Background and Objectives: Patient navigation programs help guide vulnerable populations, such as those experiencing homelessness, through the health care system. Medical students developed the student-run Patient Navigator Program (PNP) to serve persons experiencing homelessness (PEH) in the Dallas area. The objective of this study was to build on previously published data to determine how medical student attitudes, knowledge, and confidence working with PEH changed during involvement in the PNP, particularly after participating as a patient navigator.
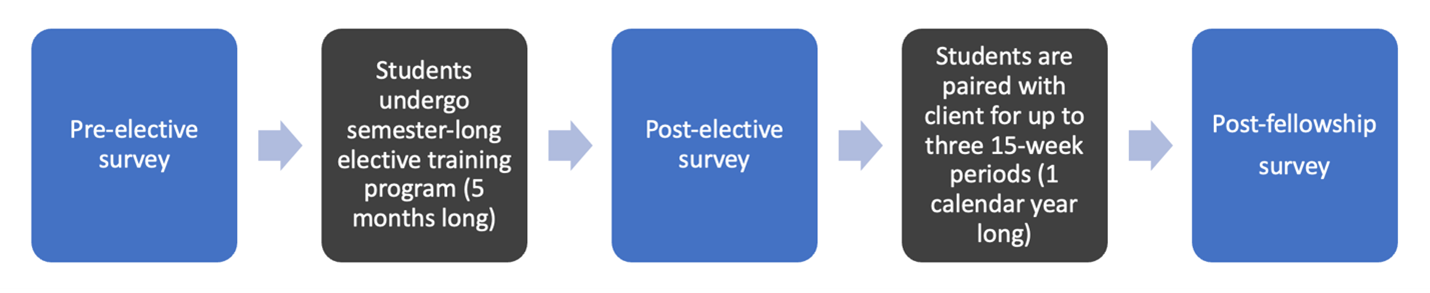
Methods: Student fellows completed a survey prior to a training elective (time point 1), immediately after the training elective (time point 2), and after acting as a patient navigator (time point 3). The PNP survey, which intended to measure student attitudes and knowledge regarding PEH, included the Health Professionals’ Attitudes Toward the Homeless Inventory (HPATHI) and the Student-Run Free Clinic Project (SRFCP) surveys. In our analysis, we compared responses among the different time points.
Results: Seventy-six of 88 students who completed the training elective chose to participate in the PNP fellowship. Skills, knowledge, and self-efficacy improved from time points 1 to 2, 1 to 3, and 2 to 3. Social advocacy also improved from time points 1 to 2 and 1 to 3.
Conclusions: Improvements from time point 1 to 2 demonstrated the value of didactic learning, while further improvements from time point 2 to 3 demonstrated the added benefit of hands-on experiential learning. Our study illustrates the potential educational benefits that a PNP provides to medical students who may encounter or care for this population during their careers.
In traversing the complex health care system, medical providers have used patient navigation programs to assist vulnerable populations, specifically those medically underserved or experiencing health disparities.1 Patient navigators provide relevant guidance needed to make appointments, secure funding, and fill out necessary paperwork—all of which can be daunting for those with minimal health care familiarity. Navigation-based interventions increase the use of primary care and screening, and reduce emergency/acute care usage and overall hospital costs. 1
Persons experiencing homelessness (PEH) face significant structural barriers to health care access and must balance competing/relative priorities related to food, income, and shelter. 2 On any given night, the Dallas–Fort Worth (DFW) area has an estimated 4,410 PEH, many of whom need identification documents, more thorough medical care, reliable housing, and other social services. 3 To meet the needs of PEH in DFW, medical students established the student-run Patient Navigator Program (PNP), which began as a training elective course on the experiences of PEH. 4 Subsequently, the PNP fellowship was developed to improve the health and well-being of PEH in Dallas by pairing them with student navigators who connect them with available community resources. 4 To our knowledge, PNP is the only patient navigation program that is fully run by medical students and the only program involving medical students with PEH.5-7 While impact of the PNP training elective has been studied previously, an understanding of how participation as a patient navigator impacts student navigators is lacking. 4 The purpose of this study was to build on previously published data and determine how medical students’ attitudes, knowledge, and confidence working with PEH have changed during their involvement in PNP, particularly after experiential involvement as a patient navigator.
Prior to volunteering, students take a semester-long course educating them about the barriers faced by PEH and available resources.4 The fellowship is structured as teams of three to five student navigators serving clients for three 15-week cycles during a calendar year. Each team and their client establish five to six SMART goals to achieve over the course of the cycle. Typical goals include obtaining identification, procuring public transit passes, setting up medical appointments, exploring affordable options for medications, and applying for the medical charity program of a Dallas County hospital.
Student fellows complete an anonymous REDCap (Vanderbilt University) survey at three points during their involvement with the PNP: prior to the training elective (time point 1), after the training elective (time point 2), and after the fellowship year (time point 3) (Figure 1). Along with questions on demographics and interest working with different populations, the survey includes the Health Professionals’ Attitudes Toward the Homeless Inventory (HPATHI) and Student-Run Free Clinic Project (SRFCP) surveys.8-10 The HPATHI survey consists of 19 items categorized into three attributes: social advocacy, personal advocacy, and cynicism.9 The SRFCP survey consists of 15 items, 13 of which are categorized into four attributes: knowledge, skills, attitudes, and self-efficacy.10 The remaining two items represent “interest working with the underserved” and “interest in primary care." 10 All HPATHI and SRFCP scores are out of 5 and 7, respectively, with higher scores representing higher self-perceived abilities.
A previous study investigated the impact of the semester-long training elective on a student cohort from one year.4 Our study included the previous study’s data as well as additional data from that cohort following the fellowship and another full-year’s cohort data. This study has been approved by the University of Texas Southwestern Medical Center Institutional Review Board.
We conducted two-tailed paired t tests, Wilcoxon signed rank tests, and two proportion z tests between survey time points to investigate changes in attitudes and knowledge. The α value was set at 0.05, and P values <.05 were considered significant.
Student Characteristics
A total of 88 student navigators completed the training elective: 46 navigators (52.3%) in the 2020 cohort and 42 navigators (47.7%) in the 2021 cohort. Forty-two of 46 students (91.3%) in the 2020 cohort opted to serve as fellows, while 34 of 42 students (81.0%) in the 2021 cohort opted to serve. Characteristics of student participants are highlighted in Table 1 .
|
Demographics (N=88)
|
n (%)
|
|
Age (Years)
|
|
|
≤21
|
6 (6.8)
|
|
22-25
|
74 (84.1)
|
|
≥26
|
8 (9.1)
|
|
Gender
|
|
|
Cisgender woman
|
62 (70.5)
|
|
Cisgender man
|
23 (26.1)
|
|
Other (transgender, nonbinary, prefer not to answer)
|
3 (3.4)
|
|
Race/ethnicity*
|
|
|
Non-Hispanic White
|
33 (37.5)
|
|
Hispanic, Latino, Spanish origin
|
5 (5.7)
|
|
Black/African American
|
3 (3.4)
|
|
Asian
|
48 (54.5)
|
|
American Indian or Alaskan Native
|
1 (1.1)
|
|
Middle Eastern or North African
|
4 (4.5)
|
|
Prefer not to answer
|
4 (4.5)
|
|
Average family income
|
|
|
$20,000 to $50,000
|
14 (15.9)
|
|
$50,001 to $100,000
|
16 (18.2)
|
|
$100,000 or more
|
49 (55.7)
|
|
Do not know/prefer not to answer
|
11 (12.5)
|
|
Personal experience with homelessness
|
|
|
Yes
|
4 (4.5)
|
|
No
|
83 (94.3)
|
|
Unsure
|
1 (1.1)
|
|
Prior experience working with persons experiencing homelessness
|
|
|
None
|
28 (31.8)
|
|
<1 year
|
42 (47.7)
|
|
1–3 years
|
15 (17)
|
|
>3 years
|
3 (3.4)
|
Survey Results
Of the total 88 navigators across both cohorts, 53 individuals completed both the preelective and postelective surveys, 40 individuals completed both the preelective and postfellowship surveys, and 17 individuals completed both the postelective and postfellowship surveys. Survey category measures that changed between different time points are presented in Table 2 . Social advocacy, skills, knowledge, self-efficacy, and attitudes all significantly improved between time points. However, all the attributes concerning interest working with different populations and in primary care had nonsignificant increases from time point 1 to 3. All other unmentioned attributes were found to have nonsignificant changes.
|
Survey
|
Metric
|
Time points
|
Mean initial value
|
Mean final value
|
P value
|
|
HPATHI
|
Social advocacy
|
1 to 2
|
4.239
|
4.440
|
<.001
|
|
HPATHI
|
Personal advocacy
|
1 to 2
|
3.948
|
3.996
|
.186
|
|
HPATHI
|
Cynicism
|
1 to 2
|
2.750
|
2.684
|
.448
|
|
SRFCP
|
Attitudes
|
1 to 2
|
6.283
|
6.443
|
.091
|
|
SRFCP
|
Skills
|
1 to 2
|
2.840
|
4.170
|
<.001
|
|
SRFCP
|
Knowledge
|
1 to 2
|
3.382
|
4.646
|
<.001
|
|
SRFCP
|
Self-efficacy
|
1 to 2
|
4.657
|
5.438
|
<.001
|
|
HPATHI
|
Social advocacy
|
1 to 3
|
4.325
|
4.558
|
<.001
|
|
HPATHI
|
Personal advocacy
|
1 to 3
|
3.922
|
4.011
|
.093
|
|
HPATHI
|
Cynicism
|
1 to 3
|
2.681
|
2.544
|
.170
|
|
SRFCP
|
Attitudes
|
1 to 3
|
6.150
|
6.600
|
.007
|
|
SRFCP
|
Skills
|
1 to 3
|
2.975
|
5.075
|
<.001
|
|
SRFCP
|
Knowledge
|
1 to 3
|
3.406
|
4.963
|
<.001
|
|
SRFCP
|
Self-efficacy
|
1 to 3
|
4.870
|
5.895
|
<.001
|
|
HPATHI
|
Social advocacy
|
2 to 3
|
4.431
|
4.588
|
.152
|
|
HPATHI
|
Personal advocacy
|
2 to 3
|
3.974
|
4.059
|
.291
|
|
HPATHI
|
Cynicism
|
2 to 3
|
2.471
|
2.618
|
.436
|
|
SRFCP
|
Attitudes
|
2 to 3
|
6.412
|
6.588
|
.105
|
|
SRFCP
|
Skills
|
2 to 3
|
4.294
|
5.324
|
.005
|
|
SRFCP
|
Knowledge
|
2 to 3
|
4.647
|
5.044
|
.015
|
|
SRFCP
|
Self-efficacy
|
2 to 3
|
5.388
|
5.929
|
.041
|
|
SRFCP
|
Interest working with the underserved
|
1 to 3
|
5.850
|
5.925
|
.637
|
|
SRFCP
|
Interest in primary care
|
1 to 3
|
4.158
|
4.421
|
.230
|
|
|
Interest in working with PEH
|
1 to 3
|
55.7%*
|
73%*
|
.058
|
|
|
Interest working with low-income individuals
|
1 to 3
|
73.9%*
|
77.5%*
|
.832
|
|
|
Interest working with racial/ethnic minorities
|
1 to 3
|
75%*
|
78%*
|
.706
|
Results of our assessments suggest that completion of the training elective and hands-on fellowship corresponded with increased students’ self-perceived ability, specifically in the skills, knowledge, and self-efficacy categories, to work with this population. We found the greatest improvements in self-perceived ability between the first and second time points, suggesting the utility of the elective training program in equipping students with adequate confidence and knowledge to begin working with PEH. Additionally, scores in these categories also improved between the second and third time points, suggesting that hands-on experience may further enhance students’ self-perceived ability to work with PEH.
Given that students volunteer to join the student-run Patient Navigator Program, the lack of significant improvement in students’ interest working with these populations, interest working in primary care, and HPATHI categories (ie, personal advocacy and cynicism) between time points may be attributable to preexisting strong interest in working with underserved populations.
While limited literature exists on the impact of patient navigation programs on medical students’ abilities, our findings are consistent with studies investigating the impact of medical student involvement in student-run free clinics on self-perceived knowledge, skills, self-efficacy, and attitudes, indicating the potential general benefit from hands-on experience and direct contact with underserved populations. 9 However, our findings contrasted with those from a study centered around a student-run free clinic for PEH, in which social advocacy, as measured by the HPATHI, did not improve. 10 More intimate exposure as a patient navigator to the social barriers PEH face, as opposed to interaction limited to the clinic, may encourage increased perception of society’s responsibility to care for this population.
Limitations of our study included survey loss to follow-up, which we addressed by aggregating data points from multiple cohorts over time. However, even with this aggregation, the sample size was only 17 when comparing time points 2 and 3, limiting the power of our statistical analyses. Two interventions improved response rate and could be used in the future: (a) allotting dedicated time to fill out the survey during a mandatory meeting, and (b) entering students into a raffle to win a gift card following completion. Another limitation was the slight modifications made to the training elective, which could have made learning inconsistent between years.
Future work includes evaluating student navigators’ career choices and gathering student learner perspectives for program improvement. Overall, we found that medical students’ self-perceived ability and knowledge related to working with PEH were increased following the PNP elective training course and hands-on patient navigator experience. We hope that this work will result in greater numbers of students eventually serving PEH, which would be the ultimate assessment of the PNP’s educational efficacy.
Acknowledgments
We thank all those at the Union of Gospel Mission shelters for their partnership and assistance through the years, without whom the PNP would not be possible.
References
-
-
Carmichael C, Smith L, Aldasoro E, et al. Exploring the application of the navigation model with people experiencing homelessness: a scoping review.
J Soc Distress Homeless. 2022;1-15.
doi:10.1080/10530789.2021.2021363
-
-
Liu A, Suarez A, Kak A, et al. Training students as navigators for patients experiencing homelessness.
Fam Med. 2023;55(1):45-50.
doi:10.22454/FamMed.55.143409
-
Qua K, Gullett H, Wilson-Delfosse A, Thomas P, Singh M. Early medical students’ experiences as system navigators: results of a qualitative study.
J Gen Intern Med. 2022;37(5):1,155-1,160.
doi:10.1007/s11606-021-07168-8
-
Gonzalo JD, Wolpaw D, Graaf D, Thompson BM. Educating patient-centered, systems-aware physicians: a qualitative analysis of medical student perceptions of value-added clinical systems learning roles.
BMC Med Educ. 2018;18(1):248.
doi:10.1186/s12909-018-1345-5
-
Henry-Tillman R, Deloney LA, Savidge M, Graham CJ, Klimberg VS. The medical student as patient navigator as an approach to teaching empathy.
Am J Surg. 2002;183(6):659-662.
doi:10.1016/S0002-9610(02)00867-X
-
Buck DS, Monteiro FM, Kneuper S, et al. Design and validation of the Health Professionals’ Attitudes Toward the Homeless Inventory (HPATHI).
BMC Med Educ. 2005;5(1):2.
doi:10.1186/1472-6920-5-2
-
Smith SD, Yoon R, Johnson ML, Natarajan L, Beck E. The effect of involvement in a student-run free clinic project on attitudes toward the underserved and interest in primary care.
J Health Care Poor Underserved. 2014;25(2):877-889.
doi:10.1353/hpu.2014.0083
-
Mercadante SF, Goldberg LA, Divakaruni VL, Erwin R, Savoy M, O’Gurek D. Impact of student-run clinics on students’ attitudes toward people experiencing homelessness.
PRiMER. 2021;5:19.
doi:10.22454/PRiMER.2021.489756



There are no comments for this article.