Thomas J, Weitzman CC. Autism training in pediatric residency: evaluation of a case-based curriculum.
J Autism Dev Disord. 2013;43(5):1,171-1,177.
doi:10.1007/s10803-012-1662-1
-
Garg P, Lillystone D, Dossetor D, et al. A framework for developing a curriculum regarding autism spectrum disorders for primary care providers.
J Clin Diagn Res. 2015;9(10):SC01-SC06.
doi:10.7860/JCDR/2015/13248.6651
-
Seehusen DA, Mainous AG III, Chessman AW. Creating a centralized infrastructure to facilitate medical education research.
Ann Fam Med. 2018;16(3):257-260.
doi:10.1370/afm.2228
-
Wood K, Giannopoulos V, Louie E, et al. The role of clinical champions in facilitating the use of evidence-based practice in drug and alcohol and mental health settings: a systematic review.
Implement Res Pract. 2020;1:2633489520959072.
doi:10.1177/2633489520959072
-
Donovan M, VanDerKolk K, Graves L, McKinney VR, Everard KM, Kamugisha EL. Gender-affirming care curriculum in family medicine residencies: a CERA study.
Fam Med. 2021;53(9):779-785.
doi:10.22454/FamMed.2021.764850
-
Sohl K, Rynkiewicz A, Nanclares-Nogués V, et al. Project Extension for Community Health Outcomes (ECHO) Autism: a successful model to increase capacity in community-based care.
Brain Sci. 2022;12(3):327.
doi:10.3390/brainsci12030327
-
Osei-Twum J-A, Wiles B, Killackey T, Mahood Q, Lalloo C, Stinson JN. Impact of Project ECHO on patient and community health outcomes: a scoping review.
Acad Med. 2022;97(9):1,393-1,402.
doi:10.1097/ACM.0000000000004749
-
Mazurek MO, Stobbe G, Loftin R, et al. ECHO Autism transition: enhancing healthcare for adolescents and young adults with autism spectrum disorder.
Autism. 2020;24(3):633-644.
doi:10.1177/1362361319879616
-
Hand BN, Coury DL, Darragh AR, et al. Patient and caregiver experiences at a specialized primary care center for autistic adults.
J Comp Eff Res. 2020;9(16):1,131-1,140.
doi:10.2217/cer-2020-0155
-
Kolomitro K, Graves L, Kirby F, et al. Developing a curriculum for addressing the opioid crisis: a national collaborative process.
J Med Educ Curric Dev. 2022;9:23821205221082913.
doi:10.1177/23821205221082913
-
Kalkbrenner AE, Daniels JL, Emch M, Morrissey J, Poole C, Chen J-C. Geographic access to health services and diagnosis with an autism spectrum disorder.
Ann Epidemiol. 2011;21(4):304-310.
doi:10.1016/j.annepidem.2010.11.010
-
Turner A, Ricketts T, Leslie LK. Comparison of number and geographic distribution of pediatric subspecialists and patient proximity to specialized care in the US between 2003 and 2019.
JAMA Pediatr. 2020;174(9):852-860.
doi:10.1001/jamapediatrics.2020.1124



There are no comments for this article.