There is a story that may or may not have been fully true, yet teaches an exquisite lesson. The lesson is those who survive transitions in a dysfunctional system may have less to teach us about improving the system than those who do not survive.
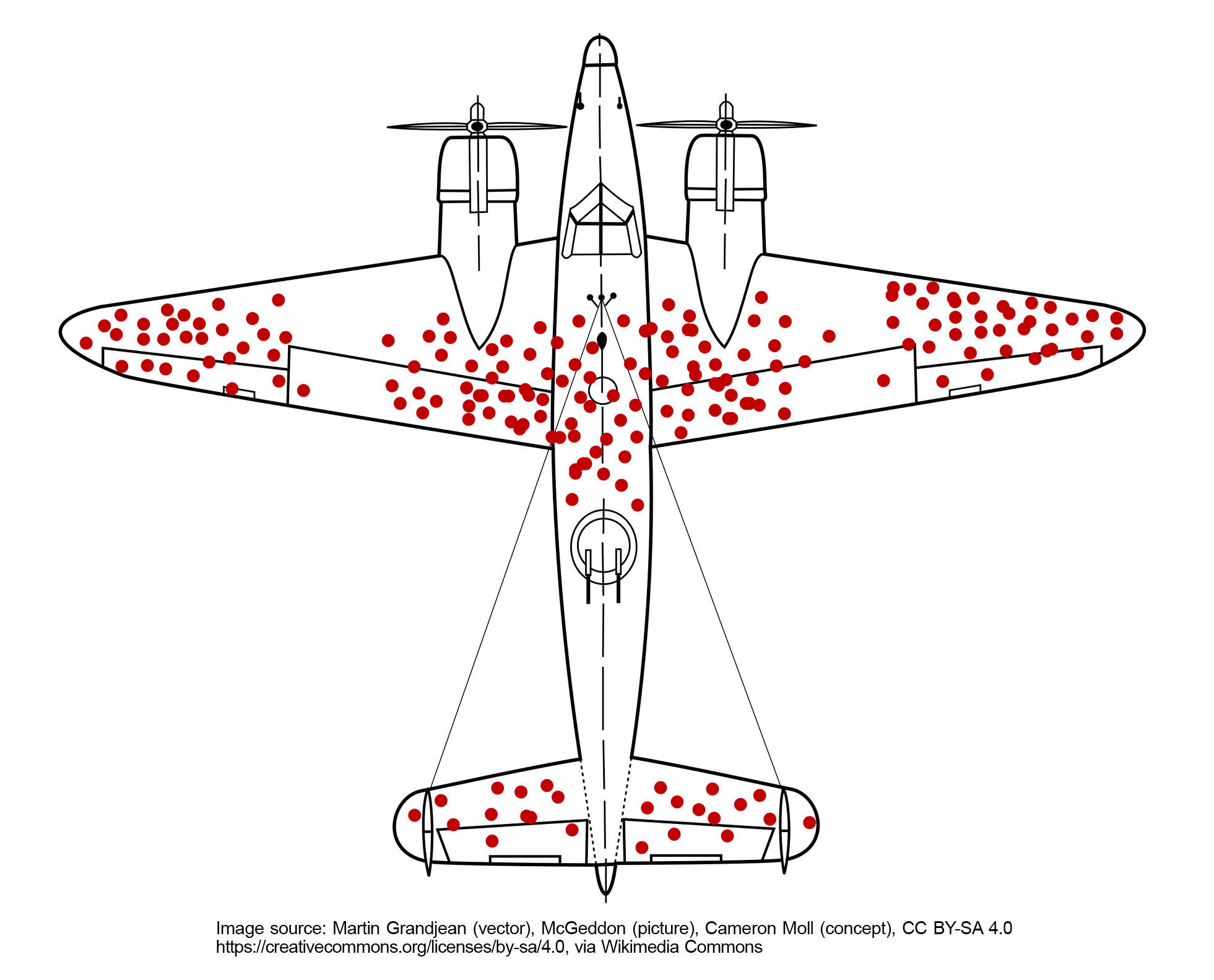
The story is set in World War II, when evaluating fighter planes that had returned from air battles and deciding where to put more armor, only one engineer was able to identify the impact of survivor bias on the options that were being proposed. Models were shown, demonstrating a composite of every location where a bullet hole was found on the returning planes (Figure 1). This model was used in discussions about putting armor where it was clear that the plane had been shot. Apparently only one engineer noted that those were the surviving planes; the planes that did not survive were the ones hit in areas that were not shown on the model. The pattern of bullets on surviving planes demonstrated areas where, if shot, the plane could still fly back to the base. If a plane was shot in other areas, it was less likely to return to the base. This story has long been trotted out as the hallmark example of survivor bias, and how it impacts decision making. Returning to base is a success, and if we want to make more people successful we need to create more paths to success, not simply reinforce the known paths.
Reinforcing known paths is a huge part of what we have done in medical education in search of the “best and brightest,” which is clearly a euphemism for those who can teach themselves and are therefore the easiest to teach in our massively dysfunctional health care and educational system.
If we want to prepare the next generation of physicians to deal with the current and future state of health care, the old curriculum of telling the students what to memorize and then testing their memorization cannot be considered the cornerstone of teaching. It has failed and left many high-capacity, potential medical students and potential residents behind. We need more paths to successful learning if we want to grow more successful learners.
In preclinical years most students spend more time watching lectures on their laptops than in a room with faculty. In residencies how many programs do primarily case-based discussions in didactics? But still, our education process remains locked into a paradigm in which those who have power point at a screen, and those in the seats teach themselves what’s being pointed at. This lonely, high-pressure, high-stakes environment may also be a large contributor to the loss of so many medical students to suicide every year,1 a horrific consequence of our dysfunctional learning structures.
The current system has devastating results for individuals and society. For example, by any calculation, we can see we need more primary care physicians. These are critical thinkers who can engage ambiguity and guide comprehensive continuity care. Our current educational system plants few and harvests even fewer primary care-destined learners, which are exactly the type of physicians our health systems and patients desperately seek.
We are ready for a change, but we cannot change a problem with the same system that created the problem. Calculated disruption is needed. We need a thoughtful educational catastrophe. In the truest form of the original Greek word, catastrophe is from kata- “down” + strophē “turning,” or we can just call it a “flip.”
The necessity for a paradigm shift in medical education is both urgent and profound, calling for a transition from traditional pedagogical methods to a more dynamic and inclusive andragogical approach. This change represents not just a modification of teaching styles, but a fundamental re-evaluation of the very foundations of medical education.
Traditional pedagogy, with its focus on memorization, fails to address the needs of adult learners in medicine who bring a diversity of experiences and require an education that promotes critical thinking, practical application, and interactive learning.
Andragogy, in contrast, acknowledges and leverages the rich backgrounds and experiences of adult learners, creating an educational environment that is more relevant and effective for the complexities of the medical field. However, this transition is not without challenges. It requires a comprehensive reassessment and restructuring of the entrenched power dynamics within educational institutions, which have traditionally favored a hierarchical, top-down approach. Embracing this shift demands courage and a willingness to challenge and reshape these dynamics in favor of a more equitable, participatory, and effective educational environment.
The current landscape of medical education, often reliant on outdated methods of passive learning, is increasingly recognized as inadequate for adult learners.2 These learners require an educational framework that emphasizes the application, analysis, and synthesis of knowledge in real-world contexts. The transition from pedagogy to andragogy, therefore, is not just a change in terminology; it represents a profound transformation in how we conceive, deliver, and evaluate medical education.
Addressing the entrenched power structures that have upheld the status quo is critical. These structures, deeply rooted in tradition, have often resisted change, favoring a top-down approach. The future of medical education demands a willingness to challenge these dynamics, decentralize authority, and foster a culture of collaboration and inclusion. Such an approach democratizes the learning process and better prepares students for the collaborative nature of modern health care.
In this transformative journey, the integration of artificial intelligence (AI) in the curriculum may provide personalized preclass teaching. This prepares the ground for an andragogical, flipped classroom model where in-person case studies and critical thinking discussions are central. AI-driven preclass preparation could provide students with a tailored educational experience, which must be continually validated to ensure it is grounded in reliable information and free from fabricated references. With these safeguards, this methodological shift would be essential in fostering a deep understanding and critical engagement, which are crucial in the evolving health care landscape.
The flipped classroom model, supported by AI-driven preparation, may revolutionize the educational environment. Classroom time shifts from passive reception of information to active engagement with complex medical scenarios. This enables a deeper exploration of case studies, encouraging students to apply their preclass learning to practical, real-world contexts. The AI component, rigorously validated, ensures that the foundational knowledge provided is reliable, accurate, and continuously updated, reflecting the latest evidence and ethical considerations in medicine.
This transformation in medical education is not merely about technological integration; it is about nurturing a new paradigm of health care professionals. It is about preparing physicians who are not only knowledgeable, but also skilled in navigating the complexities of modern health care with confidence and competence. The focus is on developing critical thinkers and problem-solvers who can adapt to a rapidly-changing medical landscape.
However, the implementation of this advanced educational model requires careful consideration of resources and collaboration. It involves a synergistic effort among educators, technologists, and health care professionals to create a seamless and effective learning ecosystem. The challenge lies in ensuring that the AI component remains true to the subject matter, providing students with accurate, relevant, and trustworthy information. The scrutiny and validation of AI-driven content are paramount to maintaining the integrity of medical education and preventing the dissemination of erroneous or unverified information.
Integrating AI into medical education, particularly in preclass preparation, may usher in a new era in the training for health care professionals. Coupled with the flipped classroom model, this approach emphasizes deep understanding and critical engagement. It marks a journey toward creating a more dynamic, responsive, and critical thinking-focused medical education system. This transformation, while challenging, presents an opportunity realize a future where medical professionals are not only well-informed but also more equipped with the critical thinking skills necessary to excel in a rapidly evolving health care environment.
We can collectively embark on this transformative journey, redefining medical education for the betterment of health care and society. Institutions should consider prioritizing the development of AI-driven educational tools, ensuring their accuracy and relevance. Faculty must be supported in adopting the flipped classroom model, with resources allocated to the necessary training and development. Collaboration across disciplines is essential to create a cohesive and integrated educational system that aligns with the goals of modern medical education.
By embracing this paradigm shift, we can ensure a more dynamic, inclusive, and effective medical education system. When we create more paths to success we will achieve more success. Shall we merely see a few survive, or can new technologies and innovative approaches allow many to thrive? “Thriver bias?” Nah, we’ll have to call it something else.



There are no comments for this article.